Boston Adult Congenital Heart Service Frontiers in Contraception
advertisement

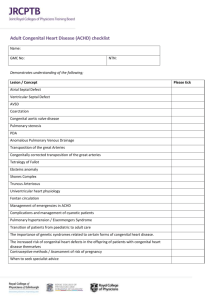
BACH and Transitioning: Preparing Adolescents with CHD for Self-Care in Adulthood Susan M. Fernandes, MPH / Michael J. Landzberg, MD Boston Adult Congenital Heart Service Children’s Hospital and BWH, Boston, MA 1/200 of us is born with congenital heart disease… A child is born in the US every 7.6 seconds… 1/10 extended families… 1 million ACHD survivors A child with CHD is born in the US every 26 minutes… 1789 Liberty Leading the People Eugene Delacroix 1830 (L’Hopital des Enfants-Malades 1802 ) These hearts are unique “Something the Lord Made” Alfred Blalock, Helen Taussig, and Vivien Thomas: 29 Nov 1944 CHD – Paradigm Shift • 40,000 infants born with CHD/ year • What is successful outcome? – Surviving initial surgical repair – Surviving to 1 year of age – Normal childhood – Normal adolescence Surviving to / through Adulthood “One Million Strong” US: 30-170 ACHD Centers to Fulfill Medical Needs and Care for ACHD Survivors Atresia d-TGA ACHD Population complex ••• Mitral CCTGA • Size makes a difference (ASD > 2 cm, VSD greater than 1 cm, PDA > 0.6-0.8 cm) • Simple ASD • Simple Aortic Disease • Simple Mitral Disease • Simple PDA • Mild VPS 60%: prior operations 50%: will have reops 3:1 interventions are CATH CHF, PAH, Arrhythmia 15% 47% 38% simple moderate Red font indicates some association with higher risk for development of PAH • • • • • • • DORV Heterotaxy Single V Conduits Truncus Cyanotic Eisenmenger • • • • • • • • • • • TOF SV Defects APV Drainage AVC Primum ASD Sub PS AoCo Ebstein VPS PR Complex PDA or VSD ACHD, adult congenital heart disease; ASD, atrial septal defect; PDA, patent ductus arteriosus; VPS, vascular positioning system; d-TGA, dextrotransposition of the great arteries; CCTGA, congenitally corrected transposition of the great arteries; DORV, double outlet right ventricle; TOF, tetralogy of Fallot; SV, stroke volume; APV, absent pulmonary valve; AVC, atrioventricular canal; PS, pulmonary stenosis; AoCo, aortic coarctation; PR, pulmonary valve regurgitation; VSD, ventricular septal defect; CATH, catheterizations. Marelli A et al. Am Heart J. 2009;157:1-8. Warnes C et al. J Am Coll Cardiol.. 2001;37:1170-1175. “One Million Strong” “One Million Frail” The ACHD Phenotype 1– – 0.9 – SCD-Free Survival (proportion) TOF COA – d-TGA 0.8 – AS n = 3589 – 0.7 – 0 5 10 15 20 25 30 Postoperative Interval (years) Silka et al. J Am Coll Cardiol . 1998; 32: 245-251. 35 ACHD “Medical Phenotype” Billett J et al. Heart. 2008, 1194-1199. BACH Original Cohort. 11 ACHD Cardiovascular “Phenotype” : MVO2 Mean ± SD Aortic coarction Tetralogy of Fallot VSD Mustard-operation Valvular disease Ebsteins anomaly Pulmonary atresia Fontan-operation ASD (late closure) ccTGA Complex anatomy Eisenmenger 28.7 ± 10.4 25.5 ± 9.1 23.4 ± 8.9 23.3 ± 7.4 22.7 ± 7.6 20.8 ± 4.2 20.1 ± 6.5 19.8 ± 5.8 19.2 ± 6.2 18.6 ± 6.9 14.6 ± 4.7 11.5 ± 3.6 ANOVA P<0.0001 5 10 15 20 25 30 35 40 Peak VO2 (ml s/b mL) MVO2 indicates Myocardial Oxygen Consumption; CCTGA, Congenitally Corrected Transposition of the Great Arteries; SD, Septal Defect; ANOVA, Analysis of the Variance; VO2, Volume of Oxygen Diller GP, et al. Circulation 2005, 828-835. 12 ACHD Arrhythmic “Phenotype” Atrial Arrhythmias (AA) in ACHD 20 year risk of AA: 15% (> 3x higher) AA in ACHD: > 50% mortal risk Bouchardy J, et al. Circulation 2009 Who is providing the care? • Many being seen by Pediatric Cardiologists NOT trained in ACHD • Many being seen by Adult Cardiologists NOT trained in ACHD • Few being seen in ACHD clinics (<5%) • In Reality: We Do Not Know! 15 ACHD Patients in USA vs Those in ACHD Clinics 787,000 Number Of Patients 800,000 – 700,000 – 600,000 – 500,000 – 400,000 – 300,000 – 200,000 – 100,000 – 0– 38,000 in ACHD Williams RG, et al. J Am Coll Cardiol. 2006;47(4):701-707. ACHA Clinic Directory Working Group 2007 16 Understanding Loss of CHD Follow-Up 650 – n=643 (100%) Attrition 177 (28%) 520 – CHD Patients n=643 (100%) 53 (8%) Attrition 123 (19%) 390 – 260 – Diagnosed by cardiologist 643 (100%) 130 – n=466 (72%) 51 (8%) Seen by cardiologist 413 (64%) Seen by cardiologist 292 (45%) 6-12 13-17 n=343 (53%) Attrition 94 (15%) Seen by cardiologist 249 (39%) 0– <6 18-22 Age Group The blue bars indicate patients who were not seen by a cardiologist within the indicated age range but were seen again by a cardiologist in an older age group (ie, transiently lost to follow-up). Adapted from: Mackie A, et al. Circulation. 2009;120:302-309. Finding the “Lost” Percent of Outpatients > 18yrs 35 30 25 20 15 10 5 0 2000 2001 2002 2003 2004 2005 2006 2007 35.00 30.00 25.00 20.00 15.00 10.00 5.00 <1y >18y 2005 2003 2001 % Echos by Age 1999 1997 1995 1993 1991 1989 1987 1985 1983 0.00 <1y CHB Transitioning Working Group • 30 clinicians throughout CHB representing all outpatient clinics • Numerous focus groups to identify key transitioning education areas that are common to a wide spectrum of pediatric diseases • Established Goals – 1). Assess the current state of preparing patients at CHB for self-care in adulthood. Current Practices for the Transition and Transfer of Patients with a Wide Spectrum of Pediatric-Onset Chronic Diseases (Fernandes et al. 2011 Int Journal of Adol and Child Health) • Single Center- CHB • Random sample of 479 outpatient clinicians • Overall response rate: 76.8% (368/479), 329/368 meet inclusion criteria – – – – 143 Physicians 157 Nurses/nurse practitioners 75 Social workers 26 Physician assistants Table 1. Clinician Characteristics (Fernandes et al. 2011 Int Journal of Adol and Child Health) Transitioning Education • 73% of clinicians stated their patients receive transitioning education – – – – 71% Physicians 75% Nurses/Nurse Practitioners 80% Physician Assistants 60% Social Workers • 92% provide transitioning education informally • 61% begin transitioning education before age 16 years (Fernandes et al. 2011 Int Journal of Adol and Child Health) Perceptions of Transitioning and Transfer: Results of a Survey of CHB Cardiology Clinicians • 31 Clinicians (16.9±9.7 years in practice) – 16 MD – 15 Nurses, NP’s, PA’s • All cardiology clinicians stated that their patients are provided with this education/assessment – 74.2% informally – 22.6% checklist – 13.0% unknown Patient and Parent Perceptions of Transitioning and Transfer @ CHB • Recruitment of 16-25 year old patients with pediatric onset disease likely to require life long medical care and their parents • 166 Patients • 104 Parents – 93 Matched Patient/Parent Patient and Parent Perceptions of Transitioning and Transfer in Cardiology @ CHB • 30 Patients CHB Cardiology – Mean age 19.5±3.0 years – 14 Complex – 6 Moderate – 1 simple – 2 HCM – 3 CVG clinic – 4 cardiac transplant Transitioning EducationResources • 90% of clinician’s support resources for the development of transitioning education programs • 73% of parents identified the need for such programs. Parental Knowledge of LLCCC • Multi-center study of 500 Parents – – – – S/p arterial switch operation (n=92) S/p tetralogy of Fallot repair (n=134) S/p Fontan procedure (n=140) S/p aortic coarctation repair (n=126) • 9 U.S. Centers • Pediatrics, 2011 Nov 28 (Epub) – 118 from CHB Key Findings ① The overwhelming majority of clinicians believe they are providing their patients with the necessary skills to become independent adults capable of self care, although informally. ① Patients and parents perceive such as severely lacking. ① Clinicians, patients and parents overwhelmingly support the need for resources to improve the delivery of this type of education. Acknowledgments Boston Adult Congenital Heart (BACH) Program