§
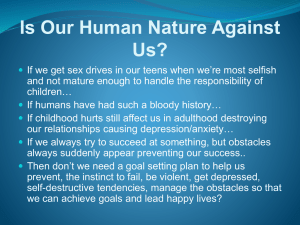
Food Allergens
Atypical IgE-Mediated Conditions
§
Non-IgE-Mediated Conditions
Characteristics and
Reaction Mechanisms
Types of Allergenic Proteins
• Storage proteins, especially in nuts, seeds
and cereal grains
• Inhibitors of enzymes that may be
destructive to storage factors, for example:
– Inhibitors of alpha amylases that might break
down starches
– Anti-trypsin protects against trypsin breakdown
of proteins in cereal grains
• Structural proteins
2
Types of Allergenic Proteins
• Regulatory proteins, such as profilins, that are
important in plant fertilization (for example in
pollens)
• Pathogenesis-related proteins: proteins involved in
the defense-related activities of the plant, for
example:
– Hevamines that are lysozyme-like enzymes that break
down fungal cell walls and defend the plant against
fungal attack
• Lipid transfer proteins (LTP) that are essential in
the functioning of a cell
3
Allergenic Proteins in Specific
Foods
• Each food contains many proteins, some of which
are potential allergens, and have different
characteristics and degree of allergenicity: for
example:
• MILK
– Contains about 30 potential allergens, some of which
are heat stable; some are heat labile:
• Caseins (α; β; κ) tend to be heat stable
• Whey proteins including alpha-lactalbumin and betalactoglobulin tend to be heat labile
– Individuals allergic to only heat labile proteins usually
can drink heated milk with impunity
4
Allergenic Proteins in Specific Foods:
Wheat
• Protein makes up ~12% of the dry wheat kernel
• Many of the proteins in wheat are allergenic
• Wheat proteins are roughly divided into the
following four classes
•
Gliadins
•
Glutenins
•
Albumins
•
Globulins
• Gliadins contain as many as 40 to 60 distinct components
• Glutenins contain at least 15
• Albumins and Globulins also may be allergenic
• Allergy to specific proteins tends to be populationrelated
5
Egg Allergens
• Eggs contain many different proteins that can lead to
allergy
• An egg-allergic individual is likely to be sensitized to more
than one protein
• Although egg yolk contains several proteins, egg white
(ovalbumin) contains the greatest number of allergens
• Up to 24 different antigenic protein fractions have been
isolated, although the allergenicity of most of them is
unknown
• The main allergens are:
–
–
–
–
Ovalbumin
Ovomucoid
Ovotransferrin
Lysozyme
6
Peanut Allergens
The major allergenic peanut proteins have been
characterized and named.
The “Ara h” in the name of each protein is derived
from the Latin name for peanut, Arachis hypogaea:
•
•
•
•
•
•
Ara h 1
Ara h 2 (5 subtypes)
Ara h 3
Ara h 4
Ara h 5
Ara h 6
•
•
•
•
•
•
Ara h 7
Ara h 8
Ara h agglutinin
Ara h LTP
Ara h oleosin
Ara h TI
7
Relative importance of individual peanut
allergens in allergy
• Ara h 2 recognized most frequently as the
causative allergen in all tests for symptomtriggering allergens and induced a reaction at
relatively low concentrations
• Ara h 1 and Ara h 3 were recognized less
frequently and reacted only at 100-fold higher
concentrations than Ara h 2
• Presence of Ara h 2 suggested as marker for
peanut allergy
Koppelman et al 2004
8
Prevalence of sensitization to all peanut
allergens
•
•
•
•
•
•
•
•
Population of 40 patients sensitized to peanut:
Ara h 1 (65%)
Ara h 2 (85%)
Ara h 4 (53%)
Ara h 5 (13%)
Ara h 6 (38%)
Ara h 7 (43%)
Although Ara h 6 was considered a minor allergen, the
authors found that sensitization to Ara h 6 was associated
with more severe clinical symptoms than most of the other
allergens
9Becker et al 2001
Chemical Structure of Food Allergens
• Allergenic proteins from an increasing
number of foods have been characterised
• The Food Allergy Research Resource
Program (Farrp) database
(http://www.allergenonline.com) contains
details of unique proteins of known
sequence that are classified as food
allergens
10
Classification of Food Allergens
[Sampson 1999]:
Class 1 food allergens:
• Encounter the immune system through the
digestive tract
• Induce allergic sensitization directly via the
intestine
• Are resistant to digestive enzymes
• Are stable in response to gastric acid
• Are heat-stable and are not deactivated by
cooking
11
Class 2 food allergens
• Do not induce allergic sensitization in the
digestive tract
• Rapidly dissolve in the oral cavity
• Are readily broken down by digestive
enzymes
• Are susceptible to acid in gastric secretions
• Are heat-labile and are generally
deactivated by cooking.
12
Class 1 Food Allergens
Characteristics
• Physicochemical properties that confer
allergenicity are relatively unknown
• Usual characteristics of allergenic fraction of food:
– Protein or glycoprotein
– Molecular size 10 to 70 kDa
– Heat stable
– Water soluble
– Relatively resistant to acid hydrolysis
– Relatively resistant to proteases (especially
digestive enzymes)
13
Incidence of Allergy to Specific Foods
• In young children: 90% of reactions caused by:
– Milk
– Egg
– Peanut
- Soy
- Wheat
• In adults: 85% of reactions caused by:
– Peanut
– Fish
– Shellfish
- Tree nuts
14
Incidence of Allergy to Specific Foods
• Increasing incidence of allergy to “exotic
foods” such as:
– Kiwi
– Papaya
– Seeds: Sesame; Rape; Poppy
– Grains: Psyllium
15
Major Allergenic Foods:
Annex IIIa EU Directive on Labeling of Foods
Which Must be Declared
• Cereals containing gluten, (i.e. wheat, rye,
barley, oats, spelt, kamut or their hybridized
strains) and products thereof
• Crustaceans and products thereof
• Eggs and products thereof
• Fish and products thereof
• Peanuts and products thereof
• Soybeans and products thereof
• Milk and products thereof (including
16
lactose)
Major Allergenic Foods:
Annex IIIa EU Directive on Labeling of Foods
Which Must be Declared Continued
• Nuts i.e. almonds, hazelnuts, walnuts, cashews,
pecan nuts, Brazil nuts, pistachio nuts, macadamia
nuts and Queensland nuts and products thereof
• Celery and products thereof
• Mustard and products thereof
• Sesame seeds and products thereof
• Sulphur dioxide and sulphites at concentrations of
more than 10 mg/kg or 10 mg/litre expressed as
SO2.
• Lupin and products thereof
• Molluscs and products thereof
17
Panallergens
• Most allergenic foods contain species-specific
proteins
• This means that individual sensitisation to a food
is specific to that food and none other, even if the
foods are zoologically or botanically related
• However, recent research is indicating that some
proteins with the same function in different food
plants or animals may be allergenic
• May be:
– Lipid transfer proteins
– Pathogenesis-related proteins
– Profilins
18
Panallergens continued
• A person sensitised to such a protein may
then be sensitive to the same protein where
it occurs in different species
• The proteins tend to be weakly allergenic
• Such allergens have been designated
“Panallergens”
• Examples include:
– Parvalbumins in fish
– Proteins responsible for oral allergy syndrome
and latex allergy
19
Oral Allergy Syndrome
(OAS)
OAS refers to clinical symptoms in the
mucosa of the mouth and throat that:
• Result from direct contact with a food allergen
• In an individual who also exhibits allergy to
inhaled allergens
• Usually pollens (pollinosis) are the primary
allergens
• Pollens usually trigger rhinitis or asthma in these
subjects
20
Oral Allergy Syndrome
Characteristics
• Inhaled pollen allergens sensitise tissues of the
upper respiratory tract
• Tissues of the respiratory tract are adjacent to oral
tissues, and the mucosa is continuous
• Sensitisation of one leads to sensitisation of the
other
• First described in 1942 in patients allergic to birch
pollens who experience oral symptoms when
eating apple and hazelnut
• OAS symptoms are mild in contrast to primary
food allergens and occur only in oral tissues
21
Oral Allergy Syndrome
Allergens
• Pollens and foods that cause OAS are
usually botanically unrelated
• Several types of plant proteins with specific
functions have been identified as being
responsible for OAS:
– Profilins
– Pathogenesis-related proteins
22
Oral Allergy Syndrome
Allergens
• Profilins are associated with reproductive
functions
• Pathogenesis-related proteins tend to be
expressed when the tree is under stress (e.g.
growing in a polluted area; exposed to
potential pathogens)
– May be hevamines
23
Oral Allergy Syndrome
Cross-Reactivity
• Occurs most frequently in persons allergic
to birch and alder pollens
• Also occurs with allergy to:
– Ragweed pollen
– Mugwort pollen
– Grass pollens
24
Oral Allergy Syndrome
Associated foods
• Foods most frequently associated with OAS are
mainly fruits, a few vegetables, and nuts
• The foods cause symptoms in the oral cavity and
local tissues immediately on contact:
–
–
–
–
–
Swelling
Throat tightening
Tingling
Itching
“Blistering”
25
Oral Allergy Syndrome
Characteristics of Associated foods
• The associated foods usually cause a reaction
when they are eaten raw
• Foods tend to lose their reactivity when cooked
• This suggests that the allergens responsible are
heat labile
• Allergic persons can usually eat cooked fruits,
vegetables, nuts, but must avoid them in the raw
state
26
Oral Allergy Syndrome (OAS):
Cross-reacting Foods and Pollens
Pollen Allergen
Birch
Mugwort
Grass
Timothy Grass
Fruit
Apple
Apricot
Cherry
Kiwi fruit
Melon
Nectarine
Orange
Peach
Pear
Plum
Prune
Watermelon
Vegetables Herbs
and Spices
Anise
Asparagus
Cabbage
Carrot
Celery
Coriander
Cumin
Dill
Fennel
Green peppers
Parsley
Parsnip
Potato
Tomato
Legumes and
Grains
Beans
Lentils
Peanuts
Peas
Soy
Rye
Nuts and
Seeds
Almond
Chestnut
Hazelnut
Walnut
Caraway seed
Poppy seed
Sesame seed
Sunflower seed
27
Oral Allergy Syndrome
Cross-reacting allergens
• Ragweed pollen with:
–
–
–
–
–
–
–
Banana
Cantaloupe
Honeydew
Watermelon
Other Melons
Courgette
Cucumber
28
Oral Allergy Syndrome Diagnosis
• Syndrome seen most often in persons with birch pollen
allergy compared to those with allergy to other pollens
• Seen in adults much more frequently than children
• Reactions to raw fruits and vegetables are the most
frequent food allergies with onset in persons over the
age of 10 years
• Has also been described in persons with IgE-mediated
allergy to shrimp and egg
This may not be true OAS; allergy may be
expressed as symptoms in the mouth in conditions
distinct from OAS
29
Expression of OAS Symptoms
• Oral reactivity to the food significantly decreases when
food is cooked
• Reactivity of the antigen depends on ripeness
– Antigen becomes more potent as the plant material ages
• People differ in the foods which trigger OAS, even when
they are allergic to the cross-reacting pollens
– Foods express the same antigen as the allergenic pollen, but
not all people will develop OAS to all foods expressing that
antigen
30
Identification of Foods Responsible
for OAS Symptoms
• Skin tests will identify the allergenic plant pollen
• Skin testing has not been successful in identifying
persons who react to cross-reacting food antigens
– Plant antigens are unstable and do not survive the
process of antigen preparation
– Crushing plant material leads to release of phenols and
degradative enzymes
• Prick + prick technique are more reliable than
standard skin tests
– Lancet is inserted in raw fruit or vegetable, withdrawn
and then used to prick the person’s skin
31
Latex Allergy
• Allergy to latex frequently starts as a Type
IV (contact) hypersensitivity reaction
• Contact is with an allergenic protein usually
through:
– Abraded (non-intact) skin
– Mucous membrane by inhalation
– Exposed tissue (e.g. during surgery)
32
Latex Allergy
Cross-reacting allergens
• As antigen comes into contact with immune
cells, repeated exposure seems to lead to
IgE mediated allergy
• Reaction becomes systemic
• Similar proteins in foods tend to trigger the
same IgE response
• In extreme cases can cause anaphylactic
reaction
33
Foods with Allergens Similar to Latex
Category
Food
Type III
Clinical findings
Identification of cross-reactive allergens
Avocado
Banana
Bell pepper
Cassava
Celery
Cherimoya
Chestnut
Custard apple
Kiwi fruit
Mango
Papaya
Passion fruit
Potato
Tomato
Chestnut
Pistachio
Walnut
Type II
Clinical findings
Characterization of cross-reactive components by extract
inhibition assays
Fig
Melon
Peach
Pineapple
Turnip
Zucchini
Type I
Clinical findings only
Apple
Apricot
Aubergine (eggplant)
Carrot
Cherry
Coconut
Loquat
Spinach
Strawberry
Watermelon
34
Common allergens in unrelated plant
materials: Summary
• OAS and latex allergy are examples of conditions
in which common antigens, expressed in
botanically unrelated plants, are capable of
eliciting a hypersensitivity reaction
• Previous assumptions that plant foods in the same
botanic family are likely to elicit the production of
the same antigen- specific IgE are thus
questionable
35
Common allergens in unrelated plant
materials: Summary
• In practice, when a specific plant food elicits an
allergic response, foods in the same botanic family
rarely elicit allergy
• It is important to recognize the allergenic potential
of antigens common to certain botanically
unrelated plant species, and take appropriate
measures to avoid exposure of the allergic
individual to them
36
Non-IgE-Mediated Allergies
Eosinophilic Gastrointestinal Diseases
Food Protein Induced Enteropathies
Eosinophilic Gastrointestinal
Diseases (EGID)
• Expanded definition of food allergy now
encompasses any immunological response to food
components that results in symptoms when the
food is consumed
• Example is group of conditions in the digestive
tract in which infiltration of eosinophils is
diagnostic
• Collectively these diseases are becoming known
as eosinophilic gastrointestinal diseases (EGID).
38
Characteristics of EGID
• Inflammatory mediators are released from
the eosinophils, and act on local tissues in
the oesophagus and gastrointestinal tract,
causing inflammation
• In eosinophilic digestive diseases there is no
evidence of IgE, therefore tests for IgEmediated allergy are usually negative
• Unless there is a concomitant IgE-mediated
reaction to food
39
Characteristics of EGID
• Eosinophils are also found in abundance
in the intestinal canal in diseases such
as:
– inflammatory bowel disease
– infections caused by parasites such as
helminths and nematode worms
• These need to be ruled out before EGID
is diagnosed
40
Eosinophilic Oesophagitis
• Symptoms most frequently associated with EO
and considered to be typical of the disease include:
– Vomiting
– Regurgitation of food
– Difficulty in swallowing: foods are said to be sticking
on the way down
– Choking on food
– Heartburn and chest pain
– Water brash (regurgitation of a watery fluid not
containing food material)
– Poor eating
– Failure to thrive (poor or no weight gain, or weight
loss)
41
Eosinophilic Oesophagitis
• Although the symptoms resemble gastrooesophageal reflux disease (GORD), the
reflux of EO dose not respond to the
medications used to suppress the gastric
acid and control regurgitation (antireflux
therapy) in GORD
• There is emerging data to suggest that use
of acid-suppressing medications may
predispose patients to the development of
EO
42
Diagnosis of EO
Three criteria must be met:
• Clinical symptoms of oesophageal
dysfunction
• Oesophageal biopsy with an eosinophil
count of at least 15 eosinophils per highpower (x400 mag) microscopy field
• Exclusion of other possible causes of the
condition
Dellon ES 2013
43
Eosinophilic Oesophagitis
Foods most frequently implicated
in Children
• Egg
• Cow’s milk
• Soy
• Wheat
• Corn
• Peanuts
• Tree nuts
• Shellfish
• Fish
• Beef
• Rye
44
Six-Food Elimination Diet and EoE
Adult study 2013
• Foods eliminated:
– Cereals
• Wheat
• Rice
• Corn
–
–
–
–
–
Milk and milk products
Eggs
Fish and seafood
Legumes including peanuts
Soy
Lucendo et al 2013
45
Six-Food Elimination Diet and EoE
• Indicators of positive outcome:
– Biopsy eosinophil count (< 15/hpf)
– Negative gastro-oesophageal reflux
• Reduced eosinophil count: 73.1% of subjects
• Maintained remission for 3 years
• Incidence of single triggering factors:
–
–
–
–
Cow’s milk 61.9%
Wheat 28.6%
Eggs 26.2%
Legumes 23.8%
• No correlation with allergy tests
46
Eosinophilic Gastroenteritis:
Diagnosis by biopsy:
Abnormal number of eosinophils in the
stomach and small intestine
Foods most frequently implicated
•
•
•
•
Egg
Cow’s milk
Soy
Wheat
•
•
•
•
Peanuts
Tree nuts
Shellfish
Fish
47
Eosinophilic Proctocolitis
Diagnosis by biopsy:
Abnormal number of Eosinophils confined to the colon
Foods most frequently implicated
•
•
Cow’s milk
Soy proteins
Most frequently develops within the first 60 days of life
Is a non-IgE-mediated condition
48
Food Protein Enteropathies
• Increasing recognition of a group of non-IgEmediated food-related gastrointestinal problems
associated with delayed or chronic reactions
• Conditions include:
– Food protein induced enterocolitis syndrome
(FPIES)
– Food protein induced proctocolitis (FPIP)
• These digestive disorders tend to:
– Appear in the first months of life
– Be generally self-limiting
– Typically resolve at about two years of age
49
Food Protein Induced Enterocolitis Syndrome:
Symptoms
Symptoms in infants typically include:
• Profuse vomiting
• Diarrhoea, which can progress to dehydration and
shock in severe cases
• Increased intestinal permeability
• Malabsorption
• Dysmotility
• Abdominal pain
• Failure to thrive (typically weight gain less than
10 g/day)
• In severe episodes the child may be hypothermic
(<36 degrees C)
50
FPIES Characteristics
• Triggered by foods, but not mediated by IgE
• Condition typically develops in response to food
proteins as a result of digestive tract and
immunological immaturity
• Cow’s milk and soy proteins, usually given in
infant formulae, reported as most frequent causes
• Milk and soy-associated FPIES usually starts
within the first year of life; most frequently within
the first six or seven months
• When solids foods are introduced, other foods
may cause the condition
• Recent research claims that rice is the most
common food causing FPIES
51
Cause of the Syndrome
• Immune system reaction in FPIES appears
to involve T helper cells that release the
cytokine TNF-α, which is typical of a Th1
response
• This is in contrast to allergy, in which a Th2
response releases the cytokines that result in
the production of IgE
• Abnormally low level of TGF-, which is
the cytokine most frequently involved in the
development of tolerance to foods, suggests
lack of immunological tolerance
52
Foods Associated with FPIES
Removal of the culprit foods usually leads to
immediate recovery from the symptoms
Foods that have been identified as triggers of FPIES
in individual cases include:
• Milk
• Cereals (oats, barley and rice)
• Legumes (peas, peanuts, soy, lentils)
• Vegetables (sweet potato, squash)
• Poultry (chicken, turkey)
• Egg
53
Prevention of FPIES
• Most reports of FPIES indicate that exclusive
breast-feeding is protective in potential cases of
FPIES
• None of the infants who later developed FPIES
after the introduction of solids had symptoms
while being exclusively breast-fed
• Authors of these studies suggest that babies with
FPIES while being breast-fed were sensitized to
the proteins through an infant formula given
during a period of immunological susceptibility
54
Diagnosis and Management of FPIES
• There are no diagnostic tests for FPIES at
present
• Indicators include clinical presentation :
– development of acute symptoms
immediately after consumption of the
offending foods (often milk- or soy-based
infant formula)
– absence of positive tests for food allergy
• Elimination and challenge with the suspect
foods will usually confirm the syndrome
55
Diagnosis and Management of FPIES
• Removal of the offending food leads to
symptom resolution
• In most cases delayed introduction of solid
foods is advised because of the possibility
that until the child’s immune system has
matured, a similar reaction to proteins in
other foods may elicit the same response
56
Food Protein Induced
Proctitis/Proctocolitis
• Blood in the stool is typical
• Condition typically appears in the first few months
of life, on average at the age of two months
• The absence of other symptoms, such as vomiting,
diarrhoea, and lack of weight gain (failure to
thrive) usually rules out other causes such as food
allergy, and food protein enteropathies
• Usually the blood loss is very slight, and anaemia
as a consequence of loss of blood is rare
• Diagnosis is usually made after other conditions
that could account for the blood, such as anal
fissure and infection, have been ruled out
57
Food Triggers of FPIP
• Most common triggers of FPIP include:
– Cow’s milk proteins
– Soy proteins
– Occasionally egg
• Many babies develop the symptoms during
breast-feeding in response to milk and soy
in the mother’s diet
58
Causes and Management of FPIP
• The cause of FPIP is unknown, but does not
involve IgE, so all tests for allergy are usually
negative
• In most cases, avoidance of the offending food
leads to a resolution of the problem
• When the baby is breast-fed, elimination of milk
and soy from the mother’s diet is usually enough
to resolve the infant’s symptoms
• Occasionally egg can cause the symptoms, in
which case, mother must avoid all sources of egg
in her diet as well
59
Progression of FPIP
• In most cases, the disorder will resolve by
the age of 1 or 2 years
• After this age, the offending foods may be
reintroduced gradually, with careful
monitoring for the reappearance of blood in
the baby’s stool
60
Probiotics
Microorganisms in the Bowel
• The healthy large bowel sustains a resident
microbiota of bacteria, fungi, and other harmless
microorganisms
• Beneficial effects include:
– Synthesis of vitamins:
•
•
•
•
•
Vitamin K
Biotin
Thiamin
Folic acid
Vitamin B12
– Interaction with immune cells to maintain a healthy
epithelium
– Positive competition with invading pathogens to resist
disease
61
Bowel Microflora and Allergy
• The type of gut colonization during the first weeks of life may
predispose an individual to atopic disease
• Microflora of the bowel of a breastfed infant is different from
that of a formula-fed baby
• The gut microflora influences:
– Resistance to infection
– Immunological environment for subsequent challenges,
including food allergens
– May influence predominance of Th1 or Th2 response
• Research studies suggest that lactobacilli and
bifidobacteria may stimulate a Th1 (protective)
response in the digestive tract without causing
disease.
_________________
Kirjavainen et al 1999
62
Clinical Trials of Probiotics
• Not all probiotics have been tested in clinical
studies with regard to allergy prevention or
treatment
• L. bulgaricus seemed to have no effect on
immune parameters, whereas it was associated
with lower frequency of allergies
• L. acidophilus consumption accelerated
recovery from food allergy symptoms
• These effects have also been observed in
infants with eczema and cow's milk allergy
using infant formulas supplemented with
L. rhamnosus.
63
Trials on Probiotics and Eczema Prevention
•
•
•
•
•
Pregnant women took capsules containing
Lactobacillus rhamnosus GG (LGG) during the last
two to four weeks of pregnancy
The newborn infants were given the same
microorganism from birth to six months by spoon
Breast-feeding mothers continued to take the
capsules during lactation
Subjects taking the probiotic had a reduced risk of
developing atopic dermatitis (eczema) compared to
controls up to 4 years of age
Other studies found no reduced incidence of
eczema in babies treated with probiotics
___________
Kalliomaki et al 2003
64
Probiotics and Lactose Intolerance
• Lactobacilli, bifidobacteria and Streptococcus
thermophilus assist in reducing the symptoms of
lactose intolerance
• Produce the enzyme beta-galactosidase (lactase) in
yogurt
• Microbial lactase breaks down lactose
• The fermented milk itself delays gastrointestinal
transit, thus allowing a longer period of time in
which both the human and microbial lactase
enzyme can act on the milk lactose.
65
Microflora and Lactose Intolerance
• Lactose tolerance in people who are deficient in
lactase may be improved by continued ingestion of
small quantities of milk
• Does not improve or affect the production of lactase
in the brush border cells of the small intestine
• Continued presence of lactose in the colon contributes
to the establishment and multiplication of bacteria
capable of synthesizing the beta-galactosidase
enzyme over time
• Resident micro-organisms will break down the
undigested lactose in the colon
• Reduces the osmotic imbalance within the colon that
is the cause of much of the distress of lactose
intolerance
___________
66
de Vrese et al 2001
Status of Probiotics as Therapy
• Great care must be taken in transferring data from
laboratory and experimental animal studies into
human use
• Applies also to the use of known probiotics, some
of which are already present in human nutrition,
such as yoghurt
• Not all strains of bacteria in use as probiotics are
completely harmless
• Their immune-modifying effects and possible
antiallergic and anti-cancer actions require large
clinical studies
67
Potential Allergens in Probiotics
Although probiotics are generally considered to
be safe, there are hazards for the allergic
individual:
– All yoghurts and other fermented milk
probiotic preparations must be avoided by
milk-allergic individuals
– Many probiotic strains, especially
Lactobacillus are grown on media
containing milk proteins, especially casein.
These may be incorporated into non-milk
probiotic products
68
Potential Allergens in Probiotics
– Saccharomyces boulardii is used in
some formulations. Persons allergic to
brewer’s and baker’s yeast
(Saccharomyces cerevisiae) may be
allergic
• There is debate as to whether
Saccharomyces boulardii is a
subspecies of Saccharomyces
cerevisiae or a separate entity.
Traditional techniques cannot
distinguish between the two
69