Presentation - Healthcare Alliance
advertisement

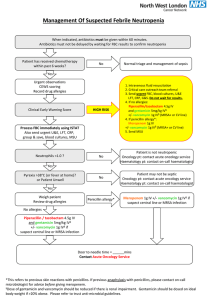
Outpatient and Inpatient MRSA: the New IDSA Guidelines Presented by Susan Kline, MD, MPH University of Minnesota Medical School Department of Medicine Division of Infectious Diseases Minneapolis , MN Presented to: Burnett Medical Center staff , Grantsburg, WI Jan. 19, 2012 Disclosure Slide I have served as a member of the Speakers Bureau and have received honoraria and research support from Pfizer Pharmaceuticals Objectives Review the new MRSA treatment guidelines Focus on adults Focus on common clinical conditions – Skin and soft tissue infections – Bacteremia and endocarditis – Pneumonia, community and hospital acquired 2011 Clinical Practice Guidelines by the Infectious Diseases Society of America: for the treatment of MRSA infections in Adults and Pediatrics Clinical Topics 1.Skin and soft tissue infections 2.Recurrent skin and soft tissue infections 3.MRSA bacteremia and endocarditis 4.MRSA pneumonia 5.MRSA bone and joint infections 6.MRSA central nervous system infections 7.Role of combination or adjunctive therapies 8.Vancomycin dosing and monitoring 9.Vancomycin susceptibility testing 10.Management of persistent bacteremia and vancomycin treatment failures 11.MRSA neonatal infections Clinical Infectious Diseases 2011:52;1-38. Evidence Grading System Strength of recommendation A Good evidence to support a recommendation for or against use B Moderate evidence to support a recommendation for or against use C Poor evidence to support a recommendation Quality of evidence I Evidence from >= 1 properly randomized, controlled trial II Evidence from >= 1 well-designed clinical trial, without randomization; from cohort or case-controlled analytic studies (preferably from > 1 center); from multiple time-series; or from dramatic results from uncontrolled experiments III Evidence from opinions of respected authorities; based on clinical experience, descriptive studies, or reports of expert committees. What is the management of skin and soft tissue infections (SSTIs) in the era of community associated MRSA (CA-MRSA) ? For cutaneous abscess incision and drainage (I &D) is the primary treatment (A-II) For simple abscess I &D alone should be adequate Additional data needed to determine role of antibiotics, if any Antibiotic therapy recommended In addition to I & D for – Severe abscesses – Multiple abscesses – Rapid progression with cellulitis – Signs or symptoms of systemic illness Send culture to guide antibiotic therapy if needed Antibiotic therapy recommended In addition to I & D for – Co-morbidities or immunosuppression – Extremes of age – Difficult to drain abscess site (face, hand, genital) – Septic phlebitis – Lack of response to I & D alone (A-III) For Outpatients with purulent cellulitis Send culture Empiric therapy for CA-MRSA 5-10+ days (follow patient response) Empiric therapy for Beta-hemolytic streptococcus likely not needed (A-II) For outpatients with non-purulent cellulitis (no purulent exudate, pus or abscess) Empiric therapy for beta hemolytic strep recommended Role of CA-MRSA unknown Add CA-MRSA coverage if – No response to strep treatment –or– Systemic toxicity Treat for 5-10+ days, need to follow patient response Treatment options for CA-MRSA outpatient empiric therapy Drug Adult Dose TMP-SMX 1-2 DS BID Doxycycline or Minocycline 100 BID Clindamycin 300-450 TID Linezolid 600 BID AII Evidence Grade AII AII AII For coverage for both beta hemolytic streptococcus and CA-MRSA Clindamycin alone (A-II) OR TMP/SMX or a tetracycline (doxy or mino) PLUS A beta-lactam (i.e.. amoxicillin, cephalexin, dicloxacillin ) (A-II) OR Linezolid alone (A-II) 32 y/o M with 3 days of an enlarging, painful lesion on his L thigh that he attributes to a “spider bite”. T 36.9 BP 118/70 P 82 What is the appropriate management of this patient? A. Incision and drainage alone B. Incision and drainage plus oral antiMRSA antimicrobial agent C. Oral anti-MRSA antimicrobial agent alone D. Therapy for Group A streptococcus alone Treatment of Complicated SSTIs hospitalized Deeper soft tissue infections Surgical/traumatic wound infection Major abscesses Cellulitis Infected ulcers/burn Surgical debridement Send cultures Start empiric therapy for MRSA Inpatient therapy for complicated SSTIs (empiric to cover MRSA) Vancomycin IV 15-20mg/kg/dose q 8-12 hours (A-I) Linezolid (IV / PO) 600mg q 12 hours (A-I) Daptomycin 4mg/kg IV q 24 hours (A-I) Televancin 10mg/kg IV q 24 hours (A-I) Clindamycin 600mg IV/PO TID (A-III) Inpatient therapy for non-purulent cellulits Could start a beta lactam alone (e.g. cefazolin) Then add MRSA coverage if no response (A-II) Length of therapy for inpatient SSTIs 7-14 days + of therapy Need to individualize based on patient response Usually start with IV and don’t switch to PO until the cellulitis is nearly resolved to prevent relapse, exception to rule is linezolid which has excellent oral absorption nearly 100% Management of recurrent MRSA SSTIs Emphasize good personnel hygiene, wound care and environmental cleaning – Regular bathing – Frequent hand washing, esp. if touch wound – Keep draining wound covered – Avoid sharing or reusing razors, linens, towels – Clean high touch surfaces with commercial cleaners Consider decolonization if Recurrent SSTI despite good wound care, hygiene and cleaning Ongoing household transmission Nasal mupirocin BID x 5-10 days +/Daily chlorhexidine gluconate baths/showers x 5-14 days Reserve oral antibiotics for active infections Use oral agent plus rifampin plus topical agents if have relapse despite doing all of the above What is the management of MRSA bacteremia and endocarditis? Uncomplicated bacteremia – No prosthesis, lines removed, fevers resolved in 72 hours, blood cultures negative after 2-4 days, no metastatic focus of infection – Endocarditis excluded Echocardiogram recommended, TEE>TTE Give antibiotics x at least 14 days – Vancomycin 15-20mg/kg IV q 12 hours (A-II) – Daptomycin 6mg/kg IV q 24 hours (A-I) Complicated MRSA bacteremia 4-6 weeks of antibiotics recommended – Vancomycin 15-20mg/kg IV q 12 hours – Daptomycin 6mg/kg IV q 24 hours – Some experts recommend high dose daptomycin 8-10mg/kg IV q 24 hours (B-III) Off label dosing MRSA endocarditis 6 weeks of antibiotics recommended – Vancomycin 15-20mg/kg IV q 12 hours – Daptomycin 6mg/kg IV q 24 hours – Some experts recommend high dose daptomycin 8-10mg/kg IV q 24 hours (B-III) Off label dosing Addition of gentamicin or rifampin not recommended for native valve endocarditis Prosthetic valve MRSA endocarditis treatment (B-II) Vancomycin IV 15-20mg/kg IV q 8-12 hours x 6 weeks Plus gentamicin 1mg/kg IV q 8 hours x 2 weeks Plus rifampin 300mg PO/IV q 8 hours X 6 weeks May need early valve replacement surgery Indications for surgery for MRSA endocarditis Large vegetations > 1 cm Occurrence of embolic events during 1st 2 weeks of therapy Severe valvular insufficiency Valve perforation or dehiscence Decompensated heart failure Perivalvular or myocardial abscess New heart block Persistent fevers or bacteremia Vancomycin dosing guidance For serious infections dose based actual weight 15-20mg/kg IV q 8-12 hours Trough goal is 15-20 microgram/ml Need to adjust dosing interval upward for decreased creatinine clearance 60 year old male presents with 4 days of fevers and chills T 38.5 BP 102/71 P 104 R 20 O2 sat 98% RA weight 100 kg Heart: 2/6 systolic murmur at apex Chest: CTAB Skin: no peripheral stigmata of endocarditis Labs: 15.5> 39 > 350 Cr 0.8 Started on IV vancomycin 1 gram every 12 hours HD #1 blood cx: 3/4 MRSA (vanco MIC 1) HD # 5 T 37.8 BP 138/70 P 113 R 16 O2 sat 96% RA Alert and interactive, no new physical exam findings Blood cx: 2/2 MRSA (vanco MIC 1) Vancomycin trough 7 microgm/mL 2 cm mitral valve vegetation on echocardiogram What changes to the patient’s antibiotics should be made? A. Add gentamicin to vancomycin B. Add rifampin to vancomycin C. Increase vancomycin dose to 1.5 gram IV Q12 hrs, target goal trough of 15-20 microgm/mL D. Discontinue vancomycin and start IV daptomycin 6 mg/kg Q24 hrs Treatment for health care associated MRSA pneumonia Vancomycin 15-20mg.kg IV q 8-12 hours (A-II) Linezolid 600mg PO/IV q 12 hours (A-II) Clindamycin 600mg PO/IV TID (B-III) – If strain susceptible 7-21 day course depends on severity/extent of infection Hospitalized patients with severe community acquired pneumonia (CAP) Start treatment for MRSA pending sputum gram stain and culture (AIII) Severe CAP defined as – ICU admit – Necrotizing or cavitary infiltrates – Empyema (also need drainage) 35 y/o F previously healthy with 4 days of fever, chills, myalgias, and cough. Now with increasing dyspnea and hemoptysis x 24 hrs T38.7 P120 BP96/60 R24 89%RA Moderate respiratory distress with coarse rhonchi WBC 15, Hct 44, Plt 425 Rapid flu: + influenza A Sputum gram stain/ cx: pending Intubated, admitted to ICU In addition to starting anti-influenza therapy, would you treat with antibiotics and if so which? A. None B. Ceftriaxone and azithromycin C. Vancomycin and ceftriaxone and azithromycin D. Linezolid and cefepime E. Daptomycin MRSA pneumonia Daptomycin should not be used for Rx of pneumonia, (inactivated by pulmonary surfactant) Empiric Rx for MRSA recommended for severe CAP (ICU admission, necrotizing or cavitary infiltrates, or empyema) Discontinue empiric Rx if cultures do not grow MRSA Questions/Discussion References: Clinical Practice Guidelines by the Infectious Disease Society of America for the Treatment of MethicillinResistant Staphylococcus aureus Infections in Adults and Children Panel Members / Authors Catherine Liu, MD Henry “Chip” Chambers, MD Arnold S. Bayer, MD Sara E. Cosgrove, MD Robert S. Daum, MD Scott K. Fridkin, MD Rachel J. Gorwitz, MD Sheldon L. Kaplan, MD A.W. Karchmer, MD Donald P. Levine, MD Barbara E. Murray, MD Michael J. Rybak, PharmD David A. Talan, MD SPGC Liaison Stan Deresinski, M.D. Published in: Clinical Infectious Diseases Feb. 1, 2011