Assessing and Improving the Understanding of DNR/DNI among
Understanding Code Status Course: Assessing and Improving the
Understanding of DNR/DNI among Medical Students and Residents
Aroonsiri (June)Sangarlangkarn
1
, MD, MPH, Margaret Drickamer
2
, MD
1 Yale Internal Medicine Residency Program, New Haven and Waterbury, CT
2 Department of Geriatrics, Yale School of Medicine, New Haven, CT
INTRODUCTION
• Many studies demonstrate continued deficiencies in physicians’ education about end-of-life care (ACGME, ABIM)
• There is limited literature on how health care providers understand the meaning and ramifications of DNR/DNI
• There is limited literature on validated teaching tools on the ramifications of DNR/DNI on patient care for health care providers
• Our study aims to assess:
1. The understanding of DNR/DNI among physicians in training
2. The efficacy of case-based learning in code status education
METHODS
Case-based learning course:
Similar format as Yale Office-Based Medicine Curriculum – literaturebased interactive course that provides an evidence-based approach to clinical practice used by residency programs across the US
Three challenging end-of-life cases focusing on DNR/not DNI patients, reversibility, futility
Qualitative surveys:
September-October 2011, before and after case-based learning course administered at noon conference attended by medical students and residents as part of Yale School of Medicine internal medicine rotations
Evaluate improvements in responses using exact Mcnemar test
Survey content:
1. DNI section: What can you give a DNI patient who has a pulse but is in respiratory failure? (check all that apply)
2. DNR section: What can you give a DNR patient in cardiopulmonary arrest? (check all that apply)
3. Adequate understanding of what DNR/DNI means?: 5 (strongly agree) to 1 (strongly disagree)
4. Would you recommend this course to others?: 5 (strongly agree) to 1
(strongly disagree)
REFERENCES
Blank LL. Overview on ABIM end-of-life patient care project: caring for the dying: identification and promotion of physician competency.
Hosp
J
1998;13: 145-50
Weissman DE et al. ACGME Requirements for End-of-life Training in
Selected Residency and Fellowship Programs: A Status Report.
Acad Med
2002;77:299-304
RESULTS
35.00%
30.00%
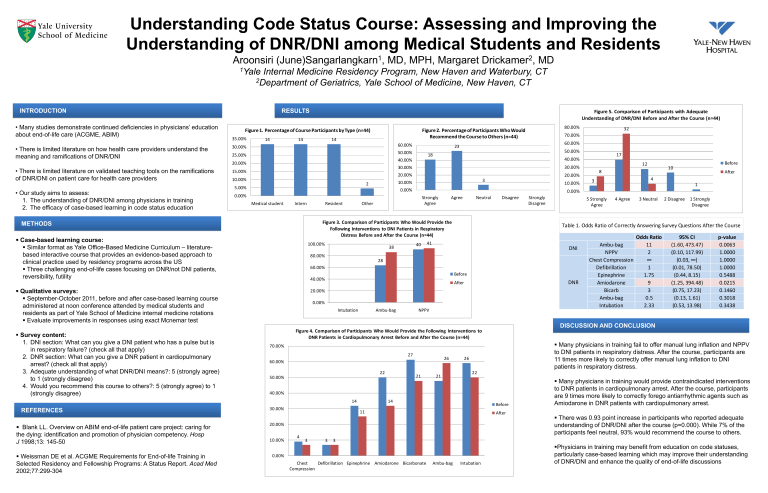
Figure 1. Percentage of Course Participants by Type (n=44)
14 14 14
25.00%
20.00%
15.00%
10.00%
5.00%
0.00%
2
Medical student Intern Resident Other
60.00%
50.00%
40.00%
30.00%
20.00%
10.00%
0.00%
Figure 2. Percentage of Participants Who Would
Recommend the Course to Others (n=44)
23
18
3
Strongly
Agree
Agree Neutral Disagree Strongly
Disagree
Figure 3. Comparison of Participants Who Would Provide the
Following Interventions to DNI Patients in Respiratory
Distress Before and After the Course (n=44)
100.00%
38
40
41
80.00%
28
60.00%
Before
40.00%
After
20.00%
0.00%
Intubation Ambu-bag NPPV
Figure 4. Comparison of Participants Who Would Provide the Following Interventions to
DNR Patients in Cardiopulmonary Arrest Before and After the Course (n=44)
70.00%
60.00%
27
26 26
50.00%
22
21 21
22
40.00%
30.00%
14
11
14
20.00%
10.00%
4
3 3 3
0.00%
Chest
Compression
Defibrillation Epinephrine Amiodarone Bicarbonate Ambu-bag Intubation
Before
After
80.00%
70.00%
60.00%
50.00%
40.00%
30.00%
20.00%
10.00%
0.00%
Figure 5. Comparison of Participants with Adequate
Understanding of DNR/DNI Before and After the Course (n=44)
32
3
8
17
12
4
10
1
5 Strongly
Agree
4 Agree 3 Neutral 2 Disagree 1 Strongly
Disagree
Before
After
Table 1. Odds Ratio of Correctly Answering Survey Questions After the Course
DNI
DNR
Ambu-bag
NPPV
Chest Compression
Defibrillation
Epinephrine
Amiodarone
Bicarb
Ambu-bag
Intubation
Odds Ratio
11
2
∞
1
1.75
9
3
0.5
2.33
95% CI
(1.60, 473.47)
(0.10, 117.99)
(0.03, ∞)
(0.01, 78.50)
(0.44, 8.15)
(1.25, 394.48)
(0.75, 17.23)
(0.13, 1.61)
(0.53, 13.98)
p-value
0.0063
1.0000
1.0000
1.0000
0.5488
0.0215
0.1460
0.3018
0.3438
DISCUSSION AND CONCLUSION
Many physicians in training fail to offer manual lung inflation and NPPV to DNI patients in respiratory distress. After the course, participants are
11 times more likely to correctly offer manual lung inflation to DNI patients in respiratory distress.
Many physicians in training would provide contraindicated interventions to DNR patients in cardiopulmonary arrest. After the course, participants are 9 times more likely to correctly forego antiarrhythmic agents such as
Amiodarone in DNR patients with cardiopulmonary arrest.
There was 0.93 point increase in participants who reported adequate understanding of DNR/DNI after the course (p=0.000). While 7% of the participants feel neutral, 93% would recommend the course to others.
Physicians in training may benefit from education on code statuses, particularly case-based learning which may improve their understanding of DNR/DNI and enhance the quality of end-of-life discussions