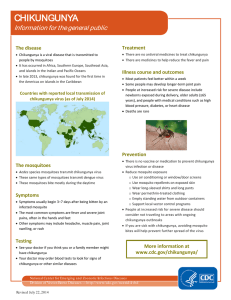
Chikungunya is a viral disease that is spread by mosquitoes. The virus is transmitted to humans by mosquitoes. The mosquito will pick up the virus when it ingests the blood while an uninfected mosquito feeds a viremic human someone with a virus circulating in their blood. The virus then undergoes a phase of reproduction in the mosquito, before which point, when the mosquito next feeds, it can then be transferred back to a young, naive host. In this newly infected human, the virus again starts to replicate and amplify to high concentrations. During the time when they have a virus circulating in their blood, if a mosquito feeds on them, the mosquito will pick up the virus, and the propagation period starts again (WHO, 2020). Two important vectors are Aedes aegypti and Aedes albopictus, which also transmit dengue virus. It is spread by the bite of the Aedes aegypti mosquito, which is also capable of spreading dengue and yellow fever, which is found in the tropics and sub-tropics of the Americas, and by the Aedes albopictus mosquito, which spreads from the eastern coast and southeast of the United States to the provinces of northern Argentina in more temperate regions. These mosquitoes are quickly identified by the white stripes across their legs; the propagation period starts when they bite a human with chikungunya furthermore when an Aedes mosquito bites someone with chikungunya when they have fever, the transmission period starts; 10 days later, the virus multiplies in the mosquito's salivary glands and is able to spread the disease when the mosquito bites a healthy person who begins to develop symptoms 3-7 days after incubation (PAHO, n.d.). Chikungunya is a mosquito-borne viral disease which causes the sudden onset of fever and severe joint pain (Litin, n.d.). The virus symptoms are close to those of other illnesses, such as dengue fever. The signs that are most prominent are: fever (sometimes as high as 104 °F), joint pain, headache, muscle pain, rash, swelling around the joints that usually occur only a few days after a person has been bitten by a mosquito and It causes a few days of fever and joint pain that can last for weeks or months. (Newman, 2017). The 39-40 ° C fever is also followed by chills and intermittent trembling. A "saddle-back" fever pattern can occur before fever develops again, an acute period lasting 2-3 d, remitting for 1-2 d. Joint activity is typically symmetrical, polyarticular, and migratory and primarily involves the elbows, wrists, ankles, and feet with small joints. 42 The wider joints are involved less often. It is likely to see periarticular swelling, discomfort, redness, and restriction of movement (Seneviratne et al., 2007). It is not always that Chikungunya disease results in death, although the symptoms can be extreme and debilitating. Within a week, most patients felt better. Those at risk of more serious illness include infected newborns at birth, elderly adults (aged 65 years or older), and persons with medical problems such as high blood pressure, diabetes, or heart failure. He or she is likely to be safe from potential infections after a person has been infected (CDC, 2018). Patients with extreme chikungunya fever requiring hospitalization appear to be elderly and have comorbidities that are separate risk factors for severe illness, such as cardiovascular, neurological, and respiratory conditions or diabetes. 49,59 As encephalopathy and encephalitis, myocarditis, hepatitis, and multiorgan failure, extreme chikungunya may manifest. In patients with chronic medical problems, these unusual variants may be lethal and usually occur. 60.61 Neonates are also at risk of significant neurological sign-related illness. The rate of infection in neonates born to viremic mothers and exposed to the virus at birth can be as high as 50%, leading to serious disease and encephalopathy, resulting in long-term neurological sequelae and poor outcomes (Galán-Huerta et al., 2015). Chikungunya's diagnosis is mainly clinical. It is necessary to deliberately check for alert signs in regions where the risk of dengue is high, with a detailed medical history and physical evaluation in addition to a full blood count and transaminases to assess the process and seriousness of the disease. (Beltrán-Silva et al., 2018) 1. The Chikungunya CHIKV test aids in the diagnosis of Chikungunya virus infection. A simple blood test is the Chikungunya CHIKV test. 2. It is a need to have Chikungunya CHIKV test because the virus is readily spread and, if not contained, has the ability to develop into an outbreak. Therefore, it is important to identify the virus at an early stage and take the appropriate precautions to ensure that it does not spread and cause casualties. 3. The other test that you might have along with Chikungunya CHIKV test are Qualitative Real-time RT-PCR and Antibody Tests (IgG, IgM). Qualitative Real-time RT-PCR is when the Chikungunya virus reverse transcriptase (RT)-PCR assay is used to detect CHIKV RNA when the signs have been seen for less than 8 days. This procedure will not be used later, as this RNA is not detectable after 1 week while the Chikungunya antibody test is administered after the signs have been seen for more than a week. The first synthesis of IgM (Immunoglobulin M) is shown, followed by IgG (Immunoglobulin G). 4. Your nutritional intake, lifestyle and any other existing drugs you are currently taking are the factors that may influence the test results. Results may also be inaccurate if the blood sample is obtained too early following infection. 5. The consequence is that the patient is infected with the Chikungunya virus when the Qualitative Real-time RT PCR is performed and the outcome is positive. In the other hand, it is not a definitive outcome if the result is negative, because the Chikungunya virus RNA is undetectable after a week. Therefore, in order to get a definitive response, the antibody test should be run. 6. There are four potential results when the Antibody test is performed. Both IgM and IgG are negative: this could be a sign that the Chikungunya virus has not been transmitted to the patient. In order to validate the diagnosis, however, the procedure must be carried out again within a few days: IgM and IgG are both positive: this means that the patient has been exposed to the infection in the past or quite recently and must be monitored for the symptoms: IgM is positive while IgG is negative: this indicates a new Chikungunya virus infection. In order to validate this diagnosis, the patient must be examined again after 5 or 10 days and IgM is negative while IgG is positive: this means that antibodies to the Chikungunya virus occur and therefore supports previous infection. 7. Up to eight hours before the exam is performed, you will be asked to stop eating or drinking. Doctors should also be aware of other examinations in the near history that you have taken. The effects of the test can be influenced by certain substances, such as hazardous substances. Currently, there is no specific medication or available vaccine to combat against the chikungunya virus. Treatment for chikungunya only focuses on symptom relief rather than completely eliminating the source. For pain relief, over-the-counter medicines such as ibuprofen, diclofenac, naproxen, or aceclofenac can be taken along with acetaminophen or paracetamol. Doctors would often recommend adequate fluid intake and plenty amounts of rest as an integrative approach. Similar to dengue, chikungunya patients are advised to avoid aspirin intake or non-steroidal anti-inflammatory drugs (NSAIDs) until dengue diagnosis is ruled out. Aspirin causes a negative effect on the platelets and consuming these medicines might cause risks of bleeding. Physical and local measures is encouraged such as active and passive movements, which is always made gently to avoid causing pain (Simon et al., 2015). Certain studies display the role of chloroquine phosphate and hydroxychloroquine, though there are not enough evidences and have been showing inconsistent effects. Although some options are being evaluated, such as the use of recombinant antigens, chimeric alphaviruses, electroporated DNA, and CHIKV attenuated by large-scale codon reencoding, no vaccines are currently available (Thiberville et al., 2013).Though there is still no commercial vaccine available, a phase 2 clinical trial of the chikungunya is currently being funded by the National Institute of Health (NIH) which consists of VLPs or virus-like particles that are said to help stimulate immune responses. Other vaccine strategies are still under clinical trials and will reach several more years before its licensing and availability to the public. Mosquitos, being the modes of transmission of CHIKV, are to be kept away from. The risk of transmission of chikungunya virus is the result of simultaneous presence of the mosquito vectors Aedes aegypti and/or Aedes albopictus, presence of the virus and susceptible population (ECDC, n.d.). A CHIKV patient must also protect their bodies from being in contact with mosquitos especially during the 1st week of infection, as the virus can be transmitted from an CHIKV patient to a mosquito, and the mosquito may spread the virus to other people through mosquito bites. The proximity of mosquito vector breeding sites to human habitation is a significant risk factor for chikungunya as well as for other diseases that Aedes mosquito species transmit (WHO, 2020). The Aedes mosquitos breed in domestic settings such as flower vases, water storage containers, desert coolers, etc. and peri-domestic areas such as construction sites, coconut shells, discarded household junk items (vehicular tires, plastic and metal cans etc.), adult mosquitos rest in cool and shady areas in domestic and peri-domestic settings and bite human beings during daytime (WHO, 2009). For prevention and control, wearing clothing with long sleeves that covers as much skin as possible is highly recommended. Use of insect repellant with the advised ingredients like DEET and picaridin and use of essential oils such as thyme, lavender, and lemon eucalyptus oil work in driving off mosquitos. Other methods of minimizing contact with them are using of mosquito nets, mosquito coils and insecticide vaporizers. During outbreaks, insecticides may be sprayed to kill off flying mosquitos, applied to surfaces and around containers where the mosquitos land, and used to treat water in containers to kill the immature larvae (WHO, 2020). Use of air-conditioners fend off mosquitos from coming near. Overall, protecting yourself from getting mosquito bites is the best way for prevention.