Nutrition in the Hospitalized Patient
advertisement

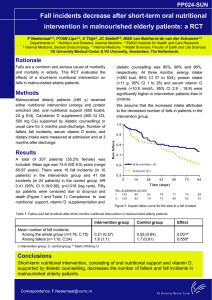
Nutrition For the Hospitalized Patient What is Important? • Making Sure that the patient eats • Making Sure that the patient eats the Right Foods Objectives of this Talk • What is Malnutrition? • Why is this Important in the hospitalized patient? • Specific Diets • Other added information Malnutrition WHO (World Health Organization) definition: Cellular imbalance between the supply of nutrients and energy AND the body’s demand for them to ensure growth, maintenance and specific functions Why Is This Important in the Hospitalized Patient? • Disease-related malnutrition is a major health care problem and results in a reduced ability to prevent, fight, and recover from disease. • Malnutrition is associated with postoperative complications, increased length of hospital stay, and even death. To Whom Should We Pay Attention? • 40 percent of older people are malnourished when they are admitted to hospital • Nutritional status of 60 percent of all older patients will deteriorate further while they are in hospital • Decreased Food Intake Represents an Independent Risk Factor for Hospital Mortality One Study in Australia • 58 percent of the patients, who were aged 65 or over, had problems eating. • Just under a third (31 percent) left more than two-thirds of their meal • Only 15 percent had eaten their whole meal. • More than half of the patients they studied (55 percent) had problems opening food. • About a third found it difficult to use cutlery (36 percent). More Results • More than a fifth (23 percent) were too far away from their food. • Interruptions were also frequent. – One in five patients (19 percent) had a doctor's visit during mealtimes – more than half (51 percent) had mealtimes interrupted by other staff, mostly nurses (92 percent). What Happens in the Starving, Stressed Patient? • Stress/Trauma activates the sympathetic nervous system (flight or flight) • Utilization of carbohydrates are inhibited and hyperglycemia often occurs – Insulin secretion declines – Blood levels of glycogen, growth factor, catecholamines, thyroid hormones, ACTH, ADH all increase • Lipolysis is activated, gluconeogenesis and proteolysis is acclerated, large amounts of protein are consumed to provide the energy needed How To Evaluate This Nutritional Assessment • • • • • • Clinical History Exam and Body Composition Analysis Indirect Calorimetry Anthropomorphic Measurements Functional Studies of Muscle Function Biochemical Measurements What is Easy and Effective? • History – At admission or during stay: 10% weight loss or more suggests protein malnutrition – NPO or Clears > 5-7 days – Use one of the simple questionnaires: • The Short Nutritional Assessment Questionnaire (SNAQ) • The Subjective Global Assessment • DETERMINE The Short Nutritional Assessment Questionnaire (SNAQ) Question Did you lose weight unintentionally? >6 kg in the past 6 mo >3 kg in the past month Did you experience a decreased appetite over the past month? Did you use supplemental drinks or tube feeding over the past month? Scoring: Well nourished: 0 or 1 points Moderately Malnourished: 2 points Severely Malnourished ≥3 points Score 3 2 1 1 Results of One Study for SNAQ • Recognition of malnutrition improved from 50% to 80% with the use of the SNAQ malnutrition screening tool during admission to the hospital. • The standardized nutritional care protocol added ≈600 kcal and 12 g protein to the daily intake of malnourished patients. • Early screening and treatment of malnourished patients reduced the length of hospital stay in malnourished patients with low handgrip strength (ie, frail patients). • To shorten the mean length of hospital stay by 1 d for all malnourished patients, a mean investment of €76 (US$91) in nutritional screening and treatment was needed. Subjective Global Assessment • Strengths: – Combines self report, clinical assessment and simple bedside evaluation for dysphagia. – Identifies patients who may benefit from nutritional counseling or home delivered meals – Includes evaluation of activities of daily living, depression, poor oral health, polypharmacy or status of underlying chronic conditions. • Limitations: – A significant proportion of the instrument requires patient or proxy report and depends on the history being available and correct. DETERMINE • Strengths: – Quick and easy to administer 10 item questionnaire to patient or proxy. – The checklist identifies patients who may benefit from nutritional counseling or home delivered meals – Evaluates activities of daily living, depression, poor oral health, polypharmacy or status of underlying chronic conditions • Limitations: – The instrument is dependent on the patient or proxy having the information and being forthright. What to Look For? Objective Findings/Exam • Weight/Ideal body weight (<85% predicted) – (IBW See Metropolitan Life Insurance Company Charts) – BMI <18 kg/m2 • Anthropometrics = weight to height assessment – difficult since there are fluid shifts or accumulations and inaccurate wts • Physical Exam – temporal wasting, thenar atrophy, … • GI tract functioning – i.e. previous surgery What to Test? • Immune Function – lymphocyte <1800, skin testing, anergy • Prealbumin – T1/2 = 2 days – Falsely elevated with RF, Hodgkin’s Disease, Steroids – Falsely low with acute catabolic stress, hepatic disease, stress, infection, surgery • Albumin – T1/2 = 21 days so does not reflect acute changes – Falsely elevated with dehydration – Falsely low with edema, hepatic disease, anemia, malabsorption, diarrhea, burns, volume overload, ESRD • Transferrin – T1/2 = 7 days • Fat Soluble Vitamins: – A, E, and 25-hydroxyvitamin D can be measured directly. – Prothrombin time is used as a proxy to measure vitamin K. More Tests • U24 hr for Urea nitrogen (cannot be used with RF) – Nitrogen balance used to measure degree of catabolism – Nitrogen Balance= Intake – Output » = Protein Intake/6.25 – (Urine urea nitrogen +4) [the 4 is to account for the skin+stool loses] » Goal is to have at least 3 to 4 grams positive for growth and repair • Serum carotene – correlated with vitamin A status – can be used as a surrogate marker of malabsorption and nutritional status • Retinol Binding Protein (RBP) - used to determine visceral protein mass in nutritional studies related to health. – measurement of serum retinol levels (levels less than 20 micrograms/dL suggest deficiency) or – the ratio of retinol:RBP (a molar ratio <0.8 suggests deficiency) Requirements in General • Figure out Calories needed then what percentages based on nutrients • Nutrients – 3 major sources for the Fuel/Calories • Amino Acids/Protein = 15% – Non Stressed Protein = 0.8 to 1 gm/kg/day or 150 mg of nitrogen/kg/day – Stressed = 1.7g/kg/day or 200 -250 mg N/kg/day • Fat = 25-50% • CHO = 35-65% – Plasma Electrolytes – Vitamins and Micronutrients • Fat Soluble Vitamins are more likely than Water Soluble to be low if malnourished What Does a Hospitalized Patient Need? BMR x Activity Factor x Stress Factor Basic Metabolic Rate (BMR) The Minimum • Women: – BMR = 655 + ( 4.35 x weight in pounds ) + ( 4.7 x height in inches ) - ( 4.7 x age in years ) • Men: – BMR = 66 + ( 6.23 x weight in pounds ) + ( 12.7 x height in inches ) - ( 6.8 x age in year ) • Women: – BMR = 655 + ( 9.6 x weight in kilos ) + ( 1.8 x height in cm ) - ( 4.7 x age in years ) • Men: – BMR = 66 + ( 13.7 x weight in kilos ) + ( 5 x height in cm ) - ( 6.8 x age in years ) Quick Reference for Requirements Without Stress or Activity • Calories 1600 • Total Fat (g) 53 • Saturated Fat (g) 18 • Total • Carbohydrate (g) 240 • Dietary Fiber (g) 20 • Protein (g) 46 1800 2000 2500 2800 59 65 73 80 19 20 24 25 270 300 330 375 23 48 25 50 25 55 30 65 Harris Benedict Formula To Determine Total Daily Calorie Needs = BMR x Activity • If you are sedentary (little or no exercise) : CalorieCalculation = BMR x 1.2 • If you are lightly active (light exercise/sports 1-3 days/week) : Calorie-Calculation = BMR x 1.375 • If you are moderatetely active (moderate exercise/sports 3-5 days/week) : Calorie-Calculation = BMR x 1.55 • If you are very active (hard exercise/sports 6-7 days a week) : Calorie-Calculation = BMR x 1.725 • If you are extra active (very hard exercise/sports & physical job or 2x training) : Calorie-Calculation = BMR x 1.9 What is Activity in the Hospitalized Patient? Patient Activity Ambulatory Activity Factor 1.25 Bedridden 1.15 Ventilator Support 1.10 Stresses of The ILL Patient Patient Status Stress Factor Elective Operation/Minor Surgery Non-Stressed, On Vent CHF Fever Peritonitis Long Bone Fracture Mild to Moderate Infection Multiple Trauma/Major Surgery Stressed/Vent Dependent Sepsis Liver Failure/Cancer Burns 1-1.2 1-1.2 1-1.2 1.1-1.2 1.13 1.05-1.25 1.2-1.4 1.3-1.55 1.4-1.6 1.5-1.75 1.5 1.25-2 Quick and Dirty Energy Requirements kcal/kg/day • Unstressed = 25 • Stressed = 35 Protein Requirements g/kg/day • • • • • • • Mild stress = 0.8-1 Moderate stress = 1-1.2 Severe stress = 1.2-2 ARF = 1-1.5 ESRD = 0.5-0.6 (if not on Hemodialysis) Hemodialysis = 1.1-1.5 Liver Failure = 0.5 (with encephalopathy) Don’t Forget Hydration • Baseline: 30-35 ml/kg/24 hr • Add: 2-2.5 ml/kg/day of fluid for each degree of temperature • Account for excess fluid losses When to Ask For Help • Apon Admission if: Enteral Dependent, Parenteral Dependent, Documented Malnutrition, Failure to Thrive, New Diagnosis of Diabetes/Renal Failure, Severe/Complicated Wounds • BMI<19 • Poor nutritional status (the current oral intake meets <50% of energy needs) • >7 days NPO • Albumin <3 measured in the absence of an inflammatory state • Severe Weight Changes = Usual BW-Current BW x 100/ Usual BW = % Weight Change – 1 week 1-2%, 1 mo 5% or greater, 3 mo 7.5% or greater, 6 mo 10% or greater Diets: • Diabetic: 1500-1800 or 1900-2500 cal – Controls CHO, Limits Na, Fat, Chol • Renal – Controls K, Protein, Phosphorous (HD 800 mg/d, Peritoneal Dialysis 1200mg/d) – Common Modifier – fluid restriction • Sodium – – – – – Cardiac 4g Na – HTN and CVD Caridac 2g Na – CHF, Fluid restrict? Regular Diet with 4g Na – HD patients with good K, Phos Liver 2 g Na – Cirrhotic with Ascites Differences: Cardiac restricts Fat, Chol, Caffeine; Liver does not restrict Fat, Protein • Dysphagia – Two Part Order – Texture = Pureed (1), 2, Mechanical Soft or Regular – Liquid Level = Thin, Nectar-thick, Honey-thick, Spoon-thick • Enteral Feeding – whole different lecture for indications, how, types, costs Sodium Amount of Sodium in Salt • ¼ teaspoon salt 600 milligrams of sodium • ½ teaspoon salt 1,200 milligrams of sodium • ¾ teaspoon salt 1,800 milligrams of sodium • 1 teaspoon salt 2,300 milligrams of sodium • 1 teaspoon baking soda 1,000 milligrams of sodium • Many non-prescription drugs such as antacids, laxatives, aspirin, • cough medicines and mouthwash have sodium. Ask your doctor or • pharmacist for more information. • Water softening equipment can add large amounts of sodium to water. Foods High in Vitamin K • • • • • • • • • Asparagus Broccoli Brussels Sprouts Dandelion greens Endive Lettuce (iceberg, bibb, Boston and green leaf) Parsley Sauerkraut Scallions Calcium • Calcium Citrate – recommended form of calcium supplements because it is best absorbed by the body. – Calcium Citrate does not require the presence of stomach acid to dissolve. – Limit your supplement to no more than 500 mg at one time to increase absorption. – All calcium supplements should include Vitamin D, – Goal is 1500 mg of calcium from food and supplements. – Do not take calcium supplements around the same time as prenatal or iron supplements. • The % daily value of Calcium on food labels – There is an easy way to figure out how many milligrams (mg) of calcium is in food items. All you have to do is remove the % from the Daily Value for calcium and add a "0"! Vitamin D • • • • 1- 70 years old = 600 IU/day > 70 years old = 800 IU/day Upper safe limit is 4000 IU/day Sources – Sunlight – 15-30 minutes/day – Foods: codliver oil, salmon canned, tuna fish canned, shrimp cooked, fortified milk/yogurt/orange juice • Medicines that interfere with Vit D – Antacids with magnesium, corticosteroids, weight loss drugs (xenical, orlistat, alli), cholesterol reducing drugs (chlosteramine, questran, locholest), seizure medications (phenytoin/dilantin, phenobarbitol), thiazide diuretics (HCTZ) Potassium • Foods Very High in Potassium (more than 400 mg per serving) – Fruits: Dried prunes (¼ cup), dried apricots (¼ cup), prune juice, orange juice, grapefruit juice, papaya, banana, honeydew melon, cantaloupe – Vegetables: Tomato paste, tomato puree, beet greens, lima beans, squash, iceberg lettuce, sweet potato, kidney beans, Chinese cabbage, tomatoes, French fries (1 small order), parsnips, frozen spinach, pumpkin, mushrooms, white potatoes (1 potato), Brussels sprouts, broccoli, cucumber – Other: Yogurt, salmon (½ fillet), barley, molasses (1 Tablespoon), cream of tartar (1 teaspoon), tuna (3 ounces), eggnog, skim milk, trail mix with chocolate chips, low sodium baking powder (1 teaspoon) Potassium • Foods High in Potassium (more than 200 mg per serving) – Fruits: Peaches, pears, watermelon, mandarin oranges, mango (1 medium mango), apple juice, blackberries, nectarine (1 nectarine), red or green grapes, strawberries, dried figs (2 figs), raisins (¼ cup), kiwi (1 medium), raspberries, boysenberries – Vegetables: Asparagus, sweet corn, carrots, summer squash, celery, cauliflower, turnip greens, red/green peppers, beets, onions, black eyed peas, spinach, zucchini – Other: Peanut butter (2 Tablespoons), 1% milk, raisin bran cereal, low-fat buttermilk, plain potato chips, soy milk, part skim ricotta cheese, seasoned dried bread crumbs, vanilla ice cream (½ cup), sunflower seeds (¼ cup), ground beef 85/15 (3 ounces), pumpkin seeds (1½ cups), roasted turkey (3 ounces), white rice, egg substitute (¼ cup), almonds (24 nuts) Iron • Iron tablets may be taken 3 times a day, in between meals. – Avoid taking iron with a phosphate binder (Calcium carbonate, Tums, Phos- Ex, Phos-Lo, Cal-Carb, Calcium acetate) – Large amounts of Calcium bind with iron and make iron less available for absorption by the body. – If a calcium binder is taken with meals, wait at least one hour after a meal before taking iron. – Avoid taking iron with coffee or tea (wait at least one hour), as well as with – Foods high in vitamin C will increase absorption of iron in your body. Phosphorous • High in Phosphorous – – – – Liver Sunflower seeds Wheat germ Pumpkin seeds • Moderate Phosphorous – – – – – – – – Milk, Dairy Products Chocolate Legumes Nuts and Seeds Meats Whole grains Bran Cereals Muffins Magnesium • Adults need between 320mg-420 mg/day • Good Sources – Nuts – almonds, cashews, peanut butter – Legumes and Seeds – blk eyed peas, garbanzo beans, kidney beans, lima beans, navy beans, sesame seeds ground as tahini, soybeans, sunflower seeds – Whole Grains – Dark Green Vegetables – beet greens, broccoli, spinach – Other vegetables – artichokes, avocados – Dried fruit - figs – Soy Products - tofu – Chocolate – Meats – Seafood – crabs, lobster, shrimp – Dairy Products – Other – oatmeal, potato baked with skin on, wheat bran, wheat germ Guideline for Nutritional Interventions • See Handout