Evidence-based clinical practice
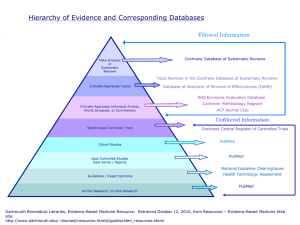
advertisement
Evidence based medicine and clinical practice Dr. J Tumbo Evidence-based clinical practice Is an approach decision-making which the to in clinician uses the best evidence available, in consultation with the patient, to decide upon the option which suits that patient best. The Evidence-based Medicine Triad Source: Florida State University, College of Medicine. What is EBP • The conscientious use of current best scientific research in making decisions regarding care of a particular patient. • It integrates current best knowledge with practitioner’s experience and patient values. • It is the link between research and patient care • Options exist of using evidence from primary studies or preappraised publications e.g. The Cochrane, Evidence that matters Clinical Questions/situations addressed in EBP Therapeutic: questions about treatment that would be given to a patient and the treatment outcomes of the different options Diagnostic: questions about the degree to which a particular test is reliable in picking the condition Prognostic: questions about a patient’s future health, lifespan and quality of life in the event that he chooses a particular treatment option or is affected by a specific condition 5 steps 1. Formulate an answerable question 2. Track down the best evidence 3. 4. 5. Critically appraise the evidence for validity, clinical relevance and applicability Individualize, based clinical expertise and patient concerns Evaluate your own performance (clinical audit) Assess your patient Ask clinical questions Acquire the best evidence Appraise the evidence Apply evidence to patient care Characteristics of answerable question (PICO) 1. Patient or Problem or Population – Describes your patient, problem or population: ask “how would I describe a group of patients similar to mine?” 2. Intervention – Activity or process related to the patient : ask “which main intervention am I considering 3. Comparison intervention (if appropriate) – ask “what is the main alternative to compare with the intervention” 4. Outcome (s) – End result of activity or intervention: ask “what can I hope to accomplish?” A. Asking the question The creation of a question from the clinical scenario is the first crucial step in searching for an answer. It arises from a comprehensive assessment of the clinical situation. Guided by clinical tasks relevant to the scenario Example of question What is the risk of development of Cancer of the Breast in a 52 year old woman using estrogen-only pills as hormone replacement therapy. B. Acquiring the best evidence • Tracking down the best evidence can be manual or computerised. • Computerised literature search needs skill in searching. • Needs for reliable sites e.g. PubMed • Use of key words (not the whole question) in the search box • Refine the search by filters to narrow down available literature and getting full text articles Refining the search Boolean operators: conjunction words that link or exclude the key words. Common Boolean operators include AND, OR, NOT. Using LIMITS to narrow the search finding. One may limit the search on the various attributes that include “Human or animal studies”, Gender, Age, Year of publication, research type and even the specialty Truncating mean the use of a asterix * as suffice to part of a word that may end in multiple ways. For example, if Bacter* is entered as a key word, the computer will search for all words starting with bacter that include Bacteria, Bacteriology, Bacterium etc. Use synonyms (words which has the same meaning as another e.g. Manager and Executive, Woman and Female). Related links/citations MESH database What is the best evidence Hierrhachy of evidence in epidemiological studies 1. Systematic reviews/meta-analysis 2. Randomized controlled trial 3. Cohort studies 4. Case control studies 5. Cross sectional studies 6. Case report 7. Anecdotes Causality Association Descriptive Case report/series Descriptive study of an experience or occurrence in one or many individuals Individual patients Patient notes Combined notes Case report Cross sectional study Descriptive study of observation or measurement of characteristics of a defined population at a specific point in time. No follow-up Population observation describe results Case control study Before exposure disease Hx of past exposure Cases/controls with/out Exposure relative to outcome Compare histories Draw conclusion Cohort study Study of group or groups with no disease in the beginning. Exposure and follow-up is done prospectively then measurement of outcome Cohorts start Outcomes Exposure/Followup cohort at end Compare outcome e.g. CANCER OF BRONCHUS Randomised controlled trial Analytical study in which study participants are randomly assigned to exposure by researcher then followed up to identify outcome Population outcome randomisation exposure followup Compare results Systematic review/Metanalysis Study 1 Study 2 Combined results Study 3 Study 4 What Is a Systematic Review? • Systematic reviews are scientific investigations in themselves, with an a priori protocol(pre-planned methods) and an assembly of original studies as their "subjects." • They synthesize the results of multiple primary investigations by using strategies that limit bias and random error What is a meta-analysis • Enhance precision by pooling smaller studies (to artificially create one large study) • to arrive at a common estimate with a certain level of certainty Perform a search on PubMed Subject searching www.pubmed.gov You are challenged by the huge number of pregnant women presenting with PET. You recall that APRIRIN could be used to prevent PET. However there are differing opinions on this. How will you proceed Search the Cochrane Library International Cochrane Collaboration >90 countries effects of interventions Includes: Full-text Systematic Reviews Abstracts to further SRs and RCTs Available at: http://www.thecochranelibrary.com C. Appraisal Refers to the assessment of evidence by systematically reviewing its relevance, validity and results to specific situations. Chambers, R. (1998). Clinical effectiveness made easy: first thoughts on clinical governance. Oxford, Radcliffe Medical Press. When you search Medline, the references that you retrieve have been published in recognised medical journals, some of which will have been peer reviewed. The peer review process means that the articles have been assessed by an expert in the field. This should help to prevent poor or inaccurate research being published. However, this does not mean that the research is always accurate or valid. Not all research is good research. One of the key messages of evidence based medicine is: "Don't believe everything you read." Why is it important Critical appraisal is important because it: • ensures a comprehensive assessment of the whole paper • allows you to identify the strengths and weaknesses of a piece of research • develops an improved understanding of the research methodology used to conduct the research • allows you to relate the published research to your local situation • enables you to identify any bias in the research • facilitates the implementation of effective interventions in your clinical practice Process of critical appraisal The process of critical appraisal can be very time consuming. It requires you to carefully read the whole article, especially the research methodology and statistical analysis - not just the "easy" bits like the introduction, results and conclusion sections! When reading an article you need to consider the following: • Who has written the article? Are they a recognised author. Are they affiliated to a recognised institution? • Why? What are the aims and objectives? • How? Has the right research methodology been used? • When? Is it recent or seminal research? • Where? Has it been published in a recognised journal? Is it a peer reviewed journal? • Do the results seem valid? • Does the statistical evidence seem valid? • Is there any obvious bias or conflict of interests? • Do the conclusions stack up? READER Relevance Education Is the study relevant to answer my Question? Does it challenge my knowledge? Applicability Does it apply to my situation? Discrimination What is the scientific quality of the paper? Evaluation What is my evaluation based on above? Reaction How can I use the information? Three questions of critical appraisal: VIA 1. Is the study Valid? Discrimination & Evaluation 2. Is it Important? Relevance & Education 3. Is it Applicable to my patient? Applicability & Reaction Question 1: Is the study valid? Type of study – strength of evidence Is the study methodology appropriate to answer the research question? Was the study done properly? Levels of evidence What type of study would give the best evidence for each type of question? Level 1a: Systematic reviews; Level 1b: Individual RCTs with narrow confidence interval Level 2a & b: Cohort studies; Level 2c: Outcomes research Level 3a & b: Case-control studies Level 4: Case series & poor quality cohort /case control studies) Level 5: Expert opinion Was the study done properly? Sample Representative and appropriate Case-control: Are cases and controls comparable Cohort: Was patients followed long enough Was loss to follow-up not too much? Randomised Controlled Trial: Double-blind Was randomisation done properly Systemic Review: Are all primary studies of high quality eg randomised controlled trials? Were results consistent Is the process explicit? Is synthesis accurate? Are findings important? Impact/Prognosis P-value Confidence interval Outcome over time Aetiology Relative risk Odds ratio Significance Diagnosis/evaluate tests Compare pre- and post-test probability Sensitivity Specificity Predictive value Treatment/harm Numbers needed to treat/harm Absolute risk reduction Is it applicable? Is your setting comparable to that of the study? Will the application of the evidence have a positive impact on your patients? What are your patients preferences? Would it be affordable in your setting? What alternatives are available in your setting? Integration into practice • Is your patient different from those in study • How much effect do you expect in your patients • Are there alternatives • Wat does the patient think? Other sources of evidence WHO CHOICE (Choosing interventions that are cost-effective) WHO initiative developed in 1998 Reports the costs and effects of a wide range of health interventions in the 14 epidemiological sub-regions Ten best health buys 1. Vaccination of children against major childhood illnesses including measles, polio, tetanus, whooping cough, and diphtheria 2. Monitor children’s health to prevent or, if necessary, treat childhood pneumonia, diarrhoea, and malaria 3. Tax tobacco products to increase consumers’ costs by at least one-third to curb smoking and reduce the prevalence of cardiovascular disease, cancer, and respiratory disease. 4. Attack the spread of HIV through a coordinated approach that includes: promoting 100 percent condom use among populations at high risk treating other sexually transmitted infections providing antiretroviral medications, especially for pregnant women offering voluntary HIV counselling and testing. 5. Give children and pregnant women essential nutrients including vitamin A, iron and iodine to prevent maternal anaemia, infant deaths, and long-term health problems 6. Provide insecticide-treated bed nets in malariaendemic areas to drastically reduce malaria 7. Enforce traffic regulations and install speed bumps at dangerous intersections to reduce traffic-related injuries 8. Treat TB patients with short-course chemotherapy to cure infected people and prevent new infections 9. Teach mothers and train birth attendants to keep newborns warm and clean to reduce illness and death 10. Promote use of aspirin and other inexpensive drugs to treat and prevent heart attack and stroke Resources Cochrane Library www.thecochranelibrary.com PubMed www.pubmed.gov TRIP www.tripdatabase.com Other sources – CEBM web-site – EBM tools www.cebm.net