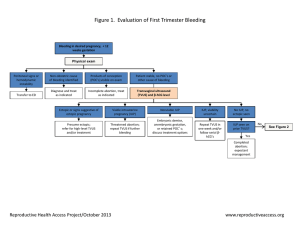
Evaluation and management of complications of first trimester
advertisement

ACEP clinical policy: complications of early pregnancy sigrid hahn, MD MPH mount sinai school of medicine, NY NY disclosures none 2012 update applies to stable patients in the first trimester with abdominal pain or vaginal bleeding does not apply to patients with vital sign instability, infertility treatment (at high risk for heterotopic pregnancy), other presenting complaints what is your “rule out ectopic” algorithm? 27 y/o F G1P0 LMP 5 weeks ago β hCG 1950 mIU/mL no IUP seen on bedside pelvic US a) repeat bedside US and attempt to visualize adnexa b) get a stat comprehensive US c) get a comprehensive US ASAP c) consult OB d) d/c with 48 hour follow up 27 y/o F G1P0 LMP 5 weeks ago β hCG 950 mIU/mL no IUP seen on bedside pelvic US a) repeat bedside US and attempt to visualize adnexa b) get a stat comprehensive US c) get a comprehensive US ASAP c) consult OB d) d/c with 48 hour follow up classic “rule out” ectopic algorithm BhcG β hCG >1500 β hCG <1500 mIU/mL 48 hour f/u US IUP Condous. BJOG. 112: 827-29. 2005 possible or proven ectopic mIU/mL classic algorithm grew out of the concept of the discriminatory zone sensitivity of pelvic US for IUP nears100% β hCG 1000 - 2000 mIU/mL IUP may be present but not yet visible classic algorithm is based on several false assumptions The beta and the discriminatory zone should help guide your evaluation and disposition The beta and the discriminatory zone should help guide your evaluation and disposition the very concept of the discriminatory zone has been challenged positive LR 0.8 (95CI 0.5 to 1.4) negative LR 1.1 (95CI 0.8 to 1.5) Wang. Ann Emerg Med. 2011; 58:12-20 Wang. Ann Emerg Med. 2011; 58:12-20 IUPs that would be misdiagnosed as abnormal or ectopic pregnancies β hCG (mIU/mL) patients with empty uterus on comprehensive US and final diagnosis of IUP 1000 - 1499 19 1500 -1999 12 > 2000 9 Doubliet. J Ultrasound Med 2011; 30:1637–1642 classic “rule out” ectopic algorithm BhcG β hCG >1500 β hCG <1500 mIU/mL 48 hour f/u US IUP Condous. BJOG. 112: 827-29. 2005 possible or proven ectopic mIU/mL You’re unlikely to see something if the bhCG is low anyway about 50% of IUPs will be diagnosed when the β hCG < 1000 mIu/mL http://www.acep.org/WorkArea/DownloadAsset.aspx?id=32886 about 50% of ectopics will have a suggestive or diagnostic US when the β hCG < 1000 mIu/mL http://www.acep.org/WorkArea/DownloadAsset.aspx?id=32886 Isn’t it unlikely that the patient will have an ectopic with a bhCG below the discriminatory zone, anyway? no ectopics often have lower β hCGs than IUPs mean EP mean IUP 1886 mIU/mL 30,512 mIU/mL Kohn. Academic Emergency Medicine. 2003. 10(2) Well, isn’t the risk of rupture of an ectopic pregnancy low if the bhCG is low? no rupture has been reported at 10 mIU/mL and 189,720 mIU/mL Barnhart. Obstetrics and Gynecology. 1994. 84(6) classic “rule out” algorithm US >1500 mIU/mL < 1500 mIU/mL 48 hour f/u US IUP Condous. BJOG. 112: 827-29. 2005 presumed or proven ectopic are there studies showing harm with the deferred ultrasound approach? no high quality studies have looked at harm • 37 patients had no deaths or hemodynamic instability despite d/c and median wait of 14 hours for US * • 69 patients had a mean delay of 5.2 days to diagnosis of ectopic with no deaths ** * Hendry JN, Naidoo Y. Emerg Med. 2001;13:338-343. ** Barnhart et al. Obstet Gynecol. 1994;84:1010-1015. ACEP clinical policy 2012 Should the emergency physician obtain a pelvic ultrasound in a clinically stable pregnant patient who presents to the ED with pelvic pain and/or vaginal bleeding and a βhCG below any discriminatory threshold? Level C recommendation: Perform or obtain a pelvic ultrasound for symptomatic pregnant patients with a β-hCG below any discriminatory threshold back to the case modern “rule out” ectopic algorithm US β hCG pending normal or suggestive 48 hour or abnormal US f/ indeterminat IUP, diagnositic e molar of ectopic IUP Condous. BJOG. 112: 827-29. 2005 what if you saw this? or this? what do you do with an indeterminate US, or a pregnancy of unknown location? ACEP clinical policy 2012 In patients who have an indeterminate transvaginal ultrasound, what is the diagnostic utility of β-hCG for identifying possible ectopic pregnancy? risk of ectopic pregnancy with indeterminate US β-hCG Threshold 1,000 mIU/mL 1,500 mIU/mL 2,000 mIU/mL 3,000 mIU/mL Relative Risk of Ectopic Below Threshold* (95%CI) Study Author Year Likelihood Ratios (95%CI) Class N Condous28 2005 II 527 Dart24 2002 II 635 0.6 (0.3 – 1.1) 7.1 (3.4 14.9) Kaplan3 1996 II 72 3.8 (1.4 - 9.8) Mol32 1998 II 262 0.4 (0.2 - 0.5) Dart35 1998 III 220 2.2 (1.0 - 4.5) Negative† 0.9 (0.8 1.0) 2.3 (1.9 2.7) 2.5 (1.4 4.5) 0.7 (0.5 0.8) 1.8 (1.1 – 2.9) 0.4 (0.2 – 0.9) 0.9 (0.8 – 1.0) 2.3 (1.1 – 4.9) 0.9 (0.8 – 1.0) 0.6 (0.5 – 0.8) 0.8 (0.5 1.3) 0.7 (0.5 0.9) 2.3 (0.9 – 5.7) Condous 28 Condous 28 2005 II 527 2005 II 527 0.5 (0.2 – 1.1) Mol32 1998 II 262 0.2 (0.1 - 0.3) Mateer26 1995 III 41 0.6 (0.2 - 1.4) Mateer33 1996 III 95 0.5 (0.3 - 0.8) Wang 27 Dart34 2011 II 141 1.3 (0.6 - 2.6) 1997 III 194 2.1 (0.9 - 4.8) 1.1 (0.8 – 1.5) 1.4 (1.0 – 1.8) Positive‡ 1.7 (0.9 – 3.1) 0.3 (0.2 – 0.5) 0.5 (0.2 – 0.9) 3.1 (2.0 - 4.8) 0.7 (0.5 - 1.0) 25 (7.9 – 81) 1.8 (0.7 - 4.8) 2.3 (1.2 - 4.3) 0.8 (0.5 - 1.4) 0.6 (0.3 - 1.1) ACEP clinical policy 2012 In patients who have an indeterminate transvaginal ultrasound, what is the diagnostic utility of β-hCG for identifying possible ectopic pregnancy? Answer: Diagnostic utility is poor Level C recommendation: Obtain specialty consultation or arrange close outpatient follow up for all patients with an indeterminate pelvic ultrasound what other ways can we risk stratify patients with indeterminate US (regardless of β hcG)? excluded IUP: yolk sac or fetal pole excluded EP: ectopic gestational sac, complex mass discrete from ovary, any echogenic fluid, moderate anechoic fluid art and Howard. Acad Emerg Med. 1998. 5:313-319. excluded IUP: yolk sac or fetal pole excluded EP: ectopic gestational sac, complex mass discrete from ovary, any echogenic fluid, moderate anechoic fluid art and Howard. Acad Emerg Med. 1998. 5:313-319. spectrogram of diagnostic certainty Small to nonmoderate specific anechoic nothing in intrauterine free fluid the uterus debris/sac, or or adnexa no adnexal nonmass specific nonadnexal ectopic specific nothing in mass IUP pregnanc intrauterine the uterus y debris/sac Indeterminate US evaluation and disposition ends up being determined by your gestalt based on patient’s clinical (and social) state, hospital and clinic system patient was sent home, and returns 2 days later… I passed a lot of tissue at home β hCG 1140 mIU/mL I think she completed. She passed POC at home and there’s just echogenic material in the uterus on ultrasound. 6% of patients with a suspected “complete miscarriage” had an ectopic pregnancy 152 patients with clinically suspected “complete miscarriage ” US with empty uterus Mean β hCG of 524 mIU/ml 94% complete 6% ectopic It’s not complete until the βhCG is 0 Condous. BJOG. 112: 827-29. 2005 Rhogam http://www.acep.org/WorkArea/DownloadAsset.aspx?id=32886 90% of alloimmunization occurs at delivery ACOG concluded that alloimmunization is exceedingly rare after threatened ABs in first trimester Higher rates of fetomaternal hemorrhage with complete AB compared with threatened AB Rhogam http://www.acep.org/WorkArea/DownloadAsset.aspx?id=32886 In patients receiving methotrexate for confirmed or suspected ectopic pregnancy, what are the implications for ED management? • MTX is relatively contraindicated in patients with an ectopic gestational sac larger than 3.5 cm or with embryonic cardiac motion seen on US • Treatment success rates are lower in patients who have a β-hCG of 5,000 mIU/L or more • Often need repeat dosing until β-hCG is decreasing • Best estimates of failure rates appx 10% • Rupture reported to range from 0.5 – 19%, probably < 5% In patients receiving methotrexate for confirmed or suspected ectopic pregnancy, what are the implications for ED management? (1) Arrange outpatient follow-up for patients who receive methotrexate therapy in the ED for a confirmed or suspected ectopic pregnancy (2) Strongly consider ruptured ectopic pregnancy in the differential diagnosis of patients who have received methotrexate and present with concerning signs or symptoms 1) don’t consider low β hCG low risk 2) consider a pelvic US for patients with any β hCG 3) your approach to the patient with a low β hCG will be determined by your US skills, comprehensive US availability, department protocol, clinical risk factors and findings 4) your approach to the patient with a PUL will also be determined by US skills, hospital protocols and resources, clinical risk factors and findings 5) a miscarriage is not complete until it’s complete 6) you probably don’t need to give rhogam for threatened AB 7) consider rupture in symptomatic patients s/p MTX