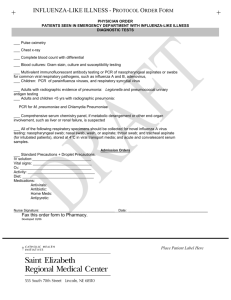
Respiratory-infections
advertisement

Respiratory infection - 1 Dr Paul McIntyre 1 Influenza - clinical presentation • Fever: high, abrupt onset • Malaise • Myalgia • Headache • Cough • Prostration 2 ‘Flu - aetiology • Classical flu – influenza A viruses – influenza B viruses • ‘Flu- like illnesses – parainfluenza viruses – many others • Haemophilus influenzae – bacterium – not a primary cause of ‘flu – may be a secondary invader 3 ‘Flu - complications • Primary influenzal pneumonia – seen most during pandemic years – can be disease of young adults – high mortality • Secondary bacterial pneumonia – more common in elderly and debilitated, preexisting disease – cause of mortality in all influenza epidemics 4 ‘Flu - therapy • Symptomatic – bed rest, fluids, paracetamol • Antivirals – oseltamivir – zanamivir • see NICE guidelines www.nice.org.uk – ‘flu circulating – risk of complications – use in prophylaxis (additional to vaccine) 5 Epidemiology of ‘flu • Winter epidemics • Epidemics seen in association with minor mutations in the surface proteins of the virus – antigenic drift • Pandemics: rare, unpredictable, influenza A – antigenic shift – segmented genome – animal reservoir/mixing vessel 6 Current pandemic planning assumption • the combination of “reasonable worst case” 30% Clinical Attack Rate and 0.1% Case Fatality Ratio would result in a total number of deaths of about 20,000, or about 1/30th of the total expected each year from all causes (about 600,000). • These are planning assumptions for forthcoming winter, not predictions 7 8 Comparison of H1N1 Swine Genotypes in Early Cases in the United States Novel Swine-Origin Influenza A (H1N1) Virus Investigation Team. N Engl J Med 2009;360:2605-2615 9 Future threats • Highly pathogenic avian flu is influenza A H5N1 • bird to human transmission seen – High mortality • not readily transmitted human to human 10 11 Egon Schiele,The Family,1918.Oesterreichische Galerie, Vienna Lab confirmation of influenza • Direct detection of virus – PCR • Throat swabs in virus transport medium • Pernasal swabs in virus transport medium • other respiratory samples – Other labs may use immunofluorescence, antigen detection (near patient), virus culture 12 Lab confirmation of influenza • Direct detection of virus – PCR • Antibody detection – may need paired acute and convalescent bloods – often retrospective 13 PCR for Influenza A Virus Influenza A RNA positive samples Influenza A RNA negative samples 14 Prevention of ‘flu • Vaccine – killed vaccine – given annually to patients at risk of complications – given to health care workers 15 Antiviral as prophylaxis • antivirals after a contact with ‘flu – NICE guidelines – rarely used • During “containment phase” of first wave of pandemic. 16 Other causes of community acquired pneumonia • Microbiological causes (all bacteria) – Mycoplasma pneumoniae – Coxiella burnetii – Chlamydia 17 Mycoplasma, coxiella and Chlamydophila psittaci • Therapy – all respond to tetracycline and macrolides (eg clarithromycin) • Mortality – varies with pathogen, but generally lower than classical bacterial pneumonia • Often known as “atypical pneumonia” – relates to presentation and response to therapy in the pre-antibiotic era 18 Lab confirmation of mycoplasma, coxiella and Chlamydophila psittaci • By serology – send acute and convalescent bloods to lab – gold top vacutainer 19 Mycoplasma pneumoniae • Common cause of community acquired pneumonia • Older children, young adults • Person to person spread 20 Coxiella burnetii (Q-fever) • Diseases – pneumonia – pyrexia of unknown origin (Q fever) • Uncommon, sporadic zoonosis • Sheep and goats • Complication – culture negative endocarditis 21 Chlamydia and respiratory disease • Chlamydophila psittaci causes Psittacosis – previously called Chlamydia psittaci – uncommon, sporadic zoonosis – caught from pet birds • parrots, budgies, cockatiels – psittacosis usually presents as pneumonia 22 Bronchiolitis • Clinical presentation – – – – – 1st or 2nd year of life Fever Coryza Cough Wheeze • Severe cases – grunting – PaO2 – Intercostal / sternal indrawing 23 Bronchiolitis - complications • Respiratory and cardiac failure – prematurity – pre-existing respiratory or cardiac disease • Scottish Intercollegiate Guidelines Network – SIGN guideline 91 24 Bronchiolitis • Aetiology – >90% cases due to Respiratory Syncytial Virus • Lab confirmation – By PCR on throat or pernasal swabs – (direct IF on NPA in some labs) • Therapy – supportive – nebulised ribavirin no longer used 25 Bronchiolitis - epidemiology and control • • • • Epidemics every winter Very common No vaccine Nosocomial spread in hospital wards – cohort nursing – handwashing, gowns, gloves • Passive immunisation – poor efficacy and cost-effectiveness 26 Metapneumovirus • First isolated 2001 children with Acute Respiratory Tract Infection – Nat Med 2001;7:719-24. 27 Epidemiology • • • • • Most children antibody positive by age 5 found in a wide range of ages Virus is newly discovered, not new World-wide distribution Highest incidence in winter – 8% of samples in Canadian children’s hospital – J Clin Micro 2005;43:5520-5. 28 Association with disease • • • • • May be sole pathogen isolated Possibly second only to RSV in bronchiolitis Similar symptoms to RSV in both children and adults Range of severity from mild to requiring ventilation Incidence of asymptomatic infection low (in children at least) – Williams JV et al. NEJM 2004;350:443-50 (and editorial) • 2% of cases of influenza-like illness – Emerging Infect Dis 2002;8:897-901 29 Laboratory confirmation • PCR 30 Other recently discovered respiratory viruses • Bocavirus • Various coronaviruses 31 Current Respiratory tests • Samples for PCR: Throat swabs in viral transport medium, bronchoalveolar lavage (BAL), endotracheal aspirate etc – Flu A, Flu B, parainfluenza 1-3, metapneumo, adeno, RSV 32 Chlamydia trachomatis and Chlamydophila pneumoniae and respiratory disease • Chlamydia trachomatis – STI which can cause infantile pneumonia – diagnosed by PCR on urine of mother or pernasal / throat swabs of child • Chlamydophila pneumoniae – person to person (formerly Chlamydia pneumoniae) – mostly mild respiratory infections – may be picked up by test for Psittacosis 33 Microbiology Problem Solving Session • Remember to bring the relevant pages from the study guide with you to the class. • Code for the classroom’s cloakroom is 1245 • Worthwhile looking at tuberculosis diagnosis and management before coming along. • Remember to wash your hands before leaving the classroom as other students use live bacteria in their practicals in that room. 34 Lecture objectives • An understanding of the epidemiology, presentation, management and prevention of many of the most important viral and “atypical” causes of respiratory infection. 35