Dr Mark Cooper
advertisement
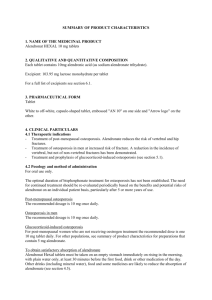
“Management of osteoporosis in primary care – can anything be learned from the UK experience?” Dr. Mark S Cooper Consultant Senior Lecturer in Endocrinology University of Birmingham Royal Orthopaedic Hospital and UHB Foundation NHS Trusts Overview Importance of osteoporosis Changing approach to how risk of osteoporotic fracture is estimated Evolution (and implosion) of guidelines for detecting and treating osteoporosis in the UK Implications for primary care when guidelines change e.g. if ways of assessing fracture risk change Osteoporosis disease continuum Kyphotic spine Healthy spine Menopausal Osteopaenic/ osteoporotic Postmenopausal woman without fracture Established osteoporosis Severe osteoporosis Postmenopausal woman Postmenopausal woman with 2 or more fractures with fracture Fractured Neck of Femur High morbidity and mortality, reduced independence, expensive to society Impact of osteoporosis - individual Approximately one in five patients die within a year as a result of their hip fracture Half who fracture a hip cannot live independently subsequently and 64% will need a walking aid 40% of patients with clinical vertebral fracture have constant pain, most have difficulty with daily living The reduction in quality of life from a vertebral fracture is half of that following hip fracture Impact of osteoporosis – health service More than 2 million hospital bed days are lost to fracture per year in England Mean length of stay 25 days, 1 in 5 orthopaedic beds occupied by patients with hip fracture Admission rate for fractured NOF has increased in England by over 2%/year since 1990 A conservative estimate for social/hospital cost of hip fracture is <£1.8 billion/year in the UK This is expected to rise to £2.1 billion by 2020 Definition of osteoporosis World Health Organisation: “A progressive systemic skeletal disease characterised by low bone mass and microarchitectural deterioration of bone tissue, with a consequent increase in bone fragility and susceptibility to fracture” Distinct from osteomalacia where there is normal amount of bone but inadequate mineralisation Consequence is an increased risk of fracture Normal versus osteoporotic bone Microarchitechture deterioration Low bone mass Normal Osteoporosis Operational definition of osteoporosis Risk factors for fracture • • • • • • • • • • Age Gender Prior Fracture Low BMD Parental history of fracture* Low BMI Current Smoking* Alcohol intake* Ever Corticosteroid use Secondary causes (e.g. RA, early menopause, coeliac disease) * Largely independent of BMD Previous emphasis almost entirely on BMD assessment. Can the factors that are independent of BMD be incorporated into guidelines? Incidence of Fracture per 100,000 Person-Years Relationship between osteoporosis and fracture Bone density Bone turnover Bone structure etc Fragility (falls “independent” fracture risk) FRACTURE Falls risk Evolution of UK guidelines RCP guidelines 2001 NICE – National Institute for Health and Clinical Excellence NICE Established in 1999 to address ‘post-code’ lottery Large disparities were present in access to medical services between regions in England (and rest of UK) Until then, general lack of health economic evaluation for medications NICE set up to evaluate whether treatments were cost effective relative to each other Funding for NICE approved (cost effective) medications should then be made available everywhere in England NICE In 2005 NICE produced guidance for secondary prevention of osteoporotic fracture Only applied to post-menopausal women, didn’t cover patients taking steroids Covered bisphosphonates, raloxifene, and teriparatide Extensive economic modelling to determine when drugs would be cost effective judged against NICE standards Calcium and vitamin D use recommended along with all treatments if possibility of deficiency of either Summary algorithm Teriparatide recommended: in women >65 years who have had an unsatisfactory response to, or are intolerant of, bisphosphonates and: • have an extremely low BMD (with a T-score of –4 SD or below), or • have a very low BMD (with a T-score of –3 SD or below) + multiple fractures (more than two) + 1 or more additional age independent risk factor Consequences of NICE guidelines 2005 General acceptance Debate about role of DXA scanning – needed or not? Requirement not to scan removed ‘post-code’ issue Teriparatide guidance resulted in access to this medication to those most at need. Primary Care Trusts were obliged to fund this if NICE conditions met However, access to treatment for other groups potentially reduced e.g. women at high risk of fracture that had not yet fractured (primary prevention) Review of NICE guidelines 2008 It was intended that NICE review secondary prevention guidelines in 2008 Also were to produce primary prevention guidance Since first guidelines were produced very little new effectiveness data published but cost of alendronate had fallen dramatically Stakeholders expected a corresponding improvement in cost-effectiveness of treatment BUT….. Secondary Prevention Guidance 2008 First Line Option – Secondary Prevention Alendronate is recommended as a treatment option for the secondary prevention of osteoporotic fragility fractures in postmenopausal women who have a T-score of −2.5 SD or below. In women aged 75 years or older, a DXA scan may not be required if the responsible clinician considers it to be clinically inappropriate or unfeasible. Alternative Treatment Options – Secondary Prevention In the secondary prevention of osteoporotic fragility fractures Risedronate and etidronate are recommended as first alternative treatment options in postmenopausal women: – Who are unable to comply with the instructions for the administration of alendronate – Who have a contraindication to or are intolerant of alendronate and – who also have a T-score, age and number of ‘independent clinical risk factors’ as indicated in the following table Age (years) No Clinical Risk Factor 1 Clinical Risk Factor 2 Clinical Risk Factors 50-54 Not recommended -3.0 -2.5 55-59 -3.0 -3.0 -2.5 60-64 -3.0 -3.0 -2.5 65-69 -3.0 -2.5 -2.5 70 or older* -2.5 -2.5 -2.5 * : For woman aged 75 years or older, a DXA scan may not be required if the responsible clinician considers it to be clinically inappropriate or unfeasible. Independent clinical risk factors = parental history of hip fracture, alcohol intake of 4 or more units per day, rheumatoid arthritis. Other Treatment Options – Secondary Prevention In the secondary prevention of osteoporotic fragility fractures Raloxifene and Strontium Ranelate are recommended as alternative treatment option in postmenopausal women: – – – Who are unable to comply with the instructions for the administration of alendronate and risedronate or etidronate Who have a contraindication to or are intolerant of alendronate and risedronate or etidronate Who also have a T-score, age and number of ‘risk factors’ as indicated in the following table Age (years) No Clinical Risk Factor 1 Clinical Risk Factor 2 Clinical Risk Factors 50-54 Not recommended -3.5 -3.5 55-59 -4.0 -3.5 -3.5 60-64 -4.0 -3.5 -3.5 65-69 -4.0 -3.5 -3.0 70-74 -3.0 -3.0 -2.5 75 or older* -3.0 -2.5 -2.5* * : For woman aged 75 years or older, with 1 or more independent clinical risk factor or indicators of low BMD has not previously had her BMD measured, a DXA scan may not be required if the responsible clinician considers it to be clinically inappropriate or unfeasible. Other Treatment Options – Secondary Prevention In the secondary prevention of osteoporotic fragility fractures Teriparatide is recommended as alternative treatment option in postmenopausal women: – Who have a contraindication to or are intolerant of alendronate, risedronate and strontium ranelate or who have an unsatisfactory response (another fragility fracture despite adherence for 1 yr and a BMD decline below pre-treatment baseline). and – Who are 55-64 years and have a T-score < -4.0 SD plus more than 2 fractures – Who are 65 years or older and have a T-score < -4.0 SD or a T-score < -3.5 SD and more than 2 fractures Secondary prevention 2008 overview Much more complicated guidance Use of risedronate, raloxifene and strontium more restricted in an age and risk factor dependent manner Teriparatide use now allowed for women age 55-65 if very high risk of fracture Primary Prevention Guidance 2008 Initial guidance was restricted only to generic alendronate In initial proposals it was indicated that only generic alendronate and etidronate would be evaluated If generic alendronate or etidronate not tolerated then no treatment should be offered After considerable protests, and an upheld appeal that other treatments should be evaluated revised guidance produced Revised guidance is not easy to summarise! First Line Option – Primary Prevention Alendronate is recommended as a treatment option for the primary prevention of osteoporotic fragility fractures in the following groups: Age (years) Minimum requirements of clinical risk factors and/or indicators of low BMD Dexa T-score Age 65 or younger One risk factor and an indicator of Low BMD T-score of −2.5 SD or below Age 65-69 One risk factor T-score of −2.5 SD or below Age 70-74 One risk factor or an indicator of Low BMD T-score of −2.5 SD or below Age 75 or older Two risk factors or indicators of Low BMD Not required if the clinician considers it inappropriate or unfeasible. Clinical risk factors = parental history of hip fracture, alcohol intake of 4 or more units per day, rheumatoid arthritis. Indicators of low BMD = low body mass index (defined as less than 22 kg/m2) and medical conditions such as ankylosing spondylitis, Crohn’s disease, conditions that result in prolonged immobility, and untreated premature menopause. Alternative Treatment Options – Primary Prevention In the primary prevention of osteoporotic fragility fractures Risedronate and etidronate are recommended as first alternative treatment options in: – women unable to comply with the instructions for the administration of alendronate – women who have a contraindication to or are intolerant of alendronate and – who also have a T-score, age and number of ‘independent clinical risk factors’ as indicated in the following table Age (years) No Risk Factor 1 Risk Factor 2 Risk Factors 65-69 Not recommended -3.5 -3.0 70-74 -3.5 -3.0 -2.5 75 or older -3.0 -3.0 -2.5* Clinical risk factors = parental history of hip fracture, alcohol intake of 4 or more units per day, rheumatoid arthritis. Other Treatment Options – Primary Prevention In the primary prevention of osteoporotic fragility fractures Strontium Ranelate is recommended as an alternative treatment option in: – women unable to comply with the instructions for the administration of alendronate and risedronate or etidronate – women who have a contraindication to or are intolerant of alendronate and risedronate or etidronate and – who also have a T-score, age and number of risk factors as indicated in the following table Age (years) No Risk Factor 1 Risk Factor 2 Risk Factors 65-69 Not recommended -4.5 -4.0 70-74 -4.5 -4.0 -3.5 75 or older -4.0 -4.0 -3.0 Raloxifene is not recommended as a treatment option for the primary prevention of osteoporotic fragility fractures in PMO. Criticisms of NICE guidelines Clinically perverse – if alendronate not tolerated in a patient then second line alternative almost certainly restricted unless patient waits until fractures or starts to consume excessive alcohol etc Using original health economic evaluation all these treatments were cost effective – model changed by NICE in multiple ways, all of which reduced reduced the cost effectiveness e.g. the evidence for hip fracture reduction with strontium accepted by the European Licensing Agency but rejected by NICE as a post-hoc analysis (this has recently been ruled unlawful by the Court of Appeal) Model assumes 100% compliance for side effects but 50% compliance for effectiveness etc, etc, etc Consequences of NICE guidelines No one uses primary prevention guideline because of their complexity and clinical perversity Follow up guidelines for men, younger women and steroid users stalled (abandoned?) as no ‘experts’ prepared to produce these in the context of current guidance As a result of ‘experts’ pointing out errors in analysis people who know about osteoporosis now excluded from NICE meetings relating to its evaluation or treatment Permanent lack of confidence in the role of NICE as an agency that judges cost-effectiveness fairly Primary care use of medications for primary prevention remains limited ACT4148 Comparison to Australian situation Health economic evaluation appears to be much more embedded in Australian system Evaluation judged by panel that appears to have sufficient clinical expertise available to avoid ‘clinical perversity’ evident in some NICE decisions It appears that the Prescriptions Benefits Advisory Committee does not try to develop its own guidelines (in contrast to NICE) Alternative approach to determining risk and guiding treatment WHO have introduced its own way of estimating fracture risk using information from large numbers of patients Most areas of the world are moving towards using this fracture risk algorithm (FRAX) Web based and easy to use Incorporates all the information and gives individual items appropriate weighting In UK output can be used to determine treatment (developed by National Osteoporosis Guidelines Group – NOGG) Implications of FRAX – reduced emphasis on spine fracture risk n=288 patients 73 Treatment Discordant 7 Lifestyle/ NOGG Treat 42 Treated/ NOGG Lifestyle 37 Osteoporosis spine 24 referred to Metabolic clinic 5 Disagree NOGG (4 Treat/NOGG lifestyle) 6 No Information 13 Agree NOGG (7 Treat/6 lifestyle) Conclusions UK NICE guidelines for osteoporosis emphasise the use of alendronate in patients at increased risk of fracture Attempts by NICE to incorporate fracture risk estimates that go beyond BMD problematic, difficult to use and hard to justify when accurate fracture risk estimation tools now available Other osteoporosis drugs can be used if alendronate intolerant but differing thresholds present difficulties in patient encounters Long term, use of FRAX and NOGG thresholds more likely to have more impact