Pressure Ulcers in the Critically Ill Patient

Jamie Oelschlaeger, RN-BSN
MRICU, St. Luke’s Medical Center
Alverno College
MSN Program
Click here to get started!
To advance to the next slide, click
To return back to the main menu at any time, click
To view the previous slide, click
To view the last seen slide, click
Review questions will be located through out the tutorial.
To re-visit the material presented in the question, click the hyperlink located in the answer box located on the slide
Pathophysiology of Integumentary
By the end of this presentation, the learner will:
Identify and differentiate the different stages of pressure ulcers
Understand the difference between pressure ulcers, deep tissue injury, and unstageable ulcers
Identify risk factors associated with the development of pressure ulcers
Largest organ of human body
Protective function
Regulates temperature with in the body
Storage for water and fat
Prevents loss of water
Prevents bacterial invasion
The Ohio State University Medical Center (n.d.)
Image provided by Microsoft clipart
Skin is composed of 3 layers:
Epidermis
▪ Outer most layer
▪ Prevents bacteria from penetrating
▪ Prevents loss of water
Dermis
▪ Middle layer
▪ Contains blood vessels, sweat glands, and nerves
Subcutis
▪ Inner most layer
▪ Contains collagen and fat
▪ Regulates body temperature
The Ohio State University Medical Center (n.d.)
Picture used for education purposes from the National
Pressure Ulcer Advisory Panel (200&
The epidermis thins
Changes in connective tissue result in less elasticity and strength
Blood vessels in dermis become fragile
The subcutaneous layer thins
Reduced sensation of touch, pressure, temperature
U.S. National Library of Medicine (2011)
MedicineNet (2011)
Web MD (2011)
Picture provided by Microsoft clipart
Skin becomes vulnerable to injury
Thinning skin and loss of subcutaneous tissue decrease protection
Increased possibility of blood vessel rupture
U.S. National Library of Medicine (2011)
MedicineNet (2011)
Web MD (2011)
Picture provided by Microsoft clipart
The subcutaneous layer of the skin thins with aging.
True
Right on!
False
No! A normal part of aging in skin includes thinning of the subcutaneous layer of skin.
A pressure ulcer is an area of tissue damage that occurs when the skin and tissues are compressed between bones and a surface which has direct contact with the body
Occurs most frequently over a bony prominence
Classified into four stages based on appearance
The AGS Foundation for Health and Aging (2011)
National Pressure Ulcer Advisory Panel (2007)
Skin is intact
NON-BLANCHABLE redness present over in localized area over bony prominence
Affected area may be:
Painful
Firm
Warmer
National Pressure Ulcer Advisory Panel (2007)
Picture used for education purposes from the National
Pressure Ulcer Advisory Panel (2007)
Loss of partial thickness to dermis
Shallow or open area
Pink and red wound bed
Slough is not present
Affected area will be:
Shiny or dry
No slough or bruising
National Pressure Ulcer Advisory Panel (2007)
Picture used for educational purposes from the
National Pressure Ulcer Advisory Panel (2007)
Click the link below to view the pressure ulcer from
Arnold (2007)!
http://www.snjourney.com/I mages/pustage2.gif
Try again! This ulcer is not intact!
Good
Job!
Try Again! This ulcer does not penetrate beyond the dermis!
No! This ulcer is not purple/maroon in appearance!
I
II
IV
Deep Tissue Injury
Loss of partial thickness to dermis
Shallow or open area
Pink and red wound bed
Slough is not present
Affected area will be:
Shiny or dry
No slough or bruising
National Pressure Ulcer Advisory Panel (2007)
Picture used for educational purposes from the National
Pressure Ulcer Advisory Panel (2007)
Full thickness tissue loss
Exposed bone, tendons, and/or muscle
Slough or eschar may be present
Affected area may include:
Undermining
Tunneling
National Pressure Ulcer Advisory Panel (2007)
Picture used for educational purposes from the National
Pressure Ulcer Advisory Panel (2007)
Click the link below to view the pressure ulcer from the
University of Washington
(2011)!
http://msktc.washington.edu
/images/stage_3_Merck.jpg
Try again! This ulcer has more than just a open pink wound bed!
Perfect
Nice try! This ulcer does not expose tendon or bone!
Not this one! This ulcer does not have a necrotic wound bed
II
III
IV
Unstageable
Skin intact or blood-filled blister
Localized area purple or maroon in color
Underlying soft tissue affected
Affected area may be:
Painful
Firm
Boggy
Warmer
National Pressure Ulcer Advisory Panel (2007)
Used for educational purposes from the National Pressure
Ulcer Advisory Panel (2007)
Full thickness tissue loss
Base of ulcer covered by slough and/or eschar
Once slough and/or eschar is removed, the ulcer can be staged
National Pressure Ulcer Advisory Panel (2007)
Used for educational purposes from the National
Pressure Ulcer Advisory Panel (2007)
Click the link below to view the pressure ulcer from
Medscape (2011)!
http://img.medscape.com/pi
/emed/ckb/rehabilitation/305
143-317514-319284-
1714350.jpg
Try again! This ulcer does not have an open wound bed!
Not this one! This ulcer does not penetrate beyond the dermis!
Try again! This ulcer is not purplish in appearance!
Correct!
II
III
Deep Tissue Injury
Unstageable
Increased pressure, moisture, friction and shear damage underlying tissues of skin
Damaged tissue releases prostaglandins and leukotrienes
WBC collect to the site of injury
Vasodilation occurs at the site
Increased venule permeabilty occurs with in the venules
Porth (2005)
Picture provided by Microsoft clipart
Exudate leaks out of the venules and into the surrounding tissue
Decreased blood volume to site of injury
Tissues swell causing edema
Pressure on nerves cause pain
Pressure ulcers develop as a result
Inflammation is the first sign of pressure ulcer development!
Porth (2005)
Picture provided by Microsoft clipart
Inflammation does not play a role the development of pressure ulcers.
True
Try Again! The inflammatory response play a large role in pressure ulcer development
False
That is correct!
There is no genetic predisposition in developing pressure ulcers
Genetic disorders and diseases can increase risk of pressure ulcer development though:
Interference with healing
Increased fragility with in blood vessels and skin
Lack of sensation in limbs
Porth (2005)
Picture provided by Microsoft clipart
Diabetes is a genetic disease that can cause neuropathy over time and result in loss of sensation in limbs
Loss of sensation can lead to an inability to feel temperature and pressure increasing the risk of pressure ulcers to develop
Peripheral vascular disease is a genetic disorder that causes blood vessel constriction or occlusion decreasing blood flow to affected area
Loss of blood flow causes a decrease in oxygen and nutrients which leads to cell death and increase pressure ulcer risk
American Diabetes Association (2010)
Columbia University Medical Center Department of Surgery (2011)
Picture provided by Microsoft clipart
Cerebral Palsy and muscular dystrophy are examples of genetic disorders that cause physical disabilities which can result in paralysis of limbs
Paralysis leads to the inability to move limbs voluntarily
Lack of movement increases risk of pressure, friction, and shear on skin
Pressure ulcers can develop as a result
National Institute of Neurological Disorders and Stroke
(2010)
Porth (2005)
Picture provided by Microsoft clipart
Diabetes can cause neuropathy which results in loss of sensation, inability to sense temperature, and pressure.
True False
That is correct!
Try again! Neuropathy does result in loss of sensation, pressure, and temperature!
Under stress, the sympathetic nervous system responds
Epinephrine and norepinepherine are released into the blood stream and attach to receptor molecules on the surface of cells
Alpha 1 receptors cause decreased blood flow to skin
Sweating often occurs
Beta 1 receptors increase the metabolic rate
Fat stores release fat into blood stream
Porth (2005)
Picture provided by Microsoft clipart
Decreased blood flow to skin results in lack of nutrients and oxygen
Sweating increases moisture and risk of friction and shear
Release of fat into the blood stream may decrease protective layer for underlying tissues
Porth (2005)
Picture provided by Microsoft clipart
Sweating increases moisture and the risk of friction and shear.
True
Right on!
False
No! Sweating does cause additional moisture which increases friction and shear
Pressure on bony prominences restrict blood flow to vulnerable areas
Restricted blood flow decreases oxygen and nutrients
Cell death can occur at area if pressure is not relieved
Mayo Foundation for Medical Education and Research
(2011)
Porth (2005)
Elbows
Hips
Ankles
Shoulder blades
Back or side of the head
Rim of ears
Heels
Toes
Bridge of nose
Sacrum
Coccyx
Bedridden or wheelchair bound
Increased risk of pressure on bony prominences and decreased blood flow to vulnerable areas
Aging
The epidermis thins and blood vessels become more fragile
Fragile skin
Increased risk of shearing and tearing of skin
Urinary or bowel incontinence
Causes skin breakdown and increased moisture
Malnourishment
Lack of vitamins and nutrients prevent healing
Smoking
Nicotine reduces oxygen level in blood and impairs circulation
Mayo Foundation for Medical Education and Research (2011)
Porth (2005)
Picture provided by Microsoft clipart
Decreased mental awareness
Mental inability to shift weight to relieve pressure appropriately
Weight loss
Lower fat stores decreases protective layer for underlying tissue
Paralysis
Lack of limb movement increases risk of pressure on vulnerable areas
Vascular disease
Increased fragility of blood vessel rupture and decreased blood flow with in vessels
Diabetes
Loss of sensation from neuropathy and poor wound healing
Mayo Foundation for Medical Education and Research
(2011)
Porth (2005)
Picture provided by Microsoft clipart
High activity levels can result in the development of pressure ulcers.
False True
Correct!
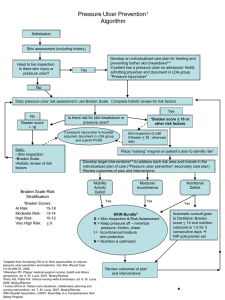
Turn bed bound patients every 2 hours
Encourage patients to shift weight in chair every 15 minutes
Repositioning relieves pressure on vulnerable bony prominences
Mayo Foundation for Medical Education and Research (2011)
U.S. National Library of Medicine (2010)
Picture provided by Microsoft clipart
Use pressure alleviating mattresses and pads
Use pillows or foam wedges to prevent contact with bony prominences
Mayo Foundation for Medical Education and Research (2011)
U.S. National Library of Medicine (2010)
Picture provided by Microsoft clipart
Apply moisture barriers and protective films to prevent moisture and skin breakdown
Apply protective, pressure alleviating dressings to open wounds
Mayo Foundation for Medical Education and Research (2011)
U.S. National Library of Medicine (2010)
Picture provided by Microsoft clipart
Encourage fluid intake to maintain skin integrity
Encourage a diet rich in protein, vitamins, and minerals to promote healing
Encourage daily exercise to increase blood flow to skin
Mayo Foundation for Medical Education and Research (2011)
U.S. National Library of Medicine (2010)
Picture provided by Microsoft clipart
Pressure alleviating mattresses are not helpful in pressure ulcer prevention.
True
No! Pressure alleviating mattresses play a key part in pressure ulcer prevention!
False
That is correct!
Mr. H, a 75 year old male, is admitted to the
ICU from the OR status post cholecystectomy.
His past medical history includes: diabetes, peripheral vascular disease, and currently smokes 2 packs per day.
Picture provided by Microsoft clipart
Mr. H experienced a number of complications during the case which extended his surgery to 8 hours. Because of his critical status, the physician ordered Mr. H to remain intubated overnight, NPO, and strict bed rest for the first 24 hours post-op.
Picture provided by Microsoft clipart
You are the nurse taking care of Mr. H 24 hours after his surgery. He remains on the ventilator and NPO but is off bed rest. You walk into the room to perform your assessment.
Picture provided by Microsoft clipart
As you are turning Mr. H onto his side, you notice an area on his coccyx that looks like this:
Click the link below to view the pressure ulcer from Medscape
(2011)!
http://img.medscape.com/article/715/969/715969-fig1.jpg
How would you describe the ulcer you assessed on Mr. H?
Skin Intact
Localized
Non-blanchable erythema
Skin Intact
Localized
Purple/Maroon appearance
Skin opened
Localized
Wound bed pink
Not this one! The ulcer does not have non-blanchable erythema
Perfect!
Try again! The ulcer is not open with a pick wound bed
Based on your assessment findings, how would you stage the ulcer?
I II
Deep Tissue
Injury
Not this one!
This is not a stage I
Try Again!
It is not a stage
II
Correct!
What risk factors make Mr. H more prone to developing pressure ulcers?
Smoking history
Good Job!
CPOD
Not a risk factor!
Diabetes
Yes!
PVD
Correct!
Pancreatitis
Not this one!
Bed ridden
Right On!
What nursing interventions could have been executed to prevent Mr. H from developing an injury?
Turning every
2 hours
Lying supine continuously
Using a pressure alleviating mattress
Applying moisture barrier cream
Correct!
Sorry! Lying in one position continuously is a common cause of pressure ulcers!
Perfect!
You got it!
AGS Foundation for Health in Aging, The. Pressure ulcers (bed sores). Retrieved February 2, 2011 from http://www.healthinaging.org/agingintheknow/chapters_ch_trial.asp?ch=30
American Diabetes Association. (2010). Genetics of diabetes. Retrieved April 5 , 2011 from http://www.diabetes.org/diabetes-basics/genetics-of-diabetes.html
Columbia University Medical Center Department of Surgery. Peripheral vascular disease: Cutting edge
therapies and studies at New-York Presbyterian hospital. Retrieved March 31, 2011 from http://www.columbiasurgery.org/news/healthpoints/2009_fall/p3.html
Long, M.A. (2007). New and improved: 2007 pressure ulcer definitions. Retrieved April 13, 2011 from
SNJourney Web Site: http://www.snjourney.com/ClinicalInfo/Systems/Intrgum/newstagepu.htm
Mayo Foundation for Medical Education and Research. (2011) Bed sores (pressure sores). Retrieved February
10, 2011 from http://www.mayoclinic.com/print/bedsores/DS00570/DSECTION=all&METHOD=print
MedicineNet. (2011). The effects of aging on your skin. Retrieved March 20 th 2011 from http://www.medicinenet.com/script/main/art.asp?articlekey=43078
Medscape. (2011). The Unavoidable Pressure Ulcer: Taking a Stand: Avoidable and Unavoidable Pressure
Ulcers. Retrieved April 13, 2011 from http://img.medscape.com/article/715/969/715969-fig1.jpg
Medscape. (2011). Pressure Ulcers, Nonsurgical Treatment and Principles. Retrieved April 13 th , 2011 from http://img.medscape.com/pi/emed/ckb/rehabilitation/305143-317514-319284-1714350.jpg
National Institute of Neurological Disorders and Stroke. (2010). NINDS cerebral palsy information page.
Retrieved March 15, 2011 from http://www.ninds.nih.gov/disorders/cerebral_palsy/cerebral_palsy.htm
National Institute of Neurological Disorders and Stroke. (2010). NINDS muscular dystrophy information
page. Retreived from http://www.ninds.nih.gov/disorders/md/md.htm
National Pressure Ulcer Advisory Panel. (2007). Pressure ulcer stages revised by NPUAP. Retrieved February
28, 2011 from http://www.npuap.org/pr2.htm
Ohio State University Medical Center. (n.d.) Anatomy of the skin. Retrieved March 23, 2011 from http://medicalcenter.osu.edu/patientcare/healthcare_services/skin_conditions/anatomy_skin/Pages/index.aspx
Porth, C.M. (2005). Pathophysiology.
University of Washington. (2011). Skin care and pressure sores. Retrieved April 13 , 2011 from http://msktc.washington.edu/images/stage_3_Merck.jpg
U.S. National Library of Medicine. (2010). Diabetic neuropathy. Retrieved March 5, 2011 from http://www.nlm.nih.gov/medlineplus/ency/article/000693.htm
U.S. National Library of Medicine. (2010). Pressure ulcer. Retrieved February 15, 2011 from http://www.nlm.nih.gov/medlineplus/ency/article/007071.htm
Web M.D. (2011). The effects of aging on skin. Retrieved March 22, 2011 from http://www.webmd.com/skin-beauty/guide/cosmetic-procedures-agingskin