Starting the Conversation
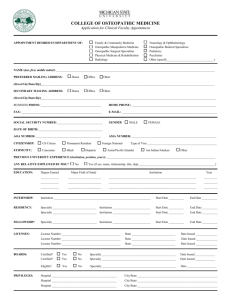
advertisement

AOA Council on Palliatve Care Goals of Care Breaking Bad News Unity Convention October 24, 2010 Bruce Bates, D.O., FACOFP, CMD Chair - Department of Geriatric Medicine University of New England College of Osteopathic Medicine Case 84 y/o W/F living independently, falls at home suffering L femur Fx Undergoes ORIF with post op delerium, dysphagia, renal failure. Aspirates, intubated difficult to wean Attentive daughter Case continued Day #14 – many doctors talk to daughter Nephrologist: making more urine but probably will need dialysis long term Intensivist: able to turn O2 down to 50% Gastroenterologist: plan for a PEG will never eat regular Internist – not doing well Case manager – doctor ordered hospice Daughter calls PCP to complain Objectives . . . Know why defining goals fo care is important Understand a 7-step protocol for delivering bad news Communicate uncertainty and conflict Adjust care to changing goals Importance of Goals of Care Most people want to Know if facing a serious illness Strengthens the physician- patient relationship Fosters collaboration Establishes an appropriate allocation of resources Permits patients, families to plan, cope Potential goals of care Cure of disease Relief of suffering Avoidance of premature death Quality of life Staying in control A good death Support for families and loved ones Maintenance or improvement in function Prolongation of life Osteopathic Tenet THE WHOLE PERSON BODY MIND SPIRIT Multiple goals of care Multiple goals often apply simultaneously Goals are often contradictory Certain goals may take priority over others Patient Centered Care Goals of Patient - initial assessment May Vary over time - ongoing assessment curative palliative self family physical spiritual integrated focused Goals may change Osteopathic Principles make very clear the distinction of caring for disease and caring for the patient who has disease Some goals take precedence over others The shift in focus of care Requires the patient (Guardian) to understand is gradual is an expected part of the continuum of medical care 7-step protocol to communicate bad news . . . 1. Create the right setting 2. Determine what the patient and family know 3. What do they want to Know . . . 7-step protocol to negotiate goals of care 4. Sharing the information 5. Respond with empathy 6. Make a plan and follow-through 7. Review and revise periodically, as appropriate 1. Create the Right Setting Quiet - private space Allot enough open ended time Determine that the right people are present FAMILY CLERGY GUARDIAN OTHER 2. What Does the Patient Know Establish Patients Knowledge and Understanding Asses ability to comprehend Correct misunderstanding Reschedule if unprepared or unresolvable conflict of info 3. How Much Does the Patient Want to Know Recognize patient preferences May decline voluntarily May designate someone to communicate on his/her behalf Consider Power of Attorney or advanced directive – 5 wishes 3. How much does the patient want to know? People handle information differently Capacity Race Ethnicity Religion Education Socio economic Age and developmental level Cultural differences Who gets the information? How to talk about information? Who makes decisions? Ask the patient Consider a family meeting 4. Sharing the Information Say it then STOP Avoid monologue- promote dialogue Avoid Jargon and Euphemisms Pause frequently Validate understanding Use Silence and Body Language Don’t minimize severity Implications of “I’m Sorry” Language with unintended consequences -Negative Do you want us to do everything possible? Will you agree to discontinue care? It’s time we talk about pulling back I think we should stop aggressive therapy I’m going to make it so he won’t suffer Language to describe the goals of care positive . . I want to seek the most comfort and dignity possible until the day you die We will concentrate on improving the quality of your child’s remaining life Let’s discuss your needs and wants 5. Respond with Empathy Affective response Tears anger sadness love anxiety relief Cognitive response Denial blame guilt disbelief fear loss shame Basic psychophysiologic response Fight – Flight 5. Respond with Empathy Listen Listen Listen Encourage descriptions of Feelings Use Non Verbal communication Physician: Acknowledge Yurself 6. Planning and followup Explore what their hopes expectations and Fears are Plan for Next Steps Added tests, treatment/non treatment, Care vs cure, referrals Sources of Support for patient/family Medical, spiritual, emotional, social, legal 7. Review and Revise Give Contact info / next appointment Assess Safety Assess informal and formal support Be Prepared to repeat info at next visit – it was not all heard Goals Change with time and progression of condition Reviewing goals, treatment priorities Goals guide care – whose? Assess priorities to develop initial plan of care Review with any change in health status advancing illness setting of care treatment preferences Communicating prognosis Providers markedly over-estimate prognosis Either way raises fears and stresses Helps patient / family cope, plan increase access to hospice, other services Offer a range or average for life expectancy Truth-telling and maintaining hope False hope may deflect from other important issues True clinical skill to help find hope for realistic goals When Family Says: “Don’t Tell” Ask Family Why not? What are you afraid I will say? What are previous experiences? Personal,religious, or cultural context? Patient knows something - why this conspiracy? Will it feed mistrust? Talk To patient together Legal Obligation to obtain consent to treat or not treat (assuming capacity) Determine specific priorities Based on Patient values, preferences, clinical circumstances Influenced by information from physician(s), team members, Patient and family Clinical Jazz Summary Begin the conversation Early Keep seven steps in mind Understand the Goal of Care Patient centered values and preferences Seek permission to involve family and others Give Permission to react/accept/reject Revise and renew IATP IT’s ABOUT THE PATIENT