Payment Reform & Cost Containment: What You Need to Know
advertisement

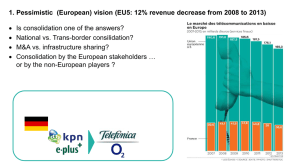
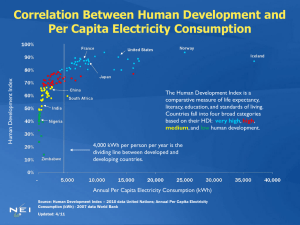
Payment Reform & Cost Containment: What You Need to Know Monday, February 13, 2012 Some Facts About the MA Market • 98% of resident insured in Massachusetts. • Commercial Market: 50% self insured, 50% fully insured. • Of those fully insured, 50% in PPO and 50% in HMO • 47 mandated benefits; 8 added since health reform passed • Mandates are not required to be covered by self insured companies • Fall exclusively on individuals, small businesses and mid-size companies • MA health care costs among highest in the nation. Why We Need to Care About Health Care Costs? MA: A model for the federal law; Best record on access Affordability is Another Story 600 Growth in Health Spending in MA Expected to Surpass Other Economic Indicators Index of Health Expenditures Per Capita and Other Indicators in MA, 1991-2020 Per Capita Health Expenditures: 550 in 2020 550 500 450 400 Per Capita GDP: 337 in 2020 350 300 Wage and Salary: 325 in 2020 250 200 Consumer Price Index (CPI): 224 in 2020 150 100 91 92 993 994 995 996 997 998 999 000 001 002 003 004 005 006 007 008 009 010 011 012 013 014 015 016 017 018 019 020 19 19 1 1 1 1 1 1 1 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 Per Capita Health Expenditures Per Capita GDP in MA Average Wage and Salary in MA CPI Boston source: Division of Health Care Finance & Policy, MA Health Care Cost Trends, Nov. 2009 What Does the Data Tell Us? Health Plan & Hospital Margins - 2010 sources: Health plan & hospital filings with the Division of Health Care Finance & Policy and Division of Insurance What Does the Data Tell Us? “Price variations are correlated to market leverage – the relative market position of the hospital or provider group compared with other hospitals or provider groups within a geographic region or within a group of academic medical centers.” “Price increases, not increases in utilization, caused most of the increases in health care costs during the past few years in Massachusetts.” “Higher priced hospitals are gaining market share at the expense of lower priced hospitals, which are losing volume.” Office of the Attorney General Examination of Health Care Cost Trends and Cost Drivers March 16, 2010 What Does the Data Tell Us? “Prices paid for the same hospital inpatient services and for physician and professional services vary significantly for every service examined. There was at least a three-fold difference for every service and for most, a variation of six- or seven-fold.” “If private payer prices among hospital inpatient services and physician and professional services were narrowed to reflect a range spanning the existing 20th percentile to 80th percentile of payments, the potential total savings for these two groups of services would be about $267 million.” Massachusetts Division of Health Care Finance & Policy MA Health Care Cost Trends, Price Variation in Health Care Services May 2011 What Does the Data Tell Us? If private payer prices among hospital inpatient services and physician and professional services were narrowed: Professional Services Inpatient Hospital Services Total Savings/Increase Payments paid at 2009 median $640MM $112MM $752MM All payments above the 80th percentile lowered to 80th percentile $320MM $170MM $490MM Lowering rates above the 80th percentile & increasing rates below the 20th percentile $179MM $88MM $267MM Massachusetts Division of Health Care Finance & Policy MA Health Care Cost Trends, Price Variation in Health Care Services May 2011 What Does the Data Tell Us? “There is wide variation in the payments made by health insurers to providers that is not adequately explained by differences in quality of care. Globally paid providers do not have consistently lower total medical expenses.” “Promote tiered and limited network products to increase value-based purchasing decisions.” “Reduce health care price distortions through temporary statutory restrictions until tiered and limited network products and commercial market transparency can improve market function.” Office of the Attorney General Examination of Health Care Cost Trends and Cost Drivers June 22, 2011 What Does the Data Tell Us? What Does the Data Tell Us? What Does the Data Tell Us? What are the Reasons for High Health Care Costs? AG & DHCFP reports & hearings in 2010 & 2011: • Price is the #1 driver of health care costs, not utilization • More and more care being delivered in high cost settings. • Certain providers have used their market clout & geographic isolation to drive prices in the Massachusetts • Prices aren’t based on quality outcomes or severity of patient illnesses or case mix. • High costs do not equal high quality. Many high quality providers among the lowest paid. • High public payer case mix does not translate into higher payments. Those with the highest Medicaid volume are among the lowest paid. • How you pay does not = lower costs – some globally paid providers among the highest paid. • AG called for short term Government intervention to address provider rate distortions The State’s Response 2010 • Chapter 288 of the Acts of 2010 • Requires carriers to develop tiered and limited network products with 12% savings off of lowest priced plan. • Additional financial reporting by health plans and providers. • Nation’s strictest MLR standards, limits to annual increases to administrative spending, and limits on profit or surplus to 1.9%. The State’s Response 2011 • Governor’s Payment Reform Bill – Key Provisions: • Move from FFS to alternative payment methods; • Standards for ACOs; • Directs DOI w/ DHCFP to set annual rates of provider reimbursement; • DOI may establish different amounts for different categories of providers • Based on criteria such as: • • • • Annual increases to GDP Total Medical Expense Relative Price Price variation • Health plan rates will be denied if they exceed these parameters; • Greater government oversight and time frames to move to alternative payment methods How Will This Change the Health Care System? ACOs • Spurred by Medicare Pioneer ACO Pilot • Goal is to: • Reward physicians for quality outcomes not volume thru alternative payment models • Create an integrated care delivery system with EMR and robust data • Primary Care Physicians as the quarterback for a patient’s care • Physicians manage the care and risk of patient population Will We See A Payment Reform Bill Before July 31, 2012 In Address, Guv to Focus on Pending Priorities: Health Care, Sentencing – January 23, 2012 House Chairman Sees Billions in Savings, Pledges “Boldest” Health Care Bill – January 25, 2012 Moore Eyes Health Care Bill By March, Mariano Touts Short-Term Plans – February 8, 2012 Speaker DeLeo: “I remain committed to reforming our health care system… We will continue to monitor the market disparity between our large providers and those in your neighborhoods that are offering low-cost high-quality care and we will thoughtfully implement the most appropriate mechanisms for balancing out the system.” – February 8, 2012 How Will Health Care Change? The Potential Transition • A move towards ACOs, greater integration, alternative payment methods where providers are rewarded for good quality outcomes rather than volume • We will, and are seeing, potential for greater consolidation in the health care market with just the simple discussion of ACOs Will greater consolidation lead to higher prices? Payer consolidation leads to lower prices while provider consolidation leads to higher prices.* Sept. 2011 Health Affairs *”The Increased Concentration of Health Plan Markets Can Benefit Consumers Through Lower Hospital Prices,” Health Affairs, September 2011. How Will Health Care Change? For a successful transition • PCPs to be the quarterbacks for patient care with a shared philosophy by providers across specialties to work with the PCP as part of an integrated team; • Provider understanding of how to manage risk; • EMR and integration of care management systems; and • Consumers engaged in their health care and willing to take restricted choice for a better care experience Key Questions to Ask About Payment Reform • • • • • • • Will changing the way we pay really save money? How does this address market power? How long do we have to wait for a return on investment? Will changing the way we pay lead to market consolidation? Will consolidation lead to lower or higher costs in the long run? What does this mean for choice? How do we ensure providers have control over where patients get care? • What does this mean for products available to employers? • How does this affect self-insured employers? MAHP’s Position Any Final Bill Must • Truly address containing costs; • Address the AG's findings re: market power – fix the foundation • Not mandate payment methods or ACOs – should incorporate a voluntary approach to new payment methods and ACOs • Not limit employer or individual choice in the market place • Ensure appropriate regulatory and consumer protection standards for AC0s and for providers taking risk • Not mandate use of health plan reserves to pay for provider infrastructure What Can Employers Do? You have an important voice Get Involved