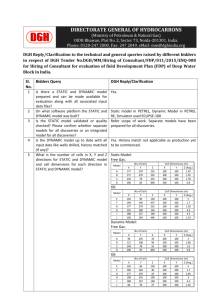
Collaborative, Seamless, Patient-Centred, Alcohol Care In Bolton

COLLABORATIVE, SEAMLESS,
PATIENT-CENTRED,
ALCOHOL CARE IN BOLTON
ALCOHOL CARE MODEL
(1990-ONGOING)
Pioneered, Sustained, Evolving
Patient-Centred, Seamless, Holistic
Collaborative Gastroenterology / Psychiatry / Community
Teamworking
Governance
Audit, Research
Training, Education
Health Promotion
Impact / Replicable
1990
Established Multidisciplinary Team
Weekly (1-2) Discuss Inpatients
Nurses, Doctors, Dietician, Physio, OT,
Pharmacist, Chemical Pathologist, Speech
Therapist, Asian Link Worker, Social Worker
(Critical)
Optimised, Unified Care
Facilitated Discharge Planning
Everyone Valued
Teamworking Ethos
1993
WENDY DARLING
- Consultant Psychiatrist
- Substance and Alcohol Misuse
JOINT INPATIENT CARE
SIMULTANEOUS ALCOHOL CLINIC
- Monthly
INITIAL PROBLEMS / PREJUDICES
OVERCOME
NIGHTINGALE WARDS
- Risk Management, Privacy
- Ward Drinking, Drug Misuse
- Advocated / Planned GI Ward
- Opened 2007
- 8 Side Rooms
SELF-INFLICTED DISEASE – Non Judgmental
REMOVED STIGMA
- Asian Community Elders
1998 – DAVID PROCTOR –
PSYCHIATRIC LIAISON NURSE
Hospital/Community
MDT Member
Brief Interventions
A&E, Acute Admissions, Gastroenterology,
Psychiatry, Orthopaedics
Firefighting
HCP Training, Education, Screening Strategy
Joined Simultaneous Alcohol Clinic
- 2 per Month
- Facilitated Communication
- Reduced DNA’s
DAVID PROCTOR (P.L.N) IMPACT
PATIENTS’ RESOURCES
- Asian
LIAISON
- GP’s
- Rapid Response Community Detoxifications
- C.A.T.
- Other Agencies
METICULOUS AUDIT/RESEARCH DATA
- Alcohol Misuse In Older People (2006)
Collaboration Cabinet Office Strategy Unit
- Wernicke-Korsakoff Syndrome (2007)
2006
Sandra Crompton Medical Liver Nurse Practitioner
Partners Emma Dermody, Hospital / Community P.L.N.
Gastroenterologist / Psychiatrist Supervision
Monday - Friday, 8am. Jointly Triage All Admissions
- Brief Interventions
- Inpatient Detoxifications Reduced 50%
- Saves Trust 1000 Bed Days (£300,000) Annually
- Rapid OPD – Sandra, Emma, C.A.T
- Assess Inpatients Daily Reduced Violent Incidents
JOINT GASTROENTEROLOGY/
PSYCHIATRY NURSING
Weekly Clinic. Simultaneous with Doctors
Open Access – Phone, Secretaries, Ward
Regional Referrals
Improved Abstinence
Excellent Patient / Carer / Staff Satisfaction
Feedback Adaptation
Waiting Times, DNA Rates, Length of Stay
Network 50+ Link HCP’s
Education/Training/Support/Audit/Q.A
Data for Health Commissioners
District Health Promotion
2006 CLINICAL GOVERNANCE
MEETINGS
Transparent, No-Blame Culture
All Deaths, Inquests
Clinical Incidents, Complaints
End of Life Care
Infections – MRSA, Cl. difficile
– Root Cause Analysis
– 50% Reduction
Feedback – Trust Governance
– Adaptation
– Audit, Closing the Loop
SEAMLESS BOLTON DISTRICT
ALCOHOL CARE
2007
2007/08
2008
2008
UNIFIED PRIMARY, SECONDARY, C.A.T
DETOXIFICATION
- Lean Methodology, Saves Bed Days
INTEGRATED BOLTON MULTIAGENCY
ALCOHOL STRATEGY
3 HEALTHCARE AWARDS
- Access, Care, Overall Team Of The Year
Pivotal Role with Public Health Team,
Multiagency Partnership persuading
DH Team for Health Inequalities to make Bolton Early Implementer of National Alcohol Strategy
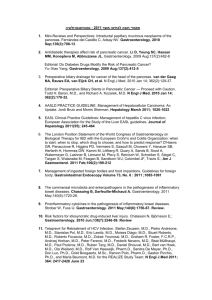
ALCOHOL-RELATED DISEASE
Meeting the challenge of improved quality of care and better use of resources
A Joint Position Paper on behalf of the
British Society of Gastroenterology,
Alcohol Health Alliance UK and the
British Association for Study of the Liver
RECOMMENDATIONS
DGH serving a population of 250,000
Key Recommendation (1)
DGH Requirement
A multidisciplinary “Alcohol Care Team,” led by a
Consultant, with dedicated sessions, who will also collaborate with Public Health, Primary Care Trusts, patient groups and key stakeholders to develop and implement a district alcohol strategy.
Key Recommendation (2)
DGH Requirement
Coordinated policies on detection and management of alcohol-use disorders in Accident and Emergency departments and Acute Medical Units, with access to
Brief Interventions and appropriate services within 24 hours of diagnosis.
Key Recommendation (3)
DGH Requirement
A 7-Day Alcohol Specialist Nurse Service and Alcohol
Link Workers’ Network, consisting of a lead healthcare professional in every clinical area.
Key Recommendation (4)
DGH Requirement
Liaison and Addiction Psychiatrists, specialising in alcohol, with specific responsibility for screening for depression and other psychiatric disorders, to provide an integrated acute hospital service, via membership of the “Alcohol Care Team.”
Key Recommendation (5)
DGH Requirement
Establishment of a hospital-led, multi-agency
Assertive Outreach Alcohol Service, including an emergency physician, acute physician, psychiatric crisis team member, alcohol specialist nurse, Drug and Alcohol Action Team member, hospital/community manager and Primary Care Trust Alcohol
Commissioner, with links to local authority, social services and third sector agencies and charities.
Key Recommendation (6)
DGH Requirement
Multidisciplinary, person-centred care, which is holistic, timely, non-judgmental and responsive to the needs and views of patients and their families.
Key Recommendation (7)
DGH Requirement
Integrated Alcohol Treatment Pathways between primary and secondary care, with progressive movement towards management in primary care.
Key Recommendation (8)
DGH Requirement
Adequate provision of Consultants in gastroenterology and hepatology to deliver specialist care to patients with alcohol-related liver disease.
Key Recommendation (9)
DGH Requirement
National Indicators and Quality metrics, including alcohol-related admissions, readmissions and deaths, against which hospitals should be audited.
Key Recommendation (10)
DGH Requirement
Integrated Modular Training in alcohol and addiction, available for alcohol specialist nurses and trainees in gastroenterology and hepatology, acute medicine, accident and emergency medicine and psychiatry.
Key Recommendation (11)
DGH Requirement
Targeted funding for research into detection, prevention and treatment strategies and outcomes for people with alcohol-use disorders.
CONCLUSION
Many of these recommendations can be implemented by intelligent re-organisation and co-ordination of existing alcohol services, while some require investment in people.
PHILOSOPHY
“We never give up on anybody, even when they have given up on themselves.”