Malabsorption syndrome
advertisement

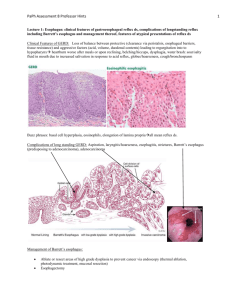
Malabsorption syndrome By: Dr. Elias S. Dr. Maruf A Malabsorption Impaired absorption of one or more dietary nutrients Dietary nutrient absorption –in small b. Ca., iron, folic acid – absorbed in proximal SB Cobalamine, bile acid – in the ileum Glucose, a.a., lipids – throughout the SB Malabsorption could be: A pathophysiologic state with multiple etiologies/varied clinical manifestations Primary (congenital defects) Secondary (acquired defects) Clinical Sx usually due to: Malabsorption of fat &/or carbohydrate (with water & electrolyte Mal.) Steatorrhea main feature in most cases Nutrient malabsorption Intestinal secretion Diarrhea Steatorrhea Watery D. Inflammatory D. Inflammation mechanisms 1. Luminal phase (processing defect) 2. Mucosal phase 3. Digestive enzyme deficiency / inactivation bile salt synthesis; Excretion; loss; bile salt de-conjugation gastric acid; intrinsic factor (p. anemia) Bacterial consumption of nutrients Epithelial transport defect – inflammations infections Brush border hydrolysis defect congenital/acquired disacharidase deficiency Post-absorptive phase Enterocyte processing – Abetalipoproteinemia Lymphocytic obstruction – intestinal lymphangectasia causes Exocrine pancreatic insufficiency ch. Pancreatitis pancreatic CA cystic fibrosis Inactivation of pancreatic lipase – Gastrinoma(ZES) drugs (orlistat) bile acid (impaired micelle formation) parenchymal liver D. cholestatic liver D. Bacterial overgrowth Anatomic stasis (blind loop,stricture,fistula) Functional stasis (DM, scleroderma) Interrupted interohepatic circulation of bile acid (ileal resection, crohn’s D.) Drugs(bind or precipitate bile salt) neomycin, chlestyramine Impaired mucosal absorbtion/ mucosal loss or defect intestinal resection or bypass inflammation/infiltration/infect. (celiac sprue, tropical sprue, whippl’s disease, lymphoma, mastocytosis, eosinophilic e., scleroderma, crohn’s D., …) Impaired nutrient transport lymphatic obstruction (lymphoma, lymphangectasia) CHF Genetic disorders disacharidase defficiency Agamaglobulinemia Abetalipoprotinemia Endocrine/Metabolic disorders DM Hyperthyroidism adrenal insufficiency carcinoid syndrome Clinical features Depend on the cause and severity Glabal Diffuse mucosal involvement Impaired absorption of all nutrients Classic manifestation Diarrhea(steatorrhea) weight loss Majority – sub clinical E.g.. Celiac disease Partial (isolated) 2° to diseases that interfere with absorption of specific nutrients E.g.Pernicious Anemia Lactase deficiency Signs & symptoms Calori Weight loss with normal appetite Fat Pale,voluminous,greasy offensive diarrhea Protein Edema, muscle atrophy, amenorrhea carbohydrate Abdominal bloating, flatus, w. diarrhea B12 Macrocytic anemia Subacut combined degeneration of sp.cord Folic acid Macrocytic anemia Vit B (general) Cheliosis, glossitis,A.stomatitis, Acrodermatitis Iron Microcytic anemia Ca & Vit D Osteomalacea (bone pain,pathologic#), Tetany Vit A Follicular hyperkeratosis, Night blindness VIt K Bleeding diathesis, Hematoma Clinical Evaluation In 75-80% of cases • Dx by expert Hx & P/E + focused lab tests 25% - need extensive study/ Hospitalization Hx: • Diarrhea- duration, consistency, frequency stool characteristics, Volume time of occurrence, association with diet etc…. • Bloating,borborigmi, flatus • Abdominal pain • Sxs of extra intestinal manifestation (joint pain, mouth ulcer..) • Previous abd. Surgery • medication • Alcohol intake • Recurrent PUD • DM , CLD • Falmily Hx – celiac disease, crohn’s D.) • Risk factors – HIV infection P/E – thorough examination Look for signs of specific nutrient Malabsorption extraintestinal signs Lab. CBC, PT, serum protein, ALP Checks for depletion of iron,folate, B12, Vit D, Vit K) RFT,electrolytes Stool exam Additional tests: Serum carotene, cholesterol, albumin, iron, folate cobalamine Tests for steatorrhea Quantitative test 72hr stool fat collection – gold standard • > 6gm/day – pathologic • P’ts with steatorrhea - >20gm/day • Modest elevation in diarrheal disease (may not necessarily indicate Malabsorption) Qualitative tests Sudan lll stain • Detect clinically significant steatorrhea in >90% of cases Acid steatocrit – a gravimetric assay • Sensitivity – 100%, specificity – 95% , PPV – 90% NIRA (near infra reflectance analysis) • Equally accurate with 72hr stool fat test • Allows simultaneous measurement of fecal fat, nitrogen, CHO Schilling test To determine the cause of cobalamine(B12) malabsorbtio Helps to asses the integrity of gastric, pancreatic and ileal functions. • Abnormal cobalamine absorbtion in: pernicious anemia, ch. Pancreatitis, Achlorohydria, Bacterial overgrowth, ileal dysfunction The test • Administering 58Co-labeled cobalamine p.o. Cobalamine 1mg i.m. 1hr after ingestion to saturate hepatic binding sites • Collecting urine for 24 hr (dependant on normal renal & bladder function) • Abnormal - <10% excretion in 24 hrs Schilling test cont…. 58CoCbl Pernicious Anemia Chronic Pancreatitis Bacterial overgrowth Ileal disease With With 5 Days Intrinsic pancreatic Of Ab factor enzyme N N N D-xylose test D-xylose A Pentose monosacharide absorbed exclusively at the proximal SB Used to asses proximal SB mucosal function The test After overnight fast, 25gm D-xylose p.o. Urine collected for next 5 hrs Abnormal test - <4.5 gm excretion show duodenal / jejunal mucosal D. False +ve results: Renal dysfunction Inadequate urine sample Impaired gastric empyting, ascitis Drugs(ASA,indometacin, Neomycin) Othe tests for carbohydrate malabsorbtion Lactose tolerance test • P.o. 50gm lactose • Bloood glucose at 0,60,120 min. • BG <20mg/l + dev’t of Sxs – diagnostic Breath tests (hydrogen,4Co2,13Co2) Test for bacterial overgrowth Tests for pancreatic insufficiency Quantitative bacterial count from aspirated SB. Normal count: < 10 /ml (jejunum) > 10 /ml (ileum) Stimulation of pancreas through adm. Of a meal or hormonal secretagogues , then analysis of duodenal fluid Indirect tests – schilling test Tests for protein malabsorption Enteral protein loss measuring alpha-1 antitirypsin clearance Endoscopy Gross morphology – gives diagnostic clue Cobblestone appearance – crhon’s D. Reduced duodenal folds and scallopng of duodenal mucosa – celiac disease • Use of vital dyes to identify villous atrophy Biopsy – to establish Dx Lesions seen – classifid in to three For p’ts with documented steatorrhea or ch. Diarrhea Diffuse,specific e.g. whippl’s Disease Patchy, specific – crohn’s D., lymphoma infectious causes Diffuse,non-specific – celiac sprue, Tropical sprue autoimmune enteropathy Suspected distal pathology - push enteroscopy wireless capsule endoscopy Barium studies Important information about the gross anatomy and morphology of SB Upper GI series with SB follow through Enteroclysis • double contrast study by passing a tube into proximal SB and injecting barium+ methylcellulose Normal study doesn’t exclude SB disease