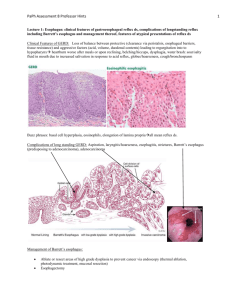
Bacterial overgrowth syndrome
advertisement
MALABSORPTION GROUP A MALABSORPTION SYNDROME Diminished intestinal absorption of one or more dietary nutrients Not an adequate final diagnosis Most are associated with steatorrhea Increase in stool fat excretion of >6% dietary fat intake APPROACH TO THE PATIENT Malabsorption HISTORY, SYMPTOMS AND INITIAL PRELIMINARY OBSERVATION Extensive small-intestinal resection for mesenteric ischemia Short bowel syndrome Steatorrhea with chronic alcohol intake and chronic pancreatitis Pancreatic exocrine dysfunction ACTIVE TRANSPORT OF SITE-SPECIFIC DIETARY NUTRIENT ABSORPTION Throughout Glucose, amino acids, lipids Proximal SI (esp. duodenum) Calcium Iron Folate Ileum Cobalamin Bile acids SI (Proximal>Distal) ADAPTATION Morphologic and functional Due to segmental resection Secondary to the presence of luminal nutrients and hormonal stimuli Critical for survival STEATORRHEA Quantitative hours) Gold standard Qualitative Sudan III stain Does not establish degree of fat malabsorption For preliminary screening studies Blood, stool fat determination (72 breath, and isotropic test Do not directly measure fat absorption Excellent sensitivity only with obvious steatorrhea Not survived transition from research laboratory to commercial application LABORATORY TESTING Vitamin D malabsorption Evidence of metabolic bone disease Elevated serum ALP Reduced serum calcium Vitamin K malabsorption Elevated prothrombin time Without liver disease No intake of anti-coagulants LABORATORY TESTING Cobalamin/Folate malabsorption Macrocytic anemia Iron malabsorption Iron deficiency anemia No occult bleeding from GIT Non-menstruating female Exclusion of celiac sprue Iron is absorbed in the proximal SI DIAGNOSTIC PROCEDURES Malabsorption DIAGNOSIS OF MALABSORPTION Effect of prolonged (>24h) fasting on stool output Osmotic diarrhea Decrease in stool output: Presumptive evidence that diarrhea is related to malabsorption Secretory diarrhea Persistence of stool output: Not due to nutrient deficiency STOOL OSMOTIC GAP Useful in differentiating secretory from osmotic diarrhea 2 x (stool [Na+] + [stool K+]) ≤ stool osmolality Normal: 290-300 mosmol/kg H20 Significant osmotic gap Suggests the presence of anions other than Na and K are present in the stool, presumably the cause of diarrhea Diff >50: osmotic gap present, dietary nutrient is not absorbed Diff <25: dietary nutrient is not responsible for the diarrhea Schilling Test Radiologic Examination -test for carbohydrate absorption -assessment of proximal small-intestinal mucosal function -evaluation of the patient with presumed or suspected malabsorption Procedure -performed by administering 58Colabeled cobalamin orally and collecting urine for 24 h - performed by giving 25 g D-xylose and collecting urine for 5 h -performed with the examination of the esophagus to duodenal bulb -insufficient barium is given to the patient Abnormal Findings <10% excretion in 24 h <4.5 g excretion Ex. strictures & fistulas (Crohn’s disease), - diminished use due to ease of obtaining a mucosal biopsy by endoscopy and falsenegative rate -abnormalities are rarely seen with current barium suspensions, skilled personnel required Use -determine the cause for cobalamin malabsorption -assess the integrity of stomach, pancreas, and colon Urinary D-Xylose Test - infrequently performed because of Disadvantage the unavailability of human intrinsic factor COBALAMIN ABSORPTION Dietary cobalamin in meat Bound to R-binder protein in stomach Complex bound in acid milieu in the stomach Uptake of cobalamin in receptors in brush border of ileal enterocytes Pancreatic protease enzymes split cobalamin and binding protein Cobalamin enters the proximal small intestine and binds to intrinsic factor SCHILLING TEST Pernicious Anemia Chronic Pancreatitis Absence of another factor secreted with acid that is responsible for splitting cobalamin from the proteins in food Bacterial Overgrowth syndromes Deficiency of pancreatic proteases to split the cobalamin-R binder complex Achlorydia Atrophy of gastric parietal cells lead to absence of gastric acid and intrinsic factor secretion Bacterial utilization of cobalamin Ileal dysfunction Impaired cobalamin – intrinsic factor uptake SCHILLING TEST 58Co-Cbl With Intrinsic Factor With Pancreatic Enzymes After 5 Days of Antibiotics Pernicious anemia Reduced Normal Reduced Reduced Chronic pancreatitis Reduced Reduced Normal Reduced Bacterial overgrowth Reduced Reduced Reduced Normal Ileal disease Reduced Reduced Reduced Reduced BIOPSY OF SMALL-INTESTINAL MUCOSA Essential in the evaluation of a patient with documented steatorrhea or chronic diarrhea Preferred method to obtain histologic material of proximal small-intestinal mucosa Indications: Evaluation of a patient either with documented or suspected steatorrhea or with chronic diarrhea Diffuse or focal abnormalities of the small intestine defined on a small-intestinal series BIOPSY LESIONS AND FINDINGS RESULTS OF DIAGNOSTIC STUDIES IN DIFFERENT CAUSES OF STEATORRHEA D-Xylose Test Chronic pancreatitis Normal Bacterial overgrowth syndrome Ileal disease Celiac sprue Normal or only modestly abnormal Normal Decreased Intestinal lymphangiectasia Normal Schilling Test Duodenal Mucosal Biopsy Normal 50% abnormal; if abnormal, normal with pancreatic enzymes Often abnormal; if Usually normal abnormal, normal after antibiotics Abnormal Normal Normal Abnormal: probably "flat" Normal Abnormal: "dilated lymphatics" DIFFERENTIAL DIAGNOSIS FOR CHRONIC DIARRHEA: APPROACH TO A PATIENT WITH MALABSORPTION CC: Diarrhea 1 month duration Prolonged fast (>24h) Osmotic Diarrhea (>50 osmotic gap difference) Secretory Diarrhea (<25 osmotic gap difference) Diagnostic Procedures i.e. biopsy of SI, Schilling test Diagnosis: Cause of Malabsorption DISEASE ENTITIES CAUSING MALABSORPTION CELIAC SPRUE Other names: Nontropical sprue, Celiac disease, gluten-sensitive enteropathy Etiology is not known Environmental – gliadin-associated Immunologic – IgA antigliadin, IgA antiendomysial, IgA anti-tTg antibodies Genetic – HLA-DQ2 allele Protean manifestations most of which are secondary to nutrient malabsorption Onset of symptoms occur at ages ranging from first year of life to eighth decade Clinical manifestations: Appear with the introduction of cereals in an infants diet ranges from significant malabsorption to multiple nutrients, diarrhea, steatorrhea, weight loss, consequences of nutrient depletion to absence of any GI symptoms but with evidence of a single nutrient depletion Hallmark: malabsorption and histologic changes Mechanism of diarrhea: Steatorrhea Secondary lactase deficiency Bile acid malabsorption Endogenous fluid secretion Associated diseases: Dermatitis herpetiformis (DH) DM type 1 IgA deficiency Complications: GI and non GI neoplasms Intestinal ulceration Refractory sprue Collagenous sprue TROPICAL SPRUE Affects 5-10% of population in some tropical area Etiology and pathogenesis is uncertain Clinical manifestations: Chronic diarrhea Steatorrhea Weight loss Folate and cobalamin deficiencies SHORT BOWEL SYNDROME General term for digestive problems that occur after a resection Depends on Segment resected Length of segment Presence of ileocecal valve Extent of colon removal Residual disease Generally, need to lose 2/3 of intestine Usually acquired Can be congenital in children Congenital short bowel After resection, intestine undergoes adaptation. SHORT BOWEL SYNDROME Clinical Presentation Diarrhea Steatorrhea Possibility of hyperoxaluria Increase in gallstone risk Increase in gastrin levels Pathophysiology Removal of Ileum Removal of ileocecal valve Bile unabsorbed Stimulates colonic fluid and electrolyte secretion Bacterial overgrowth Decrease in intestinal time Removal of intestinal mucosa Lactose intolerance Lipid, fluid and electrolytes are not absorbed SHORT BOWEL SYNDROME KEY POINTS Follows resection of intestines Generally inadequacy in absorbing food and fluids because of lack of surface area BACTERIAL OVERGROWTH SYNDROME Proliferation of colonic type bacteria within small intestine Clinical Manifestation Diarrhea Steatorrhea Macrocytic anemia BACTERIAL OVERGROWTH SYNDROME Pathogenesis Macrocytic Anemia Steatorrhea Etiology •Cobalamin deficiency •Increased bacteria = use more B12 •Impaired micelle formation Anatomical Stasis Direct Communication between SI and LI Functional Stasis Bacterial Overgrowth Diarrhea •Due to steatorrhea •Due to bacterial enterotoxins BACTERIAL OVERGROWTH SYNDROME KEY POINTS Macrocytic anemia Because of lack of B12 Stasis = allows bacteria to multiply WHIPPLE’S DISEASE Insidious in presentation Chronic multisystem disease Usually causes Clinical Manifestation Diarrhea Steatorrhea Weight loss Abdominal pain Arthralgia CNS/ cardiac problems WHIPPLE’S DISEASE Epidemiology More common in men Etiology and Pathogenesis Middle aged caucasian men T. whipplei Gram negative Rod shaped Presence of PAS (+) macrophages in SI lamina propria Fatal if left untreated Steatorrhea caused by SI mucosal injury Lymphatic obstruction WHIPPLE’S DISEASE KEY POINTS Rare, SYSTEMIC disease Insidious CNS and cardiac symptoms Dementia = POOR prognosis Caused by damage to mucosa and lymphatic obstruction PROTEIN LOSING ENTEROPATHY Group of diseases with Hypoproteinemia and edema WITHOUT Proteinuria/ kidney problems Protein synthesis defects/ liver problems Clinical Manifestation Peripheral edema Diarrhea Steatorrhea PROTEIN LOSING ENTEROPATHY Pathogenesis Etiology Excess protein loss in the GI tract Exceeds the normal 10% protein catabolism Non ulcerated mucosa group; altered permeability Mucosal Ulceration Group Lymphatic dysfunction Protein Losing enteropathy PROTEIN LOSING ENTEROPATHY KEY POINTS Peripheral edema, hypoproteinemia More than >10% total protein breakdown Proteins lost through exudates, altered permeability, lymphatic obstruction TREATMENT Disease Entity Treatment Celiac Sprue Complete dietary gluten restriction Dietary lactose and fat restriction for more severe cases Tropical Sprue Broad spectrum antibiotics and folic acid Tetracycline for 6 months Short Bowel Syndrome Opiates (codeine), Low fat high, high carbohydrate diet Fat soluble vitamins, folate, cobalamin, calcium, iron, magnesium, zinc Bacterial Overgrowth Syndrome Surgical correction on the anatomical blind loop Broad- spectrum antibiotics: Tetracycline, metronidazole, amoxicillin/clavulanic acid and cephalosporins Whipple’s disease Double strength trimethoprin/sulfamethoxazole for 1 year Alt: chloramphenicol Protein losing enteropathy Treat the underlying disease process Low fat diet and MCT’s for the treatment of hypoproteinemia