OSTEOPOROSIS and
fracture risk
Prof. J. Preželj
KO za endokrinologijo, diabetes in presnovne bolezni
Composition of bone
extracellular matrix:
30 %
70 %
organic – colagen typ 1 (osteocalcin, osteopontin etc)
anorganic (Ca, P) – hydroxy apatite
bone cells:
osteoblasts
osteoclasts
osteocytes
bone architecture:
trabeculae
normal bone turnover
•
• quiescence
quiescence
osteoid
mineralisation
• resorption
• formation
• cleansing
“COUPLING”
interleukins
osteoblast
osteoclast
resorption products
RANK/RANKL/OPG SYSTEM
preosteoblast
Physiological control of
resorption/formation balance
(hormones, factors):
PTH, PTHrP, GK, TNF,
Il-1,6,11, 17, PGE2…
preosteoclast
“up” or “down”
regulation of expresion
osteoblast
osteoclast
“bone quantity”
(BMD)
“bone quality”
• turnover
• collagen structure
• microarchitecture
• etc.
bone strenght
Osteoporosis is a skeletal disease…
…characterized by low bone mass and and micro
architecural deterioration of bone tissue with a
consenquent INCREASE IN BONE FRAGILITY (bone
strenght is reduced) and susceptibility to FRACTURE.
AGE
MENOPAUSE
70 years
MOST FREQUENT OSTEOPOROTIC FRACTURES
BMD
≈
BMD
BMD
≈
BMD
≈
bone strenght
bone strenght
bone strenght
bone strenght
quality
≈
quality
≈
quality
quality
fracture risk: NORMAL
fracture risk: INCREASED
fracture risk: INCREASED
fracture risk: VERY HIGH
BMD
bone strenght
quality
Indirect estimate of quality through ..
… data validated through extensive
epidemiological research:
age sex weight
height
parent fracture hip
previous fracture
glucocorticoids
current smoking
rheumatoid arthritis secondary osteoporosis
alcohol > 3 units per day
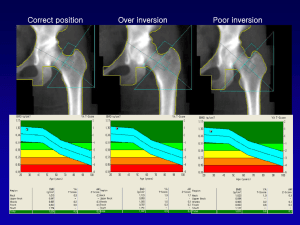
DXA
scan
(femoral neck BMD)
BMD (T – score)
T> -1,0
-1,0 > T > -2.5
T < -2,5
result
normal
osteopenia
osteoporosis
Ten year fracture probability (%)
Computer
based
algorithm
FRAX
Guidelines for starting therapy in high risk patients
Postmenopausal women
I. previous fragility fracture(s) of vertebrae or hip
exclusion of 2nd osteoporosis
Th
II. combination of age and T score < -2.5 (over L1-L4 and/or neck and/or total hip)
T - score
Age (years)
- 4.5
- 4.0
- 3.5
- 3.0
- 2.5
- 2.0 - 1.5
- 1.0
- 0.5
50 - 59
60 - 64
65 - 70
> 70
exclusion of 2nd osteoporosis
TM
FRAX
Th
III. fracture risk > 20/5 %
fracture risk < 20/5 %
Th
preventive measures
!!!
Če T < - 2.5
“laboratory is obligatory”
S - Ca,
S - A. PHOSPHATASE
SR (U - proteins, S - proteinogram)
S - creatinin, S - urea
S - AST (GOT), S - ALT (GPT), S - gama GT
hemogram
S-P
S - TSH
Therapy (reducing fracture risk)
Drugs
Calcium and vitamin D
Lifestyle changes
Therapy (reducing fracture risk)
Ca in foods
+ Ca supplements = 1200 mg Ca
1 dl milk
≈ 120 mg Ca
100 g cheese ≈ 1000 mg Ca
100 g curd cheese ≈70 mg Ca
Others:
women ≈ 250 mg
men ≈ 350 mg
1 g CaCO3
≈ 400 mg Ca
1 g Ca citrate
≈ 240 mg Ca
1 g Ca lactogluconate ≈ 90 mg Ca
Drugs
Calcium and vitamin D
Lifestyle changes
Therapy (reducing fracture risk)
ANTIRESORPTIVES
ANABOLICS
COMBINED ACTION
Drugs
Calcium and vitamin D
Lifestyle changes
Drugs for reducing fracture risk
ANTIRESORPTIVES
DRUG
DOSE
APPLICATION
EVISTA (raloksifen)
60 mg tbl/d
p/o
FOSAVANCE 5600 (alendronate + vitD3)
70 mg tbl/week
p/o
ACTONEL 75 MG (risedronate)
75 mg tbl/2 consecutive days/month
p/o
ACTONEL COMBI 75 MG (risedronat +
1000 Mg Ca + 880 IU vit D)
35 mg tbl/ week + (Ca + vit D) granula/d
BONVIVA (ibandronate)
150 mg tbl/month
p/o
p/o
BONVIVA IV (ibandronaet)
3 mg in 3 ml/ 3 months
i.v.
ACLASTA (zoledronic acid
5 mg in 100 ml/ year
i.v.
PROLIA (denosumab)
60 mg / 6 months
s.c.
PROTELOS (strontium ranelate)
COMBINED
FORSTEO (teriparatide)
2 g granula/d
ACTION
ANABOLIC
20 μg /d
p.o.
s.c.
How to prescribe antiosteoporotic therapy?
AMERICAN COLLEGE OF PHYSICIANS
We recommend that the choice of therapy be guided by judgment of the
risks, benefits, and adverse effects of drug options for each individual
patient.
hip fracture
comorbidity
PTH
HRT
risk
bisphosphonates
age
patient expectations
reimbursement
QUESTIONS ?