8af607ad-cdc9-4e07-8435
advertisement

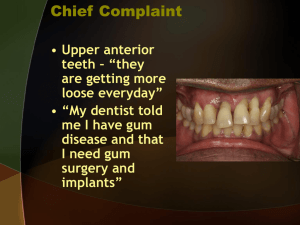
Anti-infective Therapy Dr Manal Ahmad Abu Al Ghanam Definitions Chemotherapeutic agent: acts to reduce the number of bacteria present. Antibiotic: naturally occuring semisynthetic or synthetic type of anti-infective agent. Antiseptic: a chemical antimicrobial agent applied topically or subgingivally. Route of administration Systemic: may be a necessary adjunct in controlling bacterial infection. Local: directly into the pocket has a potential to provide greater concentrations. A single agent can have a dual mechanism of action (tetracyclines) Systemic administration of antibiotics 1. 2. 3. 4. 5. Treatment of periodontal disease is based on infectious nature of the disease. An ideal antibiotic for use in prevention and treatment of periodontal disease: Specific for perio. pathogens. Allogenic. Nontoxic. Substantive. Inexpensive. Systemic administration of antibiotics 1. 2. 3. 4. The treatment of the individual patient is based on: Patient’s clinical status. Nature of colonizing bacteria. Ability of the agent to reach the site of infection. Risks and benefits associated with the proposed treatment. Systemic administration of antibiotics 1. 2. 3. 4. 5. 6. 7. The clinician is responsible for choosing the correct antimicrobial agent. Some adverse reactions include: Allergic/anaphylactic reactions. Superinfections of opportunistic bacteria. Development of resistant bacteria. Interaction with other medications. Upset stomach. Nausea. Vomiting. Tetracyclines: Used widely in perio.disease treatment. Used frequently in treatment of refractory periodontitis and LAP. Has the ability to concentrate in the periodontal tissue and inhibit the growth of Aggregatibacter actinomycetemcomitans. Exert an anticollagenase effect that can inhibit bone destruction and may aid bone regeneration. Tetracyclines: Bacteriostatic….effective against rapidly multiplying bacteria. G+ve>>G-ve bacteria. Concentration in gingival crevice 2-10 times in serum. Long term regimens can develop resistant bacteria. Tetracycline HCL Administration 250mg 4 times daily (qid). Inexpensive Side effects: GI disturbances, photosensitivity, increased blood urea nitrogen, tooth discoloration when administered to children up to 12 years. Minocycline Suppresses spirochetes and motile rods. Given twice daily (bid) facilitating compliance. Less photosensitivity and renal toxicity. Side effects: are similar to those of tetracycline however there is increased incidence in vertigo. Only tetracycline that can discolor permanently erupted teeth and gingival tissue when administered orally. Doxycycline 1. 2. 3. Has same spectrum as minocycline,but only given once daily(qd) more compliant!! Most Photosensitizing Agent In Tetracyclines. DOSES: Antiinfective agent; 100mg qd or 50mg bid . Sub antimicrobial (inhibit collagenase) 20 mg twice daily. Periostat!! Metronidazole Nitroimidazole compound developed for protozoal infection. Bactericidal to anaerobic organisms because it disrupts the bacterial DNA. Effective against P.g and P.i but not the drug of choice against A.a unless combined to other antibiotics!!!! Metronidazole 1. 2. 3. 4. 1. 2. Used to treat: Gingivitis. Necrotizing ulcerative gingivitis. Chronic periodontitis. Aggressive periodontitis. Doses: 250mg 3 times daily(tid) for a week. Arestien.(local delivery sustained release form). Metronidazole 1. 2. 3. 4. 5. Side effects: Antabuse effect when alcohal is ingested. Inhibits warfarin metabolism. Patient on anticoagulant should avoid prothrombin time. Should be avoided in patients on lithium. Metallic taste in mouth. Penicillins Most widely used antibiotic. Inhibit bacterial cell wall production and so they are bactericidal. Induce allergic reactions and bacterial resistance. Amoxicillin and amoxicillin-clavulanate potassium (Augmentin). Penicillins Amoxicillin is semisynthetic penicillin with extended antiinfective spectrum (G+ve,G-ve) Amoxicillin is for treatment of aggressive periodontitis both localized and generalized forms. Augmentin is used for management of LAP or refractory periodontitis. Cephalosporins Are not used for treatment of dental disease. Patients allergic to penicillin are allergic to cephalosporins. Clindamycin Effective against anaerobic bacteria with strong affinity for osseous tissue. For penicillin allergic patients. Efficacy to periodontitis refractory to tetracycline therapy. DOSES:150mg (qid) for 10 days. 300mg(bid) for 8 days. Associated with pseudomembranous colitis. Ciprofloxacin A quinolone active against gram negative rods (all facultative, some anaerobic putative periodontal pathogens). Ciprofloxacin therapy may facilitate establishment of a microflora associated with periodontal health. ONLY antibiotic that all strains of A.a are susceptible. Ciprofloxacin Side effects: metallic taste, inhibit the metabolism of theophilline and caffeine, enhance the effect of warfarin and other anticoagulants. Macrolids Inhibit protien synthesis,bacteriostatic or bactericidal depending on drug concentration. Macrolids used in periodontal treatment include erythromycin,spiramycin,and azithromycin. DOSES: Therapeutic doses of 250mg/day for 5 days after an initial loading dose of 500mg. Macrolids DID YOU KNOW…. Erythromycin is not concentrated in GCF, spiramycin is excreted in high concentration in saliva and it has been proposed that azithromycin penetrates fibroblasts and phagocytes in concentrations 100-200 times greater than extacellular compartment!!! SERIAL AND COMBINATION ANTIBIOTIC THERAPY Periodontitis is a mixed infection, in this condition treatment requires more than one antibiotic serially or in combination!!!!! Bacteriostatic drugs require rapidly dividing microorganisms, they do not function well with bactericidal antibiotics!!!! If both types are required then it is best to use them serially not in combination. SERIAL AND COMBINATION ANTIBIOTIC THERAPY Bacteriostatic Bactericidal Erythromycin Penicillin Tetracycline Cephalosporin Clindamycin Vancomycin Metronidazole Guidelines for antibiotics in periodontal therapy 1. 2. 3. 4. 5. Clinical diagnosis and situation dictate the need for ABC therapy. Disease activity, measured by continuing attachment loss, purulent exudates… Patient medical and dental status and current medication. Microbiological plaque sampling. Identification of which antibiotics were most effective… Local Delivery Agents Subgingival chlorhexidine . Tetracycline containing fiber. Subgingival doxycycline. Subgingival minocycline. Subgingival metronidazole. Subgingival Chlorhexidine A resorbable delivery system. Biodegradable system that resorbs in 7-10 days. No signs of staining were noted in any of the studies!! Tetracycline containing Fiber Tetracycline fibers with 12.7mg per 9 inches. It was well tolerated in oral tissues and concentrations reach 1300µg/ml No change in antibiotic resistance to tetracycline was found !! Subgingival Doxycycline A gel system using a syringe with 10% doxycycline (Atridox). Subgingival Minocycline A locally delivered sustained release form of minocycline microspheres (arestin). The 2% minocycline is encapsulated into bioresorbable microspheres in gel carrier. Subgingival Metronidazole A topical medication containing an oil based metronidazole 25% dental gel. Two 25% gel application at a 1-week interval have been used. Bleeding on probing was reduced by 88% of cases. Conclusions Scaling and root planing are effective in reducing pocket depths. When systemic antibiotics are used as adjuncts to scaling and root planing the evidence indicate that some antibiotics provide additional improvement. There are extensive reviews of the local delivery agents available for periodontitis.