Evaluation and treatment of male and female pattern hair loss
advertisement

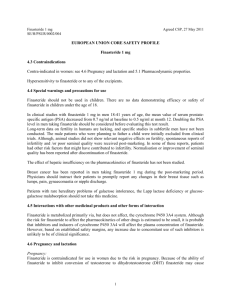
Dr Z. Shahmoradi Dermatologist Hair follicle: 5 million hair follicles on the human skin 100,000 on the scalp(plus eyelashes & eyebrows) Three types: lanugos, vellus, terminal Anagen: 90-95% of normal scalp hairs (3 yrs=1000 days) Catagen: 1-2% (3 weeks) Telogen: 5-10% (3 months=100 days) Alopecia: 1) Cicatricial: lichen planus, DLE, kerion, Favus, Morphea, Burning,…. 2) Non cicatricial: male pattern alopecia, alopecia areata, psoriasis, seborrheic dermatitis, …. Shedding in telogen effluvium. Non CA Androgenetic alopecia Alopecia areata Traction alopecia CA Synonyms Male pattern hair loss (MPHL) Male pattern baldness (MPB) Androgenetic alopecia (AGA) Common baldness Androgenetic alopecia -At least 80% of Caucasian men show some signs of AGA by age 70. Although testosterone is the major circulating androgen in men, the testosterone metabolite, DHT, plays a dominant role in AGA. In scalp biopsy: in men with MPHL: 5aR activity & DHT levels are increased AGA The conversion of T to DHT is catalyzed by 5aR DHT: temporal scalp hair recession, acne, growth of prostate, development of terminal hairs in the beard region, external ears, nostril & on the limbs. Type 1 5aR is widely expressed but its physiological function is uncertain (in sebaceous glands & liver) Type 2 5aR is expressed in androgen-dependent tissues such as the prostate & hair follicle (scalp, beard& chest) AGA MPHL is absent in men with genetic deficiency of type 2 5aR. Treatment with finasteride, a selective inhibitor of type 2 5aR, slows the progression of MPHL and produces some regrowth of hair in about 2/3 of men. The primary target of androgen action in the hair follicle: in dermal papilla & dermal sheath. AGA Genetic factors predispose to AGA, but their nature and the mode of inheritance is uncertain. Inheritance is most likely polygenic. There is increased frequency of AGA in sons of men with AGA. The maternal influence on AGA is less well defined. Women with FPHL are less likely than men to have a strong family history of the disorder Female pattern hair loss (FPHL) FPHL undoubtedly, but not necessarily, occurs in women with hyperandrogenism (MPHL, hirsutism and/or menstrual disturbance) FPHL with hyperandrogenism may respond to treatment with finasteride, or cyproteron acetate Most of women with FPHL show no other clinical or biochemical evidence of androgen excess. There was no response in postmenopausal women to treatment with finasteride or in women without signs of androgen excess to cyproteroterone acetate. Clinical finding In men Onset: may begin anytime post-puberty, usually by age 40. 14% in 15-17 yrs. Pattern: most common: bitemporal, frontal, mid scalp, vertex Uncommon: diffuse scalp hair loss or female pattern with diffuse central scalp hair thinning Hair pulling: may be positive in active early hair loss in the central scalp but generally negative in long-standing hair loss …MPHL Affected hair: miniaturization (finer, shorter) and decreased hair density Scalp: generally normal, concomitant seborrheic is common. If perifollicular erythema or hyperkeratoses = biopsy for R/O cicatricial alopecia Associated finding: high incidence coronary artery dis. (CAD), Hypertension, hypercholesterolemia. Family history: commonly positive but in 20%, not have a FH of MPHL. Clinical finding (women) Onset: may begin any time post menarche In central scalp +/-sides of scalp Pattern: A- diffuse central thinning of the crown with preservation of the frontal hair line B- frontal accentuation (Christmas tree) C- Fronto-temporal recession/vertex loss (male pattern) is uncommon. Bitemporal thinning is commonly associated with, but not necessarily indicative of FPHL. Pulling test : may be positive in active early loss in the central scalp, but generally negative in long-standing hairloss …FPHL Affected hair: miniaturization of hair Scalp: generally normal, seborrhea, R/O Cicatricial alopecia Associated finding: sign or symptoms of hyprndrogenism (hirsutism,severe acne, galactorrhea, infertility, irregular mense, A.Nigricance) Family history: FPHL are less likely than men with MPHL to have a history of first-degree relatives with MPHL. Evaluation R/O other cause of hair loss (iron def., acute & chronic telogen effluvium, Sisaipho,…) In men: anabolic steroids or supplemental androgens may worsen MPHL Consider check TSH if the hair loss is diffuse & not localized exclusively to typical MPHL Consider iron (in vegetarian or otherwise deficient diet,..) …Evaluation In hyperandrogenism, blood test should be include: 1 -free and/or total T +/- DHEAS at a minimum=done off of OCP (inhibit both ovarian & adrenal source of androgens). If these tests are normal on OCPs, but the suspicion is high for hyper A, they should be repeated at least one month after cessation of OCPs. 2 –if T is greater than 2.5x normal or >200ng/dl, or DHEAS is greater than 2x normal or >700 micro g/dl in pre or >400 in postmenopausal women, a work up for tumor with radiographic test. …Evaluation If galactohhhea or increased T or free T = check prolactin If T or DHEAS is elevate = screen for CAH. An early morning serum 17-OH progesterone during the follicular phase of the cycle (day 1-14) would be a reasonable screening test for the most common form of CAH, ie, 21hydroxylase def. If prolactin or 17-OH progesterone is increased = refer to endocrinologist. …Evaluation In women: screening blood work is generally recommended in all of women In otherwise healthy women, check TSH & serum ferritin R/O Iron def.:by serum ferritin or serum iron and TIBC. Low serum ferritin is diagnostic of iron def. depleted iron stores in patients with chronic dis. May not be detected by serum ferritin (ferritin is acute phase reactant and inflammatory disorders, malignancy, infections increase its synthesis) If check iron & TIBC: pts. Should not be taking iron preparations (multivitamin with iron or OCP with iron) for at least 24h …Evaluation Iron supplements taken for > 3 wk can falsely elevated ferritin levels in the face of iron def. Iron def. is associated with low serum iron & relatively high TIBC & low percent saturation. Other screening test may be indicated by history = CBC and/or T4 The majority of FPHL have no clinical or biochemical evidence of androgen excess. Specific investigations: Often non required Scalp biopsy Iron studies, serum electrolytes, Urea, Cr Thyroid function tests Androgen profile (if suspicious of virilization) Testosterone, DHT SHBG LH, FSH ANA Scalp photography Histopathology A- indication for biopsy: Diagnosis: Males: usually not necessary unless a FPHL, diffuse HL or scalp changes suggestive of scarring alopecia or prepubertal boy with a Ludwig PHL. -Females: sometimes necessary to exclude chronic T.E, diffuse AA or cicatricial hair loss Site of biopsy: central scalp (should not be from the bitemporal =miniaturized hair independent of MPHL or FPHL) A punch biopsy (not less than 4 mm), into the subcutaneous fat. Many dermatopathologists favor horizontal sectioning of biopsy. …histology The ratio of terminal to vellus or vellus-like hair normally is 7:1. in PHL , decrease to 2:1 The total number of hairs per unit area is usually normal in PHL (30-50 / 4mm punch), but reduced in severe baldness A perifollicular infiltrate, lymphohistiocytic Perifollicular fibrosis First line therapies: Topical minoxidil Finasteride Dutasteride Spironolactone Cyproteron acetate Camouflage A A C B B D Second line therapies: Scalp surgery or transplantation C Treatment Prevent further hair loss & if possible stimulate hair growth General: pts should avoid hair care products likely to damage scalp/hair. Pts should maintain an adequate diet (especially protein) Topical medications work only where the medication is applied If possible, any drugs that could negatively affect hair growth should be stopped. Treat any underlying scalp disorder (seborrhea, pso,..) Treatment (men) Finasteride 1mg/d & minoxidil 2-5% =FDA approved for men > 18 years old. 5% is a more rapid onset of action. Treatment should be used for 12 mo before making a decision about efficacy although benefit may be seen sooner. Finasteride : 2/3 decreased DHT in serum & scalp Efficacy: target area hair counts (TAHC): are circular target areas 1cm to 1 inch in diameter typically at the anterior leading edge of the vertex balding area where the terminal, non-vellus, or visible hairs are counted pre & post treatment. …Finasteride TAHC increase over the first year and peak by 12 mo. : in men age 18-41, hair counts increase 17/cm2 for those on 1 mg finasteride vs-4/cm2 for placebo. Hair growth continue to improve for at least the first 24 mo of treatment .in 18-41 yr, 50% of men showed an increase in hair growth by 1 yr, and 66% by 2 yr, compared to 7% & 7% by placebo (1 yr=10% increase) In 41-60 yr, 39% on finasteride versus 3% on placebo in 2 yr. (90% stop hair loss in men for at least 5 yrs, hair regrowth in 65%) Discontinue: any positive effect will be lost in 12 mo. superficial subcutis, variability in the caliber of hair follicles, with an increased number of miniaturized hairs, is apparent. Several fibrous streamers are also seen. ...Finasteride Safety: no known drug interaction, no effect on liver, BM, kidney,…, no effect on spermatogenesis Reversible sexually related side effects (decreased libido , erectile dysfunction, decreased ejaculate volume): in 2% versus 1% with placebo. In 41-60 yr : increased side effect in 8% vs 5% on placebo. Painful gynaecomastia (0.001%) This side effects often resolve during continued treatment or within days to wks after discontinued. The level of drug in semen is very low, and semen no risk to a pregnant women or her fetus. …Finasteride F. is teratogen. In male fetus : hypospadias with cleft prepuce, decreased anogenital distance, reduced prostate weight, altered nipple formation. F. has not effect on spermatogenesis or semen production No effect on bone density ...Finasteride • Reduction in PSA is based on the effect decreased DHT on the prostate. Recommendation is that any PSA test value should be doubled for any man taking finasteride to compensate for the effect of the drug. • (40% reduced PSA in 40-49 yrs & 50% in 50-59 yrs.) • Finasteride may selectively inhibit low grade prostate tumors (Gleason stage 2-6) ,25% reduce among men aged 55 and over. - low DHT may induce histologic changes that mimic high grade disease -low DHT may induce higher grade prostate cancers (Gleason stage 7-10) (5mg/d: high grade prostatic carcinoma in elderly men (or reduced?) ...Finasteride Finasteride & dutasteride are both teratogens with very long biological half-lives (activity may persist into second trimaster), but pharmacokinetic half-life is 8 h. Photography is useful for monitoring, but unlikely to detect changes of less than 20% in hair density. Max increase occur after 1 yr Further improvement : increase in hair length, diameter & pigmentation. Dutasteride D. is a combined type 1 & 2 5aR inhibitor. 0.5 mg/d a 53% reduction is scalp DHT and at 2.5 mg/d the reduction is 83%. Sexual side effects are more common but reversible. Minoxidil FDA approved for upper 18 yrs old (in adolescents) Mode of action: increases duration of anagen & enlarges miniaturized follicles(enlargement of shaft diameter) - K channel opener & vasodilator 1 ml twice daily, require 1h for absorption Best result in early case (<10 yrs), limited extend(<10 cm, on the vertex), hair density above 20 hairs/cm2) Efficacy: TAHC & photographs confirm a significant increase in hair density, hair growth appears to peak at 16 wk, 5% is superior to 2%, TAHC increases are 19/cm2 for 5% & 13/cm2 for 2% & 4/cm2 for placebo at 6 mo. …Minoxidil photography: 58% increased hair growth on 5% & 41% for 2% & 23% on placebo at 1 yrs. Conversion of vellus to terminal hair (30%), complete remission (10%) ..Minoxidil Discontinue: any positive effect will be lost in 4-6 mo. Initial telogen effluvium, begin 2-8 wk after treatment initiation ( result from release of telogen hair as anagen promotion begins), self limiting with continued treat. Safety: side effects are mainly dermatologic: scalp irritation, dryness, scaling, itching, redness (more common with 5%) -Allergic C.D: is uncommon (with minoxidil or PG) Combination therapy -Additive effect For switch from treatment with one of these agents to other should continue for at least 3 mo together. Treatment for women Women with or without hyperandrogenism: - no androgen therapy -FDA : only 2% minoxidil approved for women (60% arrested hair loss or mild to moderate hair growth) - treatment should be used for 12 mo before making a decision about efficacy although benefit may be seen sooner. - minoxidil in those women with FPHL both with or without hyperandrogenism, in young & old, in pre & postmenopausal women alike. ..Minoxidil Safety: either 2 or 5% appears safe to use in women with FPHL, with the only additional risk of the 5% for face hypertrichosis (3-5%). The hypertrichosis tends to occur over the cheeks & forehead as vellus, not terminal, hair and disappears within 4 mo. of stopping the drug. - hypertrichosis due to spreading to the face or may also be a result of hypersensitivity to low levels of systemic absorption. Women with hyperandrogenism <40% of women with FPHL have hyperandrogenism (androgen hypersensitivity or overproduction) Efficacy of this drugs in women with FPHL who do not have overt H.A have not specifically shown proven efficacy. Since all antiandrogens or 5aR inhibitors may cause feminization of the mal fetus, all women of childbearing = OCP. Spironolactone Act by blocking cytoplasmic receptors for DHT. Also weakly inhibits androgen biosynthesis. Spironolactone 100-300mg /d.(usually 200mg), check K at baseline & 1 mo after beginning treatment (hyperkalemia). Pts should keep well hydrated. Spironolactone 200mg/d or cyproterone acetate 100mg (days 5-15), will prevent further hair loss in up to 90% of women. Regrowth may be seen in up to 40% after 1-2 yr of treatment. Contraindication: in pregnancy: risk of feminization in male fetus & hypospadias. (In childbearing: OCP is choice) ..Spironolactone Side eff.: are dose related, mense irregularity, postmenopausal bleeding, breast tenderness or enlargement, fatigue Concomitant use of OCP: reduced side eff. Rare cases of hepatocellular carcinoma & hepatitis (with higher dose) Contraindication: in pregnancy: risk of feminization in male fetus & hypospadias. Finasteride 1-1.25 mg/d. not useful in post-menopausal with FPHL. Some positive reports in women with HA treated with 1.25 mg /d have emerged. There are no anticipated side effects and no blood tests are necessary. Cyproterone acetate Androgen receptor blocker, potent progestin, antigonadotrophic effect. May use for over 40 yr. For postmenopause, androcor with or without estrogens may be used continuously. 100 mg days 5-15 with Diane 5-26, appears most useful. Diane only , less effective in hair loss. Side eff.: wieght gain, breast tenderness, loss of libido, lassitude, depression, nausea, feminization of male fetus No specific blood tests are necessary. Flutamide A non-steroidal antiandrogen: inhibiting androgen uptake, inhibiting nuclear binding of andogen within the target tissue. In one study: F. is superior to androcor & finasteride Side eff.: rare but potentially fatal hepatotoxicity Low-level light therapy Most are packaged like a hairbrush or comb which shines red light directly on the scalp while it is used to comb through the hair. Only on such device, called the HairMax LaserComb, has obtained 510k FDA approval for use as a medical device Should be explain to patients: this device has safety rather than actual efficacy. Cosmetic aids & …. Not all treatment work for all people Tinted powders, lotions, hair sprays Shampoo ketoconazol,Sawpalmetto, palminex Vitamins, supplements? Wigs, hair pieces, Camouflages,… Hair transplantation