Fluid Balance in CHF Patients
advertisement

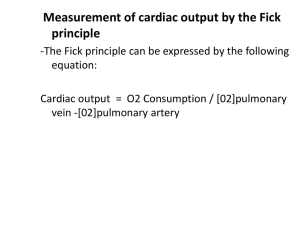
Maintaining Fluid Balance In Patients with Heart Failure Sarah Carek, RN, MSN Student Alverno College Spring 2010 What should I know by the end of this tutorial? • Understand the basic physiology of the heart. • Develop a clear picture as to how Heart Failure is a pathological process. • Recognize how excess fluid volume can result from Heart Failure. • Apply nursing interventions to patients with Heart Failure. • Examine how aging, stress, inflammation and genetics play in the development of Heart Failure. Tutorial Navigation • Click to advance to the next slide. • Click to go to the previous slide • All buttons will be on the bottom of each page. • Begin the tutorial by clicking on the first topic on the home page. Slides with Animation • FYI..many slides contain animation. Keep clicking the mouse to advance through the entire animation. If you hover your cursor over areas and it changes from an arrow to a hand…click and animation will occur. • Any underlined words have definitions available. Hover your cursor over the word and the definition will appear. Home Page Cardiac Physiology Pathophysiology of Heart Failure Causes of Heart Failure Important Nursing Interventions Fresh and New: Aging, Stress, Inflammation & Genetics References Contact Information CARDIAC PHYSIOLOGY Microsoft Clipart (manually altered) Let’s see what you know already! Hover your mouse cursor over each section of the heart until the cursor turns from an arrow to a hand. Then click to reveal its label. **If the mouse has not turned from an arrow to a hand..Do Not Click*** Aorta Pulmonary Arteries Pulmonary Veins Superior Vena Cava Left Atrium Right Atrium Left Ventricle Right Ventricle Inferior Vena Cava Microsoft Clipart (manually altered) What do the areas of the heart do? Click on the boxes to the left to find their function. Right Atrium Pumps deoxygenated blood from the body into the right ventricle. Right Ventricle Pumps deoxygenated blood to the lungs to get oxygenated. Left Atrium Receives oxygenated blood from the lungs and pumps it to the left ventricle. Left Ventricle Pumps oxygenated blood to the body to get used for energy Normal Blood Flow Microsoft Clipart (manually altered) What about the valves? The valves of the heart assure that blood flows in the right direction. Click on the diagram to find the four valves. They are half-moon shaped. Again when the cursor turns into a hand, it means you can click on it. Pulmonic Valve Aortic Valve Mitral Tricuspid (Bicuspid) Valve Valve Microsoft Clipart (manually altered) The Cardiac Cycle Click on the boxes on the left to find their definition. Microsoft Clipart Microsoft Clipart (manually altered) Systole The period during the cardiac cycle where the ventricles are contracting and moving the blood forward. Diastole The period during the cardiac cycle where the ventricles are relaxed and filling with new blood. (Porth & Matfin, 2009) The Heart as a Pump Cardiac Ouput Stroke Volume Heart Rate • Cardiac output measures how well the heart is doing its job of pumping blood to the body. • The heart has the ability to adjust cardiac output based on the body’s needs (i.e. exercise, sleep, illness). This depends on preload, afterload, cardiac contractility and heart rate. • Average cardiac output = 3.5 – 8 Liters/minute (Porth & Matfin, 2009) Keep clicking to advance through the animation of the slide. End-Diastolic Volume Starling’s Law Stretching of Cardiac Muscle Force of Contraction FYI: The fibers only stretch so far. There is a maximum force of contraction that can be achieved. The more blood in the heart at the end of diastole… The more the cardiac muscle fibers stretch… The greater the force of the contraction. (Porth & Matfin, 2009) Let’s Review Right Try Again! Atrium Left Excellent! Ventricle Left Close! Atrium No…but you are Right Ventricle on the right track. To prevent blood from Try Again! moving forward. To let air escape preventing Nope.an air embolus. To keep blood You’re Right! moving forward. To prevent blood from Keep leaking Trying! out of the heart. A. CO = HR x AV Incorrect B. CO = SV x HR Good Job! C. CO = AV x SV Try Again! D. CO = HR x EF Nope A. Blood Viscosity does not help the heart increase Blood Viscosity cardiac output. In order to increase cardiac output the heart B. Correct! Cardiac Contractility must be able to change the force of contraction. C. Yes! The heart can change its rate in order to Heart Rateor decrease cardiac output. increase Good Job! According to Starling’s Law, if End-Diastolic Volume D. Preload (preload) increases, the force of contraction will as well. E. Excellent! Cardiac output can be adjusted based Afterload on systemic arterial pressure (afterload). PATHOPHYSIOLOGY OF HEART FAILURE Microsoft Clipart (manually altered) Cardiac Function is Impaired Heart the Failure when there is Remember hearthappens is a pump… one or more alterations in preload, SV COcardiac contractility HR leading afterload or to decreased Cardiac Output. • Cardiac Output is a reflection of how well the heart is doing its jobAFTERLOAD of being a pump. CONTRACTILITY Decreased ATP Preload If vascular resistance is • HR either speeds up or slows down depending production and A stiffer heart will elevated, the heart has availability of Calcium of what the sympathetic or parasympathetic decrease the amount to pump harder to causes the heart to of blood at the end of overcome putting whations nervous system tells theit, heart to do. become less able to diastole stress on it which can • SV is determined by our friends preload, contract effectively wear it out afterload and cardiac contractility. (Porth & Matfin, 2009) These Malfunctions can be Classified into Systolic and Diastolic Dysfunction Click on each box to find the definition. Remember the arrow should turn to a hand before you click. Impaired contractility leads to a decrease in Ejection Fraction SYSTOLIC and Cardiac Output. Preload, ventricular wall dilation and DYSFUNCTION pressure subsequently increase. The ventricles are unable to DIASTOLIC relax and expand, leading to a decrease in preload, stroke DYSFUNCTION volume and cardiac output. (Porth & Matfin, 2009) Heart Failure can also be classified as either Left Sided Heart Failure or Right Sided Heart failure. Right Heart Failure Left Heart Failure Are you starting to see how excess fluid balance contributes to heart failure? Blood cannot reach the lungs to get oxygenated. Blood begins to pool in the venous system and tissues. Dependent Edema Jugular Vein Distension Ascites Pooling of Blood in GI Tract Pooling of Blood in Hepatic Veins Oxygenized blood from the lungs cannot get to the body. Cardiac Output decreases and blood pools in the lungs. Decrease in Tissue Perfusion Activity Intolerance Cough, Orthopnea Hypoxia, PND Pumonary Edema (Porth & Matfin, 2009) Before learning about what causes these malfunctions to occur….Let’s Review Yes! Good Job. Afterload Excellent! Preload Cardiac That’s Right! Contractility Try Again. This is Blood the thickness of Viscosity the blood. Diastolic Try Again! Dysfunction Priastolic Sorry I made this one up! Dysfunction No. Right We didn’t talk about this Ventricular one. Dysfunction Systolic Great! Dysfuction CAUSES OF HEART FAILURE ***Remember to place your cursor over the underline words to get the definition*** Microsoft Clipart (manually altered) Acute Coronary Syndrome Myocardial Infarction and Unstable Angina Decreased blood flow to the myocardium caused by a clot in the coronary arteries. Blood begins to pool leading to fluid volume overload!!! Myocardial Damage (Infarction): evidenced by serum cardiac markers (CK-MB, Troponin). Ventricular Remodeling: the area of the ventricle that is damaged undergoes changes in size, shape and thickness (hypertrophy and dilation). Damage to the ventricle can lead to alterations in preload, afterload and cardiac contractility leading to a decrease in cardiac output. (Porth & Matfin, 2009) Ischemic Heart Disease Coronary Artery Disease Decreased blood flow to the myocardium from the coronary arteries caused by plaque buildup. Blood begins to pool leading to fluid volume overload!!! Myocardial Damage (Infarction): evidenced by serum cardiac markers (CK-MB, Troponin). Ventricular Remodeling: the area of the ventricle that is damaged undergoes changes in size, shape and thickness (hypertrophy and dilation). Damage to the ventricle can lead to alterations in preload, afterload and cardiac contractility leading to a decrease in cardiac output. (Porth & Matfin, 2009) Cardiomyopathy Hypertrophic Cardiomyopathy Left Ventricle thickens through genetic predisposition. Blood begins to pool leading to fluid volume overload!!! The heart is unable to fill properly during diastole – Altered Preload. Stroke volume is decreased. Cardiac Output is decreased. (Porth & Matfin, 2009) Cardiomyopathy cont… Dilated Cardiomyopathy The ventricle is enlarged and wall thickness is decreased due to genetic predisposition, infection, alcohol or unknown cause. Blood begins to pool leading to fluid volume overload!!! Preload and pressure increase. Cardiac Output decreases. (Porth & Matfin, 2009) Valvular Heart Disease Mitral Valve Disorders Stenosis Regurgitation Because the valve is unable to open fully, the left atrium becomes distended leading to impaired filling during diastole. This leads to decreased cardiac output. Because the valve does not open and close completely, it becomes leaky. Stroke volume is reduced leading to decreased cardiac output. Blood begins to pool leading to fluid volume overload!!! (Porth & Matfin, 2009) Valvular Heart Disease Cont… Aortic Valve Disorder Stenosis Regurgitation Because the valve is unable to open fully, blood is unable to exit the left ventricle properly and begins to pool. This decreases cardiac output. Because the valve allows blood to flow back into the left ventricle during diastole, cardiac output is decreased. Blood begins to pool leading to fluid volume overload!!! (Porth & Matfin, 2009) Let’s see if you understand causes of heart failure… Try Again! This is Dilated a cause of chronic Cardiomyopathy heart failure. Excellent! Ischemia to the Myocardial heart can cause it to not pumpInfarction blood like it should resulting in heart failure. Nope. Keep thinking! This is a Aortic Stenosis chronic cause of HF. This is a cause of Mitral Valve chronic heart Prolapse failure. Blood cannot fill Now you’re properly during thinking! diastole. Cardiac Output is Yay! decreased. Blood will spill out Now that’s just of the heart crazy talk. everywhere. Blood pools Good Job! creating edema. Microsoft Clipart Nursing Interventions Let’s take a look at how you fit into taking care of heart failure patients… Take a minute to think of nursing interventions you do on a daily basis that might apply to a patient with heart failure. Remember the nursing process…? Assess Evaluate Implement Diagnose Plan Keep clicking to advance the animation. Fluid Volume Excess (Ackley & Ladwig, 2006) Things You Would Find On Assessment • Assessment – – – – – – Lung sounds Daily weights Vital signs I & O’s Behavior Drug side effects • Interventions – – – – Restricted sodium diet Fluid restrictions Diuretics Turning patients with edema – Promoting positive self image – Consult with physician Microsoft Clipart Heart Failure and Aging The Stats • ¾ of the 5 million Americans suffering with heart failure are over the age of 65 and ½ are over the age of You 75. can see that older adults with heart failure are a huge population for us as • Heart failure is the leading cause of hospitalization healthcare providers. As America ages, the among the elderly. population will grow larger. • 1 million older adults areonly hospitalized annually with heart failure. (AHA, 2010) Changes Related to Aging (Thomas & Rich, 2006) • Arteries stiffen creating resistance against which the heart has to pump. • Heart muscle stiffens, creating filling difficulty. • Cardiac Output declines due to a decline in the maximum rate the heart can reach. • The aged are less able to increase the force of their contractions as is needed during stress, illness and exercise. Remember Starling’s Law… End-Diastolic Volume Stretching of Cardiac Muscle Force of Contraction With age the heart muscles stiffens, limiting the amount of blood that can fill during diastole. Thus the fibers cannot stretch as far, creating a decreased force The more The greater blood in the The more the of contraction. the force of heart at the cardiac muscle end of diastole… fibers stretch… the contraction. (Thomas & Rich, 2006) Microsoft Clipart Heart Failure and Stress Remember the equation for cardiac output… SV CO HR In a diseased heart, cardiac output would not increase as it should during the If the heart rate is under sympathetic nervous system (SNS) and parasympathetic nervous system (PSNS) control….think about normal stress response. The heart would what chronic stress would do to the heart rate and subsequently cardiacof output…. not be capable pumping blood Stress efficiently. Therefore a prolonged stress Release of Increased Activation Epinephrine responseof SNS would onlyandexacerbate signs heartthe rate and blood pressure Norepinephrine and symptoms of heart failure. (Porth & Matfin, 2009) Heart Failure and Inflammation • Inflammatory mediators (such as nitric oxide) are activated in a patient with heart failure in an effort to improve cardiac function. • These mediators can damage the endothelium in blood vessels supplying the heart with blood. • Ventricular and vascular remodeling of the myocardium may be a result of this damage. • Ventricular remodeling of the myocardium can result in heart failure because the ventricular cannot pump blood efficiently. Blood begins to pool leading to fluid volume overload!!! (Brunini, et.al., 2009) Genetics and Heart Failure • Some patients are believed to be at high risk for heart failure due to their genetic make-up. • In a small population, mutations have been found in single genes that trigger the development of heart failure. • Gene mutations have been found in the people with ventricular remodeling and cardiomyopathies • Some mutation examples are – Genes encoding for protein components of the sarcomere which leads to hypertrophy of the myocardium. – Gene mutations resulting in altered dystrophin which normally gives stability to the sarcomere. Blood begins to pool leading to fluid volume overload!!! (Morita, Seidman & Seidman, 2005) References Ackley, B.J. & Ladwig, G.B (2006). Nursing diagnosis handbook: a guide to planning care (7th Ed.). St. Louis, MO: Mosby Elsevier. American Heart Association (2010). Statistics retrieved from http://www.americanheart.org/presenter.jhtml?identifier=1200026. Brunini, T.M., Mann, G.E., Matsuura, C., Meirelles, L.R., Menden-Ribeiro,A.C., & Moss, M.B. (2009). The role of exercise on l-arginine nitric oxide pathway in chronic heart failure. The Open Biochemistry Journal, 3, 55-65. Morita, H., Seidman, C.E., & Seidman, J. (2005). Genetic causes of human heart failure. The Journal of Clinical Investigation, 115(3), 518-526. Porth, C.M. & Matfin, G. (2009). Pathophysiology: concepts of altered health status (8th Ed.). Philadelphia, PA: Lippincott Williams & Wilkins. Thomas, S. & Rich, M.W. (2006). Heart failure in older people. Generations (Fall 2006), pp. 25-32. Contact Information Questions, Comments, Concerns? Sarah Carek, RN, MSN student careksl@yahoo.com (608) 577-7866