Chapter 10 ss Contraception
advertisement
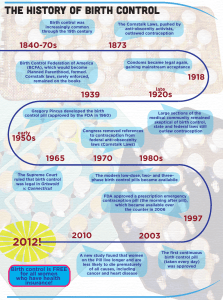
Chapter 10 Contraception Historical and Social Perspectives • Evidence of contraception since the beginning of recorded history • U.S. contraceptive efforts – 1800s Comstock laws: – 1915: Margaret Sanger • Opened illegal clinic. • The Woman Rebel. – U.S. Supreme Court rulings • Griswold vs. Connecticut (1965)- Married couples. • Eisenstadt vs. Baird (1972) - Unmarried individuals. – Today:Far-Right politics, denying contraceptive to 3rd world. Pro-Life anticontraception politics. Contraception as a contemporary issue - in the U.S. • Allows couples to plan for wanted children, establish relationship, financial stability • Allows women to pursue professional life with more freedom • Can increase women’s health – Pregnancy itself has health risks, spacing pregnancies at least 18 months apart results in better health for both mothers and children • Increased pressure to mandate health insurance coverage for prescription contraceptives – Many health insurance companies covered Viagra before they covered the pill – Coverage has increased, but is still not universal Sex, politics, & contraception • Many pro-life religious groups oppose contraception and want to prevent access to it. – Don’t see contraception as a way to prevent abortion, but as “a gateway to abortion” (American Life League) – Many pro-life groups embrace traditional role of women staying home raising children as the ideal – Has led to decreased funding for clinics that provide free or affordable birth control, and a higher rate of abortion. • View access to contraception as a threat b/c it helps women expand their roles into traditionally male realms of work & politics • Bush administration – Political influence of these groups has increased – Anti-contraception policies have been extended globally • international anti-contraceptive organizations • Bush admin’s refusal to release $34 million that Congress appropriated to provide contraception and reproductive health services internationally Contraception as a global issue • Helps curtail global population growth & spread of HIV – Most successful way to reduce population growth worldwide is to expand women’s educational and economic opportunities – Worldwide, women w/more education have fewer children • Different cultures and religions have different views about contraception – EX: Catholic church forbids contraception (other than abstinence and cycle-based methods), though 70% of American Catholics use contraceptive methods forbidden by the Church A look at the state of Kerala in India • Primarily rural, similar to rest of India; income level also not different from rest of India • Why does Kerala have such a low birth rate and infant mortality rate? • High rate of women’s literacy (85% in Kerala, compared w/<40% in India on avg) • Higher status for women in Kerala- women can own land; rather than having to pay a dowry to marry a woman off, women in Kerala bring their families a brideprice & are considered an asset to the family Sharing responsibility in choosing a birth control method • Sharing responsibility is in the interest of both partners – Can enhance relationship trust – Can be a good way to practice discussing personal & sexual topics – Women respect men who share responsibility and often resent men who do not. – Men shouldn’t assume that a woman is “taking care of it” – Dealing w/an unplanned pregnancy is difficult • How to share responsibility – – – – ask about BC before intercourse read & discuss options together attend a class or clinic together share expenses Choosing a Birth Control Method things to consider • Effectiveness--statistics show two numbers: – Failure rate: # of women per 100 who become pregnant after 1 yr. when using a b.c. consistently & correctly – Typical use failure rate--takes into account improper or inconsistent use • Factors that contribute to improper use include: lack of partner involvement, forgetfulness, feeling guilty about sex, poor communication w/partner, not wanting to appear “easy” – About half of all unintended pregnancies occur among women using contraceptives • Cost • Ease of use • Side effects Effectiveness of birth control methods Also see Table 10.1 p. 268 w/o spermicide FDA, 1997 Using backup methods to increase contraceptive effectiveness • Backup methods: contraceptive methods used simultaneously w/another method to support it • Condoms, foam, diaphragm, can all be combined w/other methods for extra protection • When a backup method might be a good idea: – If on the pill: • During first cycle of the pill • After forgetting 2 or more pills, or after several days of diarrhea or vomiting when on the pill • First month after switching pill type • When taking medications that can reduce effectiveness of the pill – During first 1-3 months after IUD insertion – When first learning how to use a new method – To increase overall effectiveness of contraception “Outercourse” …is to prevent pregnancy, not to protect against STI’s • Noncoital forms of sexual intimacy • Kissing, touching, mutual masturbation, oral sex, anal sex • Any type of sexual intimacy that avoids male ejaculation near vaginal opening • Can be primary or temporary means of preventing pregnancy • Can also be used when it’s not advisable to have intercourse for other reasons, such as after childbirth or abortion • No undesirable contraceptive side effects • Does not eliminate chances of spreading STDs, especially if it involves oral or anal sex Hormone-based contraceptives 5 types 1) Oral contraceptives (pills) 2) Vaginal ring 3) Transdermal patch 4) Injected hormones 5) Hormonal IUDs Gonadotropin releasing hormone (GnRH) triggers release of gonadotropins FSH & LH How hormonal contraceptives work FSH & LH trigger ovulation Estrogen & progesterone in hormonal contraceptives inhibit LH, FSH, and GnRH secretion, preventing ovulation Progesterone also: •thickens cervical mucus to prevent Passage of sperm into the uterus •changes uterine lining to inhibit implantation Types of oral contraceptives • Constant-dose combination pill – Contains both estrogen and progestin – Dose of each is constant throughout cycle – Amount of estrogen in pills has decreased from approx. 175 micrograms in 1960 to avg. of 25 micrograms today • Triphasic pill – Levels of hormones (estrogen & progestin) fluctuate during cycle • Seasonale – Reduces the # of menstrual periods to 4 instead of 13 per year – Has lower dose of estrogen and progestin • Progestin-only pill – Low dose of progestin and no estrogen – For women who should not take estrogen (breastfeeding, high b.p., at risk for blood clots, smoke) How to use oral contraceptives • Different types of OCs will differ in how to begin, and other instructions--read instructions carefully & talk w/health care practitioner • Don’t skip pills, regardless of whether or not you are having sex • Take pill at the same time each day – If you miss 1 pill: take missed pill as soon as you remember, and then take next pill at the regular time – If you miss >1 pill: consult health care practitioner for advice; use a backup method for remainder of your cycle Oral contraceptives possible side effects & health issues • Women who should not take OCs: – history of blood clots, strokes, heart/circulation problems, jaundice, breast or uterine cancer, liver disease • Women considered risky for taking OCs: – Women who smoke, have migraines, depression, high b.p., epilepsy, diabetes/prediabetes, asthma, varicose veins • Side effects of OCs can include: – Weight gain, decreased sexual interest, headaches, mood changes, nausea, bleeding between periods – May clear up after 2-3 cycles on the pill Oral contraceptives possible side effects & health issues • Rare but serious side effects of OCs--must be reported to a health care practioner ASAP 10.3 Other hormonal methods (contain both estrogen and progestin) • Vaginal ring (Nuvaring) – 2” ring inserted into the vagina during period – Worn for 3 weeks, removed for 1 week, then replaced with new ring – Cost per year: $580 – Pros: no daily pill; spontaneity – Cons: no STD protection, not effective for women over 198 lbs. • Transdermal patch (Ortho Evra) – Patch is placed on buttock, abdomen, outer upper arm, or upper torso – Replaced weekly for 3 weeks, then a patchfree week – Cost per year: $420 – Pros: no daily pill; spontaneity – Cons: no STD protection, skin irritation Other hormonal methods • Injected Contraceptives – – – – – Depo-Provera (prog.); Lunelle (prog.+est.) Injections: D-P every 12 weeks; Lunelle monthly Cost per year: $196 for D-P; $420 for Lunelle Pros: no daily pill; spontaneity Cons: no STD protection, weight gain, bleeding, mood change, frequent clinic visits – D-P: takes up to 10 months for a woman to get pregnant after stopping injections • Contraceptive Implants – – – – – – 1.5” rod is inserted under skin of upper arm Progestin-only Effective for up to 3 years Cost not yet known Pros: no daily pill; spontaneity Cons: no STD protection, weight gain, bleeding, mood change, surgical procedure (cont.) Barrier & spermicide methods • Include: – Condoms (male & female) – Spermicides (foam, sponge) – Cervical barriers (diaphragm & cervical cap) • Work by preventing sperm from reaching an egg • Only condoms provide protection against STIs Condoms (male) • Sheath that fits over the erect penis • The only temporary method of birth control for men • Only form of contraception that effectively reduces STI transmission • Made of thin latex, polyurethane, or natural membrane – Natural membrane (from sheep intestines) condoms can permit passage of viruses, incl. those that cause AIDS, herpes, hepatitis, HPV • Many varieties – Different features, shapes, textures, colors, flavors – Some “extended pleasure” types have a desensitizing agent on the inside to delay ejaculation – Lubricated or nonlubricated • Note: average shelf life of condoms is 5 years; don’t store latex condoms in hot places (glove compartment, back pocket) b/c heat can deteriorate the latex How to use the (male) condom • Pinch reservoir tip or twist tip of nonreservoir tip condom before unrolling condom over the penis to leave room for ejaculate-reduces chance of condom breaking • Unroll condom over erect penis before any contact between the penis and vulva occurs – Common error: putting on a condom after vaginal penetration but before ejaculation--increases risk of pregnancy & STI transmission • Use a water-based lubricant to reduce risk of condom breaking (oilbased lubricants deteriorate condom) • Hold condom at the base of the penis before withdrawing from the vagina to avoid spilling semen inside vagina Female condom • Consists of two flexible polyurethane rings and a soft, loose-fitting polyurethane sheath – One ring at closed end fits loosely against cervix; other ring at open end encircles the labial area • Can be inserted before sexual activity; don’t need to remove it immediately following ejaculation Costs, pros, & cons of condoms • Costs – Male condoms, about $0.75-$1 each – Female condoms, about $3 each • Advantages – STI protection! – Available w/o prescription or medical intervention • Disadvantages – Can reduce sensation • Polyurethane transmits heat well, so some say that the female condom has less reduction in sensation – Interruption of sexual experience (though some couples find sensual ways of incorporating condoms into foreplay) – Note: female condom can be inserted several hours before intercourse Vaginal spermicides • Include: foam, sponge, suppositories, creams, film • Spermicide: chemical that kills sperm (nonoxynol-9) • Cost: $0.85 per application • Advantage: no prescription necessary • Disadvantages: – Interruption of sexual experience (except for the sponge) – Skin irritation (which can increase susceptibility to STI infection) – No protection from STIs – Not effective enough to be used w/o a condom or other method Cervical barrier devices • Covering the cervix is one of the oldest methods in contraceptive history – Casanova (18th century Europe) promoted using squeezed-out lemon half; European women shaped beeswax to cover cervix diaphragm FemCap Cerv cap Lea’s shield • Cervical cap: covers cervix only • Diaphragm: covers upper vaginal wall behind cervix underneath pubic bone • FemCap & Lea’s shield have removal straps • Lea’s Shield allows a one-way flow of fluid from cervix to vagina • Method is usually combined w/spermicide How to use cervical barrier devices • Diaphragm & cervical cap: need to be fitted (may need to be refitted w/weight gain or loss >10 lbs.) • FemCap & Lea’s Shield do not have to be fitted, but still require a prescription in the U.S. • Use diaphragm & cervical cap only with water-based lubricants b/c they are latex (FemCap & L.S. are silicone) • Can insert up to 6-8 hr. before intercourse; should leave in at least 8 hr after Placement of cervical barrier devices (& FemCap) Intrauterine Devices (IUDs) • Small plastic objects into uterus • 2 types – Hormone-releasing – Copper-releasing inserted (progesterone) progesterone • Have fine plastic threads attached that hang slightly out of cervix into vagina for removal • Very high continuation rate (how many women are still using it one year after starting) compared w/other methods IUD Mechanisms of Action Levonorgestrel-Releasing IUD (LNG-IUS, Mirena®) – Inhibits fertilization – Thickens cervical mucous – Inhibits sperm function – Thins and suppresses the endometrium Copper-Releasing IUD (ParaGard® T380A) – Inhibits fertilization – Releases copper ions (Cu2+) that reduce sperm motility – May disrupt the normal division of oocytes and the formation of fertilizable ova Jonsson B, et al. Contraception. 1991;43:447-458; Videla-Rivero L, et al. Contraception. 1987;36:217-226; Kulier R, et al. Cochrane Database Syst Rev. 2006;3: CD005347. Costs, pros, & cons of IUDs • Costs – Copper: $550 (good for up to 10 years) – Hormone: $500-$700 (good for up to 5 years) • Advantages – – – – – Very effective (essentially no “user error”) Long-term protection No interruption of sexual activity Don’t have to remember to use Can be used during breast-feeding • Disadvantages – No STI protection – Risk of PID (usually within first 1-2 months following insertion) – Rare incidence of perforating uterine wall Emergency Contraception • Works mainly by preventing ovulation or fertilization • In theory, can also interfere w/implantation – Evidence suggests this is not primary mechanism of action • If it was, efficacy should not decrease w/short-term delay, as long as EC was administered some time before implantation • However, EC is increasingly less effective w/delay • Oral contraceptive pills – – – – 95% effective within 24 hrs; 75% effective within 72 hrs Preven: 2 doses of combined estrogen & progesterone Plan B: 2 doses of progesterone Other combinations of oral contraceptives can substitute for these (see Table 10.7, p. 283) • Copper-T IUD – 99% effective if inserted within 5 days Fertility Awareness Methods • Standard days method – For women w/cycles btwn 26 & 32 days – Couples avoid unprotected intercourse btwn days 8-19 of each menstrual cycle – Highest rate of effectiveness of natural family planning methods • Mucus method: based on cyclical changes – Vaginal secretions change throughout cycle; woman learns to “read” these changes and keeps a daily chart • Calendar method: self- knowledge of fertility – After charting cycles for some time (preferably 1 year), a woman estimates the time she is ovulating based on the calendar • Basal body-temperature – Based on changes in body temperature around ovulation • Often, some combination of these methods will be used Standard Days Method (w/Cyclebeads) 1 On the day you start your your period, move the ring to the RED bead. If you have not started your period by the day after you put the ring on the last brown bread, contact your provider. If you start your period before you put the ring on the darker brown bead, contact your provider. (may not be a good method for you) On BROWN bead days you can have intercourse with very low probability of pregnancy. Also, mark this date on your calendar 2 Every morning move the ring to the next bead. On WHITE bead days you can get pregnant. Always move the ring from the narrow to the wide end. Avoid unprotected intercourse to prevent a pregnancy. Arevalo M et al., Contraception, 2002;65:333-338. When you start your next period, move the ring directly to red bead and begin again. Cervical Mucus Method no unprotected intercourse Early Mucus Transitional Mucus Highly Fertile Mucus • Slight amount • Thick • White • Sticky • Holds its shape • Increasing amounts • Thinner • Cloudy • Slightly stretchy • Profuse • Thin • Transparent • Stretchy Stanford JB, et al. Obstet Gynecol. 2003;101:1285-1293. Calendar or Rhythm Method 8 Low-risk Days Egg may still be present These days may be unsafe if 28-day cycle varies as much as 8-9 days between shortest and longest cycles. Intercourse on these days may leave live sperm to fertilize egg. Ovulation Billings JJ. Med J Aust. 1978;2:436. Byer/Shainberg/Galliano. Dimensions of Human Sexuality, 5e. 1999, The McGraw-Hill Companies, Inc. Basal Body Temperature Method • BBT=body temp in resting state on waking • Slight drop immediately before ovulation • After ovulation, release of progesterone causes slight increase in temperature Fertility Awareness Methods pros & cons • Pros: – – – – Essentially free No medical side effects Does not interrupt sexual activity Woman gains awareness about her body and natural cycles, which can increase comfort w/sexuality – Acceptable to Catholic Church • Cons: – No STI protection – Requires some degree of discipline in order to keep track of calendar/charts, etc. – Need to abstain from intercourse or use a backup method during fertile days Sterilization • Essentially permanent, although vasectomies are sometimes reversible • Does not affect hormones, desire, sexual functioning • Female sterilization – Tubal sterilization: fallopian tubes are severed to block passage of sperm & eggs – Transcervical sterilization: tiny coil inserted through cervix into fallopian tubes • Coil promotes tissue growth that, after 3 months, blocks fallopian tubes • Male sterilization (vasectomy) – Safer, less expensive, fewer complications than female sterilization – Cutting and closing vas deferens (ducts that carry sperm) Ex. of female sterilization procedure • Laparoscope: narrow, lighted viewing instrument that is inserted into abdomen to locate the fallopian tubes Ex. of male sterilization procedure • Vas deferens on each side is cut; small section is removed, and the ends are tied off or cauterized Less than Effective Methods • Nursing – amenorrhea is common for a brief period after birth while breastfeeding – 80% of women ovulate before first period (and so do not know that they are fertile) • Withdrawal before ejaculation – – – – difficult to judge when to withdraw anxiety may lower pleasure for both partners Cowper's gland fluid may carry sperm any sperm on vulva may travel into vagina/uterus • Douching – sperm reach uterus in 1-2 minutes – douching may speed sperm along – irritates vaginal tissue New Directions in Contraception for men • The “male pill”: Testosterone & progestin may lower sperm count • New forms of reversible vasectomy – Injection of a blocking gel into vas deferens; gel is dissolved to reverse the procedure – Insertion of two plugs into each vas deferens-can be removed later New Directions in Contraception for women • Most new developments are improvements on existing contraception for females – Variations on methods of delivery, formulation of hormones – New designs of IUDs, female condoms – spermicides with microbicides (to kill microbes that cause STIs) Discussion question: Should women convicted of child abuse be mandated to use “doctor-certified” contraception (e.g. injected/implanted hormonal contraceptive, or IUD)?