- Lectures
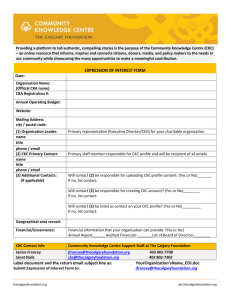
advertisement
Essential Considerations in Designing a Rehabilitation Program for the Injured Patient Chapter 1 Introduction • Rehabilitation of athletic injuries through programs utilizing progressive therapeutic exercises is a responsibility of the sports medicine team, emphasizing the skills and knowledge of the therapist.. Philosophy of Sports Medicine Rehabilitation • Key words – – – – Aggressive Quick return to play (RTP) Safety “Balancing Act” • Finding the balance between to much exercise and not enough exercise Philosophy of Sports Medicine Rehabilitation • What sports medicine professional need to understand – Types of injuries – Healing process – Pathomechanics of injuries and illnesses • Etiology – Cause of disease/injury • Pathology – Study of nature/causes of a disease which involves changes in structure and function – – – – Psychological aspect of rehabilitation Available tools and resources Therapeutic exercise vs. conditioning exercises Protocols Types of Injuries • Macro vs. microtrauma – Macro • • • • Sprains (ligaments) Strains (muscles) Fractures (bones) Contusion (soft-tissue and bone) – Micro • Stress fractures • Tendonitis Healing Process • Altering a therapeutic exercise or conditioning program is primarily dependent upon understanding the different phases the body goes through while healing • Therefore, sports medicine professionals must try to create an environment conducive to the healing process Healing Response • Bodies mechanism to rid the body of damaged tissue • Immediate response to acute injuries • Non-specific to site or stimulus • Essential for tissue repair • Divided into three process – Acute inflammation, proliferation (fibroblasticrepair) & maturation (maturation-repair) Healing Response Inflammation • Initial injury to body – Microtrauma or macrotrauma • Used to protect, localize, and rid the body of injurious agents • Includes a number of vascular, cellular and cellular changes – cell membrane permeability and edema formation – Phagocytosis • Concerned w/ 2nd death of tissue – Secondary hypoxic injury • Cardinal Signs of Inflammation – Heat and redness • BF and cell metabolism to traumatized tissue – Swelling • Loss of continuity of vascular structures • Chemical mediators – Pain • Chemical mediators • Swelling – Loss of function • Combination of the above Healing Response Proliferation • Marked by the removal of the cellular debris and the creation of a vascular network to support new tissue growth • Rate of proliferation phase in influenced by several factors include cell type, health, age, nutrition • Looking for the regeneration and restoration of the destroyed/lost tissue, however most tissue will never be identical to the traumatized tissue • May last 48-72 hrs up to 6 weeks after inflammatory phase • May begin after 2nd tissue death and cell debris has been cleaned Healing Response Maturation • “Cleaning-up” period • May last up to a year or more • Fibroblasts, myofibroblasts, macrophages are reduced to pre-injury state • Scar begins to fade as the extra capillaries and water are moved from the area • Need to keep encouraging re-organization & tensile stress to the tissue Healing Process • SAID Principle – Specific Adaptation to Imposed Demands • “When an injured structure is subjected to stress and overloads of varying intensities, it will gradually adapt over time to whatever demands were placed upon it”` – In some situation failure to do this leads to injury – Therefore, exercise intensity must be equal to the healing phase Pathomechanics • Injuries result in changes to the normal joint arthokinematics and osteokinematics • Therefore, sports medicine professionals need to have adequate knowledge in structural mechanics and how the structures will react to these changes Psychological • This stage is often the most neglected • Injuries/illnesses produce a wide range of emotions and how an individual and/or athlete reacts will affect his/her interpretation and reaction to pain, cooperation, compliance, denial, etc Tools • Sports medicine professional should try to have knowledge of things such as: – Basic first aid principles, understanding of the differences between different types of exercises based on the phase of tissue healing, how and when to progress an athlete, modalities, ortho evaluation skills • Athletes differ in their response to rehabilitation therefore avoid “cookbook” or “recipe” approach • Do what is right and not what is seen. Strict application of knowledge and using all knowledge separates a great therapist from everyone else Therapeutic Exercise vs. Conditioning Exercise • Therapeutic exercise – Any kind of movement of any of the body parts to rehabilitate to optimal function and to reduce symptoms – Problem orientated • Conditioning exercise – Used to maintain cardiovascular and physical fitness to avoid injury • Need to consider the affects of each of these on the types of exercise – Effects on muscles – Effects on joints – Effects on cardiorespiratory system Goals of Rehabilitation • Provide correct/immediate medical intervention to limit or minimize swelling and injury • Decrease or minimize pain • Restore full ROM • Restore or increase strength, endurance, and power • Re-establish neuromuscular control • Increase balance and proprioception awareness • Maintain cardiovascular endurance • Functional progression Therapeutic Exercise Template Every Assignment/Test *You now have the keys to modalities & Ther X • • • • • • • • • Modalities – Pain/Edema – Neurological functioning Scar tissue formation Joint Mobs, distraction, myofascial release ROM Flexibility /restore Balance/Gait training Establish core stability Postural stability/balance Restore/increase strength – atrophy, hypertrophy • • • • • • Restore or increase endurance Restore or increase power Reestablish neuromuscular control Restore/ balance & proprioception Maintain/ cardiovascular endurance Functional exercise/progression – • • • Multiple planes Modalities – As needed Functional testing Return to activity testing Keys – Daily SOAP Note Every Assignment/Test • Subjective – How does the patient feel, NSAIDs/drugs, Pain level, residual pain • Objective – Short term/long term goals – List entire treatment in detail. Ortho special tests, modality settings/time, exercise, sets/reps/weight, duration • Assessment – How did the patient react to the treatment. Specific problems, effort, adherence, special tests/documentation as needed • Plan – Add, delete, or continue rehab plan. Special test or measurements to be done in the future. Why Document Using SOAP • • • • • Legal ramifications Communication Organization Professionalism Patient motivation – Review goals – Review objective data progress Goals of Rehabilitation Inflammation • Prevent new tissue disruption using PRICE – Protection • Splints, pads, immobilization if necessary – Restricted Activity (Rest) • Research has shown that complete mobility can be bad, rather controlled mobility may aid in reducing scar formation, revascularization of tissue, muscle regeneration and reorientation of muscle fibers and tensile strength – Ice • Decreases pain & promotes vasoconstriction, thereby controlling hemorrhage & edema – Decreases 2nd tissue death – Decreases muscle spasms and provides an analgesic effect – Used in the treatment of bursitis, tenosynovitis, and tendonitis Goals of Rehabilitation Inflammation – Compression • Most important factor in controlling swelling – Purpose is to mechanically reduce the amount of space available for swelling by applying pressure around the injured area – Wrap distal to proximal – Elevation • Eliminates the affects of gravity on blood and other fluid pooling in an extremity – Assists in venous and lymphatic drainage – Greater the degree of elevation the more effective it is in reducing swelling Goals of Rehabilitation Proliferation • Goals is to prevent muscle atrophy and joint deterioration while preventing destruction of new tissues • Begin to apply low-load stress to prevent a loss of joint motion, however need to because about the amount of load and point of application • Continue to maintain cardiovascular and cardiorespiratory function Goals of Rehabilitation Maturation • Optimizing tissue function is the primary goal during the final phase of healing • Include the addition of functional and sportsspecific activities, however, still need to maintain the balance between too much and not enough Exercise Strategies Proliferation • Major goal is to work through “full pain-free ROM” • Accomplished through the use of: – Isometric exercise • Submaximal • However, they are joint angle specific – Isotonic • Movement with a constant external resistance – Gravity – Resistance bands – Dumbbells – Weight machines – Proprioception • Refers to conscious and unconscious appreciation of joint position Exercise Strategies Maturation • Focus is placed on: – – – – Functional activities Sport-specific exercises Closed and open chain exercises Exercises to improve proprioception Closed vs. Open Chain • Panaereillo defines CKC as – “activity of the extremities as an activity in which the foot or hand is in contact with the ground or a surface.” – Emphasizes that the body weight must be supported for a closed-kinetic chain to exist • Note: Few exercises can be absolutely classified as open or closed chain kinetic exercises • Most such as running and jumping fall somewhere in between Closed vs. Open Chain Characteristics • • • • • • CKC Joint compression force Joint congruency (stability) Shear force Acceleration force Larger resistance force Stimulation of proprioceptors OKC • • • • • • Distraction and rotational forces Deformation of joint and muscle mechanoreceptors Acceleration forces Resistance force Concentric acceleration and eccentric deceleration forces Promotion of functional activity Closed vs. Open Chain CKC Advantages • Safer and produces stress and force that are potentially less of a threat to the healing tissue • Muscular co-activation – required for joint stabilization • Decrease in shear force, caused by muscular coactivation • Lower extremity activities tend to be more functional in nature • Requires synchronism of the agonist and antagonist Closed vs. Open Chain OKC Advantages • Motion isolated to a single joint within a specific plane • Used to improve strength and ROM • Applied to single joint manually as in PNF and joint mobilizations or threw some type of machine • Isokinetic exercises are an example of open chain exercises Guidelines for Progression of CKC Exercises • • • • • • • • • Static stabilization dynamic stabilization Stable surface unstable surface Single plane movements multi-plane movements Straight planes diagonal planes Wide base of support small base of support No resistance resistance Fundamental movements – dynamic movements Bilateral support unilateral support Consistent movements perturbation training Functional Progression/Functional Testing • Functional Progression – Gradually helps achieve normal pain-free ROM – Helps to restore adequate strength levels – Helps to regain neuromuscular control and balance • Functional Testing – Uses functional progression drills to assess the athlete’s ability to perform a specific activity Developing Relationships • Developing and working with rehabilitating athletes requires – Communication between all involved parties • Do not be afraid to consult others – The Power of Consultation – Understanding all individuals’ rehabilitation philosophies (AT, MD, Athlete, etc) – Continually working to improve and re-assess the athletes functional status – ABOVE ALL ELSE “DO NO HARM” Specific Closed Chain Exercises Lower Extremity Exercises • Mini-squats / Wall slides / Lunges – Involves simultaneous hip and knee extension and is performed between 0-40° • 60-90° increases tibial translation compared to OKC exercises – Concurrent shift helps minimize the flexion moment at the knee – Half squat produces less shear at the knee than OCK exercises in full extension – Slight flexion flexion of the trunk anteriorly helps to increase hip flexion moment and decrease knee moment Lower Extremity Exercises • Leg Press – Utilize the CKC, while providing stability and decreasing strain on low back – Allows for lower resistance and unilateral exercises – Recommend from 0-60°, utilizing full hip extension • Lateral Step-Ups – Adjusted to the needs of the athlete and progress up to 8 in. – Generate significantly more quad activity Lower Extremity Exercises • Stair-Climbing – Steeping machines are true CKC exercises – Body should be held erect with slight trunk flexion – EMB studies have show that the gastrocnemius fires considerably • Terminal Extension with Tubing – Anterior tibial translation occurs between 0-30° of flexion – Application of resistance anteriorly at the femur produces anterior shear of femur, eliminating anterior translation of the tibia – Tubing produces an eccentric contraction of the quad when moving into knee flexion Lower Extremity Exercises • Bike – Utilized for cardiovascular, strengthening, and ROM – Toe clips facilitate HS contractions on the upstroke • BAPS Board and Mini-tramp – Provide unstable base – Allows simultaneous work for strength and ROM while regain NMC and balance • Slide Board and Fitter – Weight shifts and more functional activities – Re-establishes dynamic control Upper Extremity • Glenohumeral joint force couples must be re-established – Anterior deltoid along with the infraspinatus and teres minor in the frontal plane – Subscapularis counterbalanced by the infraspinatus and teres minor in the transverse plane • Scapulohumeral rhythm is also necessary to ensure proper positioning of the scapula during motion – Force couple between the inferior traps and upper trap and levator scaupla – Rhomboids and middle traps counterbalanced by the serratus anterior Upper Extremity • CKC GH joint exercises are used during the early phases of rehabilitation, especially with unstable shoulders to – Promote co-contraction and muscle recruitment and preventing shut down of the RC 2nd to pain and inflammation • Also used in later stages to: – Promote muscular endurance and stability (Dynamic and ballistic motions) OKC & CKC Exercises for the GH Joint Phase CKC OKC Acute Isometric press-up, push-up, and strengthening; WB shifts; axial compression against wall Subacute Resisted wall circles and wall abduction/adduction; slide board; pushups; PNF Isotonic and isokientic strengthening Chronic Push-ups on balance board; lateral stetups; shuttle walking; Stairmaster; plyometric push-ups Isotonic and isokinetic strengthening; plyometrics; sport-specific training OKC & CKC Exercises for the Scapulothoracic Joint Phase CKC OKC Acute Isometric punches, strengthening, and press-ups Isotonic strengthening Subacute Push-ups, military presses, press-up Isotonic and isokinetic strengthening, rowing, prone horizontal abduction Chronic NMC drills, rhythmic stabilization, circles, Progression of isotonic diagonal patterns strengthening exercises Upper Extremity • Weight Shifts – Used to facilitate GH and ST dynamic stability – Done in standing, quadruped, tripod, or biped moving from stable to unstable – Movements are from side to side, front to back, and diagonal – Progress from a wide base to a small base – Provide resistance to stimulate rhythmic stabilization (Used also to regain NMC of scapular muscles with the hand in a CKC and random pressure applied to the scapula border) Upper Extremity • Push-ups, Push-Ups with a Plus, Press-Ups and Step-Ups – Push-ups and press-ups are done to regain NMC – Push-ups with a plus are done to strengthen the serratus anterior which is critical for dynamic stability in overhead activities – Press-ups (sitting on the table and lifting body weight up) involves isometric contraction of the GH stabilizers Upper Extremity • Slide Board – Promote strength and stability and improves muscular endurance • Hands move forward, side to side, wax-on-wax off Upper Extremity Immediately after GH joint subluxation or dislocations • Acute – Isometric press-up & isomeric weight bearing & shifts, axial compression against a table or wall • These movements produce joint compression and approximation which enhances muscular co-contraction about the joint, leading to dynamic stabilization • Sub-acute – Resistance is applied to the distal segment • Include resisted arm circles against a wall, resisted axial load side to side either against a wall or on a slide board, and push-ups • Resistance can be applied in different amounts to multiple positions Upper Extremity Immediately after GH joint subluxation or dislocations • Advanced – Weight bearing exercises are usually high-demanding movements that require a tremendous degree of dynamic stability • Push-up with the hands on a ball, which produces axial load on the joint but keeps the distal segment somewhat free to move (additional unstable foot platform) • Lateral step-ups using the hands and retrograde lateral walking on the hands on a treadmill or stair steppers • Requires a fair amount of dynamic stability and strength Exceeding Healing Tissue Strength • Pain • Swelling • Loss/plateau of strength • Loss/plateau of ROM • Increase in joint laxity • When do I increase weights or difficulty of therapeutic exercise plan? – Refer to left