Chikungunya Jan2014
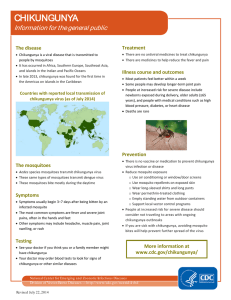
advertisement
Chikungunya Fever: Re-emerging vectorborne disease Margaret McLees, M.D., DTMH Denver Public Health January 17, 2014 Outline Case Presentation Epidemiology Presentation Diagnosis Treatment and Prevention Implications for our Travelers Case 65 yo female with fevers, rash, and arthralgias 12-day trip to Bali, Indonesia, returned 2 days prior Day 12 developed severe arthralgias and arthritis Sick contact: landlord found down, dx’d with viral illness Traveled from Bali to Hong Kong Admitted in Hong Kong for 3 days Persistent severe arthralgias, 1 day diarrhea Rash Paracetamol, diclofenac, ranitidine Case, continued Returned to Denver with ongoing rash and arthralgias, resolution of fevers Medications: oral hormone replacement PMH: Migraines Social Hx: tourist activities while traveling, no bad habits, +insect bites, no animal exposures, no freshwater/saltwater exposures Afebrile on exam Conjunctival erythema Facial edema and rash Upper and lower extremity edema Case: Rash Case: Rash Case: Laboratory data WBC 3.4, 8% bands, plt 109, AST 68 Malaria smear negative Electrolytes, kidney, liver function, urinalysis normal Typhoid & paratyphoid by Widal test, Influenza A&B, Dengue IgM, Brucella abortus Ag by Weil Felix, respiratory virus panel negative CXR: blunted right costophrenic angle, no infiltrates or consolidation Clinical diagnosis: Chikungunya Fever Serologies sent to CDC for arboviruses likely to be present in SE Asia Ross River virus Dengue Chikungunya Japanese encephalitis virus IgM positive to multiple viruses on acute sample Chikungunya, Barmah Forest and Ross River Virus Chikungunya IgM, IgG positive on convalescent samples in May Chikungunya Virus (CHIKV): Alphavirus “That which bends up” in Swahili Togaviridae family Single strand RNA virus, mosquito-transmitted New World: Fever, rash, encephalitis Western equine encephalitis Eastern Equine encephalitis Old World: Fever, rash, arthralgias Chikungunya Ross River Virus (Oceana) Barmah Forest Virus (AUS) O’nyong-nyong (Africa) Semliki Forest Virus (Africa) Mayoro (South America) Sindbis virus (AUS, Africa, Europe, Asia minor) www.cdc.gov/ncidod/dvbid/arbor/alphavir.htm Mosquito Transmission: Aedes aegypti and Aedes albopictus Transmission: Aedes mosquito Aedes aegypti Urban mosquito Needs standing water for larvae Prefers cool, dark areas for resting Feeds through the day, most active at dawn/dusk Eggs do not survive winter in temperate climates Aedes albopictus: Asian Tiger Mosquito Urban, periurban, rural habitats Feeds through the day, most active dawn/afternoon Eggs survive winter in temperate climates Invasive- spreading in Europe and Americas www.cdc.gov CHIKV: Geographic Distribution As of January 6, 2014 www.cdc.gov Aedes: Geographic distribution and CHIKV imported cases Soumahoro at al EID 2010 Transmission Cycle Africa Sylvatic transmission cycle Maintained in non-human primates, small mammals, Aedes mosquitos Human reservoirs during epidemics without animal reservoirs Outbreaks usually associated with heavy rainful and increased mosquito population Asia Human-mosquito cycle Urban epidemics Aedes aegypti and Aedes albopictus Burt FJ et al. Lancet 2012; 379:662-71 www.cdc.gov Transmission by corneal graft La Reunion Outbreak, Indian Ocean 2005-2007 Implementation of screening of organ and tissue donors in 2005 12 of 69 asymptomatic corneal donors were viremic or IgM positive for CHIK 4 of 12 corneas from these donors were infected with CHIK (qRT-PCR) No correlation with systemic symptoms, viremia, or presence of anti-CHIK IgM Mouse models showed ocular innoculation of CHIK produced systemic infection Corneal collection and transplantation suspended Couderc et al. JID 2012 Lumsden WH. Trans Roy Soc Trop Med Hyg 1955;49:33-57 Clinical Findings Incubation period 1-12 days, average 2-4 Abrupt onset fever, myalgias, headache and photophobia Rash: maculopapular, lasting 2-3 days Aphthous ulcers Vesiculobullous lesions with desquamation Vasculitic lesions Diarrhea, nausea vomiting may occur Neurologic symptoms (up to 16%) Encephalopathy, seizures, meningoencephalitis Acute flacid paralysis Guillan-Barre like syndrome Rarely: myocarditis, hepatitis, nephritis, anterior uveitis, retinitis, optic neuritis Mahendradas et al. J Ophth Inflam Infec 2013; 3:35 Burt FJ et al. Lancet 2012; 379:662-71 Thiberville, SD et al. PLOS Neg Trop Dis. 2013 Clinical features: Day 1, 7, 25 Joint disease Severe Arthralgias Polyarticular, usually symmetric, small joints Swelling but no large effusions Some improvement in 1-2 weeks, but may persist for years Malaysia retrospective review Mean duration of arthralgia 3 months 45% had arthralgias beyond 4 months 22% with arthralgias beyond 1 year Réunion: Persistence at 36 months Risk increases with age >35 years old Presence of arthralgia at 4 months was predictor of chronic disease Mouse models suggest due to viral persistence in tissues Zim MA et al. J Clin Virol. 2013; 56:141-45. Thiberville, SD et al. PLOS Neg Trop Dis. 2013 Schilte et al. Plos Neg Trop Dis. 2013 Hawman et al. J. Virology 2013; 87:13878 Diagnosis Differential Dengue Ross River virus, O’nyong-nyong and other alphaviruses Leptospirosis, malaria, group A strep, rickettsia, rubella, measles, parvovirus, enterovirus, adenovirus, rheumatologic diseases Clinical findings, epidemiology, lab confirmation Viral culture in 1st 3 days of illness RT-PCR for viral RNA in 1st 8 days Serology for IgM and IgG by end of 1st week Convalescent titers with four-fold increase in IgG Samples to CDC through CDPHE www.cdc.gov Treatment and Prevention Acute Illness Supportive care NSAIDS Case reports of short steroid courses for severe early disease Persistent arthralgias: no good data for treatment Chloroquine, hydroxychloroquine No sig difference in efficacy for acute arthralgias between chloroquine and meloxicam in 509 indiv in India Sulfasalazine, methotrexate, ribavirin, interferon-alpha Mosquito avoidance Vaccines in research, not licensed Monoclonal antibodies as prophylaxis effective in mouse models Mosquito avoidance on return home to prevent local transmission Chopra et al. Arthritis and Rheum 2012. Accepted Article, doi: 10.1002/art.38221 Chopra et al. Arthritis and Rheum 2008;9:2921-2 Selvarajah et al. PLoS Neg Trop Dis 2013;7:e2423 Janu et al. J. Assoc. Phys India 2011; 59:83-6 CHIKV: re-emerging disease Initial descriptions in 1950s 2006 Maldives 2000 Epidemic in Kinshasa, 2008 Singapore DRC, 1st in 39 years 2001-2003 epidemic in Indonesia, 1st in 20 years 2004 Coastal Kenya E226V mutation more efficiently transmitted by Aedes albopictus 2005 Spread to Comoros Islands 2005-2007 Epidemic in Réunion: 35% attack rate 266,000 cases 0.1% mortality 2012 Rural Cambodia 44.7% prevalence 5.3% asymptomatic 2012 Bhutan 1st cases reported Index case recent travel from India East/Central/South African genotype 2012 Papua New Guinea 1st cases reported MMWR 2012; 61: 737-40 www.cdc.gov/eid 2013 vol 19 CHIKV Epidemics 2005-2006 Re-emergence in India after 32 years 1.3 million cases in 13 states 2007 Northern Italy: Emilia-Romagna 254 locally acquired infections Index case just returned from India 2010 French Riviera: Frejús, Nice Index case young girl with recent return from India December 2013 Carribbean isle of St. Martin Dec 6th: 2 cases of locally acquired chikungunya 1st cases reported in the Americas Dec 10th: 2 confirmed, 4 probable, 20 suspected cases of chikungunya reported to WHO www.who.int/scr/don/2013_12_10a/en/index.html; accessed 1/12/14 Tomasello et al. Travel Med and Inf Dis 2013; 11, 274-284 CHIKV and US Travelers 1995-2009: 109 lab-confirmed cases in US Adult travelers, mean age 48 yrs 57% female Gibney et al. CID 2011; 0:1-6 CHIKV and Travelers 1995-2009: 109 lab-confirmed cases in US Adult travelers, mean age 48 yrs 57% female Gibney et al. CID 2011; 0:1-6 CHIKV Cases in the US Gibney et al. CID 2011; 0:1-6 US Distribution of Imported CHIKV Gibney et al. CID 2011; 0:1-6 Travelers from Indian Ocean Islands, 1997-2010 Savini et al., EID 2013; 19 Implications for Travelers Increased education regarding expanding geographic distribution of vectors for chikungunya (and dengue) virus, especially Europe and Caribbean Emphasis on need for mosquito avoidance in areas that are not tropical or traditional risk areas Prompt evaluation of return travelers with fever and awareness of CHIKV Avoidance of mosquitos after diagnosis of chikungunya to decrease risk of local transmission