Introduction to Cancer Genetics - West Essex General Practice
advertisement

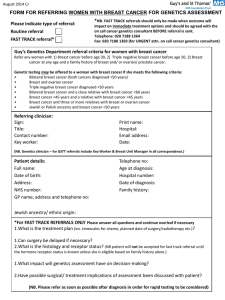
Introduction to Cancer Genetics Emma Williams Genetic Counsellor NE Thames Regional Genetics Service Overview Cancer Syndromes & Management options Genes & Genetic testing Genetic Counselling & Cancer Genetic Service Population cancer risk What are the cancer risks for the general population? • 1 in 3 people will develop cancer at some point in their lives – – – – – – – – Prostate: Female Breast: Lung: Colorectal cancer: Melanoma: Ovarian: Stomach / Pancreas: Male breast: 17% 12-13% 6-8% 6% 1-2% 1.5% 1% 0.1% SEER Figures. NCI 2001-2003 How Many Cancers are Genetic? Sporadic (~85%) Familial (~10%) Hereditary (~5%) Sporadic Cancer • Many patients may have a similar FHx • Age of diagnosis typically later in life • Usually not inherited • Can be reassuring Aims of Genetic Counselling Help patients to… • Understand the information about the genetic condition • Appreciate inheritance patterns and risk of recurrence • Understand available options • Make informed choices appropriate to their personal and family situation • Make the best possible adjustment to the condition and risk North East Thames Regional Genetics Service Genetic Clinics in NE Thames Cancer Genetics Clinics General Genetics Clinics Referral guidelines http://www.ich.ucl.ac.uk/gosh/clinicalservices/Clinical_genetics/Custom%20Menu_01 Do Genes Affect Cancer Risk? Risk Assessment Tools • • • • • Referral guidelines / NICE guidelines Family History form Comprehensive 3 generation pedigree Confirmation of cancer pathology Pedigree assessment – Manchester score – BOADICEA (Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm) – Amsterdam I/II Criteria – Bethesda Criteria Genetic Cancers • • • • • • • • • • • • • Breast and ovarian Colon cancers Cowden syndrome Gastric cancer Gorlin Syndrome Li-Fraumeni Multiple endocrine neoplasia (MEN) Neurofibromatosis Peutz-Jeghers syndrome Phaeochromocytoma Retinoblastoma von Hippel-Lindau disease Wilm’s tumour Hereditary Cancer Several affected family members Earlier than average age of onset Multiple generations are affected on one side of the family A particular pattern of cancers noted Individuals with more than one primary tumour site 5-10% of Cancer Cases Most Cancer Susceptibility Genes Are Dominant With Incomplete Penetrance Normal Susceptible Carrier Carrier, affected Ca Sporadic Ca • You only need one altered copy of the gene to have an increased risk of cancer • Gender is irrelevant • It is not possible to “skip” generations • Penetrance can be incomplete • All offspring are at 50:50 risk Genetic Testing • Genetic testing is usually carried out on DNA from a blood sample • Technically difficult to locate the mutation in a cancer gene for a particular family – Can take up to three months • Usually need to first test a living relative who has already developed cancer • Is only offered to high risk families (>20% chance of mutation) • Often cannot locate a mutation in a family (only identified in about 20% of families) Genetic Testing cont… • Genetic testing is NOT usually possible if there are no living affected relatives – Exception is populations with founder mutations eg Ashkenazi Jewish population • Once a mutation is found, testing can be offered to other at-risk family members • Individuals who DO NOT carry the family mutation ARE NOT at increased risk of developing the cancers, but are still at population risk • Individuals who DO carry the family mutation ARE at increased risk of developing cancer but there is still uncertainty. . . However, testing enables us to identify individuals who may be at higher risk of developing certain types of cancer Hereditary Breast and Ovarian Cancer Other genes BRCA1 BRCA2 5-10% Sporadic Hereditary • Most cases caused by a mutation in BRCA1 or BRCA2 gene • BRCA1 / 2 are tumour suppressor genes, which are involved in the repair of DNA • Accounts for about 5% of breast cancer cases and about 12% of ovarian cancer cases BRCA1 -Associated Cancers: Lifetime Risk Breast cancer 56%-87% (often early age at onset) Second primary breast cancer 64% Ovarian cancer 16%-44% Increased risk of other cancers, eg about double population risk for prostate cancer in men BRCA2-Associated Cancers: Lifetime Risk breast cancer (50%-80%) male breast cancer (7%) contralateral breast (50%) ovarian cancer (15-27%) prostate (~30%) Other cancers: pancreatic malignant melanoma Options for BRCA1/2 Carriers • Cancer Screening – Additional breast screening by mammography / MRI – Ovarian screening through UKFOCSS research trial • Prophylactic bilateral mastectomy – ~90% reduction in breast CA risk • Prophylactic bilateral salpingo-oophorectomy – ~up to 96-98% reduction in ovarian CA risk – ~50% reduction in breast CA risk (age dependant) • ? Chemoprevention in the future • ? Tailoring of treatment for carriers in the future When to refer • 2 first or second degree relatives with breast cancer < 50 yr • 3 first or second degree relatives with breast cancer <60yr • 4 relatives with breast cancer at any age • 1 ovarian cancer at any age + 1 breast cancer < 50yr • 1 ovarian cancer + 2 breast cancer both < 60y • 2 ovarian cancer any age • Patients who are thought to be of Ashkenazi Jewish heritage with at least one first degree relative with breast cancer <50 years or ovarian cancer any age • NB bilateral breast primaries equivalent to 2 relatives Colorectal Cancer Sporadic (~60%) Familial (~30%) Rare FAP (~1%) Syndromes (~4%) MAP (~1%) HNPCC (3-5%) HNPCC or Lynch syndrome Hereditary non-polyposis colorectal cancer (HNPCC) • 3-5% of all colorectal cancer cases • Autosomal dominant – multiple generations affected • High penetrance • Typical age of CA onset is 40-50 yrs • 60-70% right-sided/proximal CRC tumors • Polyps may be present, multiple primaries common. Can overlap with AFAP HNPCC • Lifetime cancer risks: – Colorectal – – – – – – – Endometrial Gastric Ovarian Biliary tract Urinary tract Small bowel Brain/CNS 80% 20-60% 13-19% 9-12% 2% 4% 1-4% 1-3% HNPCC Caused by mutations or deletions in mismatch repair (MMR) genes MMR genes are like spell checkers in our DNA. MSH2, MLH1, MSH6, PMS2 90% of detectable mutations in MSH2 and MLH1 7-10% of detectable mutations in MSH6 Options for individuals with HNPCC • 1-2 yearly colonoscopy • Ovarian and endometrial screening (not proven to be effective) • ? renal/upper GI screening effective (if have history of gastric/renal cancers) • Surgery – Prophylactic bowel surgery not often chosen – Total abdominal hysterectomy and salphingo oophorectomy for females Familial adenomatous polyposis (FAP) • 1 in 10,000 incidence • 100’s to 1000’s of colonic adenomas by teens • 7% risk of CRC by 21 yrs; 93% by 50 yrs • 20-25% no history in parents • Extra-colonic features • Screening – 1 – 2 yearly flexible sigmoidoscopy from age 10 – 12 – Upper GI endoscopy 1 –3 yearly from age 25 MAP syndrome/MYH gene • MYH associated Polyposis (MAP) syndrome – Autosomal recessive; mutations in the MYH gene – Median number of polyps = 55 – Mean age of polyp diagnosis = 30-50 years – Polyps mainly small, mildly dysplastic tubular adenomas. Some tubulovillous, hyperplastic, serrated adenomas, microadenomas • 30% of individuals with 15-100 polyps have homozygous mutations in the MYH gene • Genetic testing should be offered if >10-15 polyps (and APC gene testing negative) When to refer • • • • Patient or 1 first degree relative affected with – Colorectal cancer <50yrs – 2 or more colorectal primary cancers any age – Colorectal cancer and a related cancer* any age. 2 first degree relatives affected with colorectal cancer or related cancer* at any age 3 relatives affected with colorectal cancer or related cancer* at any age, one of which must be a first degree relative. History of Polyposis (e.g. Familial adenomatous Polyposis) – *related cancers- endometrial, ovarian, small bowel, ureter, renal pelvis and stomach Genetics and Uncertainty • Cancer genetics is not relevant for most people • Cancer genetics is not a crystal ball But cancer genetics can have a great impact on those families most at risk of familial cancer What Can You Do? • Recognise patterns of cancers in families – Young onset – Lots of one or two particular types of cancer – Jewish? • If not sure ask – Don’t be afraid to contact genetics for advice • Take a blood sample for DNA banking DNA Banking • DNA banking provides families with the chance to pursue genetic testing at a later point in time. – where there is currently no genetic test available. DNA banking will allow the family to take advantage of future advances in genetic testing technology. – A family member diagnosed with cancer who is terminally ill and there is no time for traditional a genetic assessment and/or testing. The family can then focus their attention on their loved one and defer the process of genetic counselling and testing to a time when they are ready. Contact Details Emma Williams Registered Genetic Counsellor NE Thames Regional Genetics Service Great Ormond Street Hospital Great Ormond Street London, WC1N 3JH email: emma.williams@gosh.nhs.uk Tel: 0207 905 2625 Fax: 0207 813 8141 Case 1: Ruth Ruth, a 35 year old Ashkenazi Jewish woman, comes because she is anxious about her family history of cancer. You inquire about family health history and find out the following information: – Paternal family history is as follows: • Paternal grandmother diagnosed with ovarian cancer age at 63 • Paternal aunt diagnosed with breast cancer age 42 Ruth has no other risk factors or pertinent family history Case 1: Pedigree Polish Jewish Russian Jewish Dx 63 82 yrs Dx 42 60 58 Key 64yrs 41 Ruth 35 38 -Ov Ca -Br CA Case 1: Assessment • Patient is in “Moderate risk” category • However ethnicity is important as she is of Ashkenazi Jewish descent • Refer to genetics clinic • Moderate risk screening for breast cancer arranged • Genetic testing for 3 common ‘Jewish Mutations’ Case 2: Ann • Ann has come along because her sister has ovarian cancer, sadly the cancer has spread. Her family history is a follows: • Sister diagnosed with ovarian CA at 53 yrs. • Mother diagnosed with ovarian CA at 61 yrs and has sadly died. • Maternal aunt diagnosed with breast cancer at 48 yrs. Ann has no other risk factors for breast cancer. She feels that with her family history, cancer is inevitable Case 2: Pedigree Dx 61 Dx 48 Died 64 73 39 DX 53 2 49 65 3 30s 2 Case 2: Assessment • Patient is in “High” risk category • Refer to genetics clinic promptly • High risk screening breast and ovarian cancer • Genetic testing offered Case 3 • • • Helen has primary ovarian cancer Would this family need seeing by genetics? What other cancer could she be at risk for? YES Colon and uterine cancers Case 4 French, Irish, Scottish German, English 88 yr Dx 50 61 yr CRC Dx 48 63 yr 4 polyps 50 yrs. Key: 38 yr 35 yr Endometrial CA Dx 38 Colorectal CA Adenomatous polyps Lynch syndrome 10 yr 8 yr Case 5 • • Would you refer this gentleman to genetics? What else would you ask about the family? YES Is he Jewish? He has a BRCA mutation! Case 6 • • Which side of the family are you worried about? What surveillance does she need? Both Breast and ovarian screening She actually had two BRCA mutations! Case 7: Ted • Ted is 30 and wants a colonoscopy because his mother was just diagnosed with colon cancer after routine screening at age 54. Family history reveals: – Paternal grandfather: died of CRC at age 79. – No hx of endometrial, ovarian, small bowel or ureter/kidney cancer on either side of family. – Two maternal aunts: cervical cancer at ages 30 & 34 – Maternal grandmother: breast cancer age 85 Reassure Case 8: Alison Alison is a 40 year old Caucasian (non-Jewish) patient who asks you for information about the “breast cancer gene test”. She states she wants this test. You ask about her family history: – Mother with breast cancer - age 58 – Maternal aunt with breast cancer – age 65 – Paternal grandmother with breast cancer – age 79 Alison has no other risk factors for breast cancer She feels that with her family history, breast cancer is inevitable Case 8: Pedigree British German/Dutch Dx 79 d.81 Dx 58 65 yr Dx 65 71 yr Key: Alison 40 yr 15 yr -Breast CA Case 8: Assessment • Patient is in “Moderate” risk category • Refer to breast clinic for breast cancer screening from 40-50 years then NBSP • Counselling issues: – Unlikely to be due to a BRCA1 or BRCA2 mutation – Screening and preventive strategies – Psychosocial – perceived risk, fears – Support resources