Aphasia Treatment Evidence-based Practice – The State
advertisement

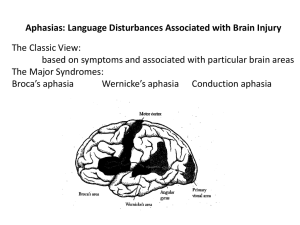
Aphasia Treatment Evidence-based Practice – The State of the Evidence Janet Patterson, Ph.D., CCC-SLP VA Northern California Healthcare System Martinez CA and California State University East Bay Hayward CA Session One Evidence-based Practice Aphasia Treatment Impairment-based Treatment Objectives – List principles of Evidence-based Practice – Identify a system for evaluating strength of evidence – Identify evidence for impairment-based treatment techniques 2 Neurophysiology and Neurogenic Speech and Language Disorders Join ASHA Division 2 and receive these affiliate benefits: • CEUs when reading Perspectives; 4 issues filled with cutting edge clinical and research information • 50% off select Division-sponsored Short Courses at Convention • Networking with colleagues on the listserv and regional resource clinicians • Other CEU opportunities at a discount • Access to affiliate-only web pages All for only $35 for ASHA members NSSLHA Students join for only $10.00 To join, contact the ASHA Action Center at 1-800-498-2071. Academy of Neurologic Communication Disorders & Sciences The purposes are professional, clinical, educational, scientific and charitable, and are ultimately to encourage the highest quality of life for individuals with neurologic communication disorders. Evidence-based Practice Evidence-based medicine is the integration of best research evidence with clinical expertise and patient values. (Sackett et al. Evidence-Based Medicine: How to Practice and Teach EBM, 2nd edition. Churchill Livingstone, Edinburgh, 2000, p.1) EBP components The goal of EBP is the integration of: (a) clinical expertise, (b) best current evidence, and (c) client values to provide high-quality services reflecting the interests, values, needs, and choices of the individuals we serve. http://www.asha.org/members/ebp/intro.htm Finding the evidence • ASHA National Center for Evidence-Based Practice (N-CEP) – http://www.asha.org/Membe rs/ebp/default/ • ASHA Division 2 – http://www.asha.org/membe rs/divs/div_2.htm • ANCDS – www.ancds.org • Agency for Healthcare Research and Quality – http://www.guideline.gov/ • The Cochrane Collaboration – http://www.cochrane.org/ • Centre for EvidenceBased Medicine – http://www.cebm.net/ SORTing the Evidence • Patient-oriented evidence measures outcomes that matter to patients: morbidity, mortality, symptom improvement, cost reduction, and quality of life. • Disease-oriented evidence measures intermediate, physiologic, or surrogate end points that may or may not reflect improvements in patient outcomes (e.g., blood pressure, blood chemistry, physiologic function, pathologic findings). Grading the Evidence Strength of Recommendation The strength (or grade) of a recommendation for clinical practice is based on a body of evidence (typically more than one study). This approach takes into account the level of evidence of individual studies; the type of outcomes measured by these studies (patient-oriented or disease-oriented); the number, consistency, and coherence of the evidence as a whole; and the relationship between benefits, harms, and costs. Ebell, Siwek, Weiss, Woolf, Susman, Ewigman & Bowman (2003) Strength of recommendation A = Consistent, good-quality patient-oriented evidence B = Inconsistent or limited-quality patient-oriented evidence C = Consensus, disease-oriented evidence, usual practice, expert opinion, or case series for studies of diagnosis, treatment, prevention, or screening (Ebell, et al., 2003) Outcome Measures WHO International Classification of Functioning, Disability and Health http://www.who.int/classifications/icf/training/icfbeginnersguide.pdf Impairment Activity/Participation Contextual factors Pre- and Post-treatment Measures Daily Probes • Impairment-based outcome measures – Standardized tests (i.e. WAB, BDAE, BNT) – Lexical retrieval measures (i.e. # items named) – Sentence production (i.e. sentence form SVO) • Activity/Participation-based outcomes – Communication skills (i.e. CETI Lomas et al. 1989 ) – Correct Information Units (i.e. CIUs Brookshire & Nicholas, 1993) – Content (i.e. Content Units Yorkston & Beukelman, 1980) – Communication partner rating Effect size • Many methods of calculation • Most common method references means and variability – d = (M post-treatment – M pre-treatment) SD Pre-treatment – Between or within subjects – .2 = small .5 = medium .8 = large (Cohen, 1962) • Single subject designs (Beeson & Robey, 2008) ASHA & Evidence • National Center for Evidence-based Practice – Compendium of evidence – Systematic Reviews – Evidence Maps • Advisory Committee on Evidence-based Practice – Guides the work of N-CEP – Identify clinical questions ASHA Homepage > Research Tab > Evidence-based Practice KSHA 2010 Aphasia Treatment KSHA 2010 Aphasia Treatment KSHA 2010 Aphasia Treatment KSHA 2010 Aphasia Treatment KSHA 2010 Aphasia Treatment KSHA 2010 Aphasia Treatment KSHA 2010 Aphasia Treatment ANCDS & Evidence • Writing Groups • Practice Guidelines KSHA 2010 Aphasia Treatment KSHA 2010 Aphasia Treatment Cautions • Study quality Strength of evidence Practice Guidelines • Methodology is often inconsistent • Seeking the best evidence may result in lack of support for a treatment without evidence • Consider all EBP components in treatment decisions APHASIA TREATMENT Aphasia language treatment • Treatment is beneficial – Kelly, Brady & Enderby (2009) • http://web.ebscohost.com/ehost/pdfviewer/pdfviewer ?vid=8&hid=10&sid=c62a94a6-f882-4088-973a0099791a0b6b%40sessionmgr112 – Robey (1998, 1994) – Salter, Teasell, Bhogal, Zettler, Foley (2009) • http://www.ebrsr.com/reviews_list.php • Insufficient evidence to state which treatment for which patient in which dosage IMPAIRMENT-BASED TREATMENT TECHNIQUES Impairment-based treatment techniques • • • • • • • Lexical retrieval Constraint-Induced Language Treatment Cueing Hierarchy Semantic Feature Therapy Reading Writing Complexity Account of Treatment Effectiveness LEXICAL RETRIEVAL Theoretical Foundation • Semantic network or feature network – A way of thinking about knowledge in which there are concepts and relationships among them. – A diagrammatic representation comprising some combination of boxes, arrows and labels. • Storage, central processing or retrieval deficit Example of a semantic network • A concept (bird) defined as set of features – defining features - necessary to the meaning of the item (robin has a red breast) – characteristic features - descriptive but not essential • How close is target to exemplar – Target = chicken, sparrow, robin, penguin – Exemplar = robin Example of semantic feature set Cognitive neuropsychological processing model of word retrieval Kay, Lesser & Coltheart, 1992 Treatment examples • Stimulation-facilitation (Schuell, 1965) • Cues – Cueing hierarchy (Linebaugh & Lehner; Patterson, 2001) – Semantic or Phonologic (Raymer et al., 1993; Wambaugh et al., 2002) – Personal cues (Marshall, Karow, Freed & Babcock, 2002) – Semantic Features (Boyle & Coelho, 1995) • Gesture (Raymer, Singletary, Rodriguez , Ciampitti, Heilman & Rothi , 2006; Rose, Douglas & Matyas, 2002) Evidence, ES & Conclusions • Evidence – – – – Some RCTs but not large scale clinical trials No Systematic Reviews One meta analyses (Wisenburn & Mahoney, 2009) Many single subject designs or case studies • Effect Sizes – Robey & Beeson (2005) reported tentative ES of 4.0, 7.0 and 10.1 calculated from 12 studies • Point is that Cohen’s d is meant for group studies and much of our work is single subject studies, requiring a different comparison – Compare an individual study to these benchmarks RCT Effect Size favoring treatment for naming outcome measure Treated items Naming Naming Task Specific v General Individual v Group PICA AAT SLP v Volunteer PICA AAT Effect Size Conventional v Functional AAT PALPA Treatment v Social Support Word Fluency Object Naming Test Treatment v No Treatment WAB Naming BNT 0 2 4 6 8 10 12 14 Kelly, Brady & Enderby, 2010 • Consistent results across sources of evidence – RCT, EBSR, individual review • Moderate to strong evidence in favor of treatment – Task specific and item specific effects • Phonological v semantic cueing • Noun v verb training • Weak evidence in favor of generalization to untreated items and maintenance • Insufficient evidence to state which treatment for which patient in which dosage CONSTRAINT INDUCED LANGUAGE THERAPY Theoretical Foundation • Pulvermller et al. (2001) reasoned that principles of CIMT could be applied to aphasia treatment • Learned non use observed in persons with aphasia – Failed communicative attempts “punished” (i.e. frustration or embarrassment) leading to even fewer attempts – Compensatory communication attempts rewarded and thus prevail – Fewer and more difficult communicative attempts occurred • Does “use it to improve it” apply to language change in persons with aphasia? Principles of CILT • Forced verbal language use and application of constraint – Verbalization required – Compensatory strategies prohibited (constrained) • Intensive treatment schedule – Massed practice – 3 hrs/day 5 days/week 2 weeks • Shaping verbal responses – Begin with words or short phrases – Move to longer and more complex utterances Model Use dependent Cortical Reorganization Neuronal plasticity – Events that regulate the capacity of the CNS to change in response to injury or physiological demands – Potential for change – Several mechanisms of change (i.e. synaptogenesis, dendritic arborization) CILT questions For stroke-induced chronic aphasia, what is the influence of constraintinduced language therapy on measures of language impairment? For stroke-induced chronic aphasia, what is the influence of constraintinduced language therapy on measures of communication activity/participation? For stroke-induced acute aphasia, what is the influence of constraint-induced language therapy on measures of language impairment? For stroke-induced acute aphasia, what is the influence of constraint-induced language therapy on measures of communication activity/participation? For stroke-induced chronic aphasia, what treatment outcomes are maintained following constraint-induced language therapy? Cherney, Patterson, Raymer, Frymark, Schooling (2008) Evidence, ES & Conclusions • Systematic Review 2008 • 5 studies with 90 participants - Language impairment measures: CILT resulted in positive changes; primarily nonfluent patients - Communication activity/participation measures: CILT reported to lead to positive changes, though no effect sizes calculable - Data available only for chronic aphasia. No data speak to the effects of CILT in acute aphasia. - Maintenance of CILT effects: reported to lead to positive changes; no effect sizes calculable Cherney, Patterson, Raymer, Frymark, Schooling (2008) • CILT Update 2010 • 14 studies with 230 participants - Language impairment measures: CILT resulted in positive changes - Communication activity/participation measures: CILT resulted in positive changes - Data available for acute and chronic aphasia. CILT resulted in positive changes - Maintenance of CILT effects: CILT resulted in positive changes • However … – Preliminary evidence; exploratory in nature – Varying protocols and tasks Frymark, Cherney, Patterson & Raymer (2010) Activity Participation Impairment Effect Sizes favoring Constraint Induced Language Treatment for Impairment and Activity/Participation outcome measures Total # words Tense diversity Tense accuracy Proportion of well-formed sentences Proportion of sentences Memantine+CIAT prepost (CAL) Different root words # Utterances AATSpontaneous Speech Severity Repetition Naming Memantine+CIAT v Placebo+CIAT Memantine+CIAT prepost (Naming) LCI Comprehension BNT BDAE-3 VE BDAE-3 AC ANT ANELT SC ANELT AC AAT TT AAT TT AAT TT AAT Profile Therapist trained AAT Profile Relative trained AAT Profile AAT Profile WAB AQ -0.2 0.8 1.8 2.8 3.8 4.8 5.8 6.8 Summary Evidence-based medicine is the integration of best research evidence with clinical expertise and patient values. N-CEP, PsychBITE, ANCDS, Division 2 are sources of evidence. Aphasia therapy is effective; dosage is unclear. Moderate evidence for effectiveness of lexical retrieval treatment. Weak evidence for generalization of treatment gains. Moderate evidence for effectiveness of CILT.