Uterine Myoma Uterine Fibroids, Leiomyomas, Myomas, Fibromyomas
advertisement
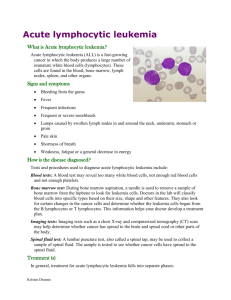
Acute Lymphoblastic Leukemia I2 黃 柏 瑋 Malignancy remains the major cause of death to disease between the age of 1 and 15 years The precise cause of childhood cancer is unknow Leukemia, Neuroblastoma, Wilms tumor , retinoblastoma and tumor of liver Introduction Leukemia – the most common malignancy in childhood. Acute leukemia– 97% Acute lymphoblastic leukemia– 75% Acute myeloblastic leukemia– 20% Chronic leukemia– 3% Chronic myelogenous leukemia (Ph positive) Juvenile myelomonocytic leukemia ( JMML) Introduction to pediatric neoplastic disease and tumor Leukemia and a more pronounced rise in central nervous system tumor Boy > girl Leukemia The most common childhood cancer ( 1/3 of pediatric malignancies ). Acute lymphoblastic leukemia (ALL) represents about 75 % (peak incidence at age 4 years). Acute myeloid leukemia (AML) accounts for about 20 % of leukemia (stable from birth through age 10) Others : CML Acute Lymphoblastic Leukemia Childhood acute lymphoblastic leukemia (also called acute lymphocytic leukemia or ALL). is a disease in which too many underdeveloped infection-fighting white blood cells, called lymphocytes, are found in a child's blood and bone marrow. Acute Lymphoblastic Leukemia These abnormal cells reproduce very quickly and do not function as healthy white blood cells to help fight infection. the most common form of leukemia the most common kind of childhood cancer. Acute Lymphoblastic Leukemia In the United States, about 3,000 children each year are found to have ALL Peak incidence occurs from 3 to 5 years of age. Acute Lymphoblastic Leukemia the most common symptoms of leukemia:fever, anemia, bleeding and/or bruising ,persistant weakness or tiredness, achiness in the bones or joints, recurrent infections , difficulty breathing (dyspnea) or swollen lymph nodes. Clinical manifestations Protean Bone marrow failure & Organ infiltration Common symptoms Fever ( 60%) Malaise ( 50%) Pallor ( 40%) Etiology Unknown ( usually) Hereditary Down’s syndrome Leukemia in siblings Chemicals Chronic benzene exposure Alkylating agents Ionizing radiation Predisposing hematological disease ( MPD, AA) Viruses ( HTLV-1) Diagnostic criteria ALL is often difficult to diagnose. The early signs may be similar to the flu or other common diseases. Diagnostic criteria bone marrow aspiration and biopsy complete blood count (CBC) additional blood tests computerized tomography scan magnetic resonanec imaging (MRI) x-ray ultrasound lymph node biopsy spinal tap/lumbar puncture Diagnostic criteria Peripheral blood: anemia,thrombocytopenia, variable white cell count with or without blasts. Bone marrow: hyper-or hypo-cellularity with excess of blasts (blasts>30% of nucleated cells). Diagnostic criteria Cytochemistry study and surface marker study confirm the lymphoid origin . Diagnostic criteria blood tests to count the number of each of the different kinds of blood cells.. If the results of the blood tests are not normal, a doctor may do a bone marrow biopsy . The chance of recovery (prognosis) depends on how the leukemia cells look under a microscope. V-25 Leukemic cells in acute lymphoblastic leukemia characterized by round or convoluted nuclei, high nuclear/cytoplasmic ratio and absence of cytoplasmic graulnes. Differential diagnosis AML. MDS. Non-Hodgkin‘s lymphoma with bone marrow involvement or with leukemic change. CLL. Differential diagnosis Viral infection with lymphocytosis CML with acute blastic crisis. Acute lymphoblastic leukemia Laboratory examinations Full blood count Coagulation screening – esp AML M3. Biochemical screening Chest radiography Bone marrow aspiration Immunophenotyping Cytogenetics & molecular studies Lumbar puncture ( CNS involvement) Complications Cerebral hemorrhage, pul. hemorrhage or other vital organ hemorrhage. Infection(sepsis or septic shock ) , pulmonary edema. Tumor lysis syndrome. Complications Infiltration syndrome(CNS, GI tract or gonads). Coagulopathy before or after chemotherapy. Anemia. Risk Grouping of TPOG (ALL) Standard Risk High Risk– CNS leukemia, cranial nerve palsy, testicular leukemia, pre-B ALL t(1;19) or E2A-PBX1 fusion Very High Risk WBC > 100000/mm3 T – cell < 1y/o Lymphoblastic lymphoma with bone marrow lymphoblasts > 25% t(9;22) or BCR-ABL fusion t(4;11) or MLL-AF4 fusion Other MLL gene rearrangement Hypodiploidy ( chr 44 or less) Poor Prognosis (I) Acute lymphoblastic leukemia Relapse Bone marrow– the most common site, blast cell increase CNS– IICP ( vomiting, headache, papilledema, lethargy) Convulsion Behavior disturbance Testis– painless swelling Survival rates 75 % to 80% of children with ALL survive at least 5 years from diagnosis with current treatments that incorporate systemic therapy (e.g., combination chemotherapy) and specific central nervous system (CNS) preventive therapy (i.e., intrathecal chemotherapy with or without cranial irradiation). Recurrent The most important extramedullary sites of relapse are the CNS and the testes. Treatment Chemotherapy – reach to remission (blast<5%) CNS prophylaxis Intrathecal C/T Cranial irradiation Bone marrow transplantation Management and treatment Hydration, prevention of hyperuricemia and tumor lysis syndrome. Antibiotics, may need the 3rd generation of cephalosporin or other strong antibiotics, even antifungal agents. Management and treatment Chemotherapy(include remission induction, consolidation & maintenance. CNS prophylaxis with chemotherapeutic agents(methotrexate 10~15mg, intrathecal injection). Management and treatment Blood transfusion(component therapy) Nutritional support Bone marrow transplantation Growth factor Treatment The primary treatment for ALL is chemotherapy. Radiation therapy may be used in certain cases Bone marrow transplantation is being studied in clinical trials. Treatment : Chemotherapy uses drugs to kill cancer cells drugs may be taken by mouth, or may be put into the body by a needle in a vein or muscle. All chemotherapy is stopped after two to three years of treatment . Treatment : Chemotherapy Prednisone: Used in induction and reinduction therapy and also given as intermittent pulses during continuation therapy. toxicity : fluid retention, increased appetite, transient diabetes, acne, striae, personality changes, peptic ulcer, immunosuppression, osteoporosis, growth retardation; caution in diabetes, fungal infections, and osteonecrosis Vincristine: toxicity : Peripheral neuropathy manifested by constipation, ileus, ptosis, vocal cord paralysis, jaw pain, abdominal pain, loss of deep tendon reflexes; reduce dosage with severe peripheral neuropathy; bone marrow depression; local ulceration with extravasation, SIADH Asparaginase local rash, hives, anaphylaxis; bone marrow depression, hyperglycemia, hepatotoxicity, and bleeding may occur. Daunorubicin Myelosuppression and thrombocytopenia; may cause cardiac arrhythmias immediately following administration and cardiomyopathy after long-term use; nausea, vomiting, stomatitis, and alopecia; extravasation may occur, resulting in severe tissue necrosis; caution with impaired hepatic, renal, or biliary function. Methotrexate (Folex PFS) Hematologic, renal, GI, pulmonary, and neurologic systems; discontinue if significant drop in blood counts; aspirin, NSAIDs, or low-dose steroids may be administered concomitantly with MTX (possibility of increased toxicity with NSAIDs, including salicylates, has not been tested) Radiation Therapy uses x-rays or other high-energy rays to kill cancer cells and shrink tumors. Treatmet for VHR Induction:(10 weeks) Prednisolone,Vincristine,Idarubicin, Asparaginase,cyclophosphamine,cytarabine, 6-MP,TIT. Consolidation:(8 weeks) 6-MP,MTX,TIT Reinduction:(7 weeks) Dexamethasone, ,Vincristine,Idarubicin, Asparaginase,cyclophosphamine,cytarabine, 6-MP,TIT. Bone Marrow Transplantation Hematopoietic stem cell transplantation is an option for very high-risk cases (e.g., Philadelphia chromosomepositive ALL) or those who develop an early relapse in the bone marrow. Bone Marrow Transplantation a newer type of treatment. high doses of chemotherapy with or without radiation therapy are given to destroy all of the bone marrow in the body. Healthy marrow is then taken from another person (a donor). autologous bone marrow transplant, is being studied in clinical trials. Treatment Induction : 4 weeks Hyhration. Allopurinol Vincristine iv qw & Prednisolone po qd L- asparaginase Mediastinum or spine tumor : R/T Treatment CNS prophylaxis Intrathecal ingestion : methotrexate Intrathecal ingestion : methotrexate , Ara-C, hydrocortisone High risk:Intrathecal ingestion C/T&R/T THANKS !