MOLST Staff Education
advertisement

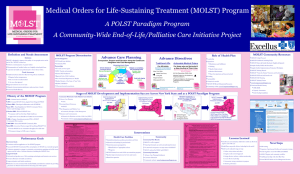
Medical Orders for Life-Sustaining Treatments MOLST Staff Education Patricia A. Bomba M.D., F.A.C.P. Vice President and Medical Director, Geriatrics Excellus BlueCross BlueShield A Community-wide End-of-life/Palliative Care Initiative project Objectives • Background • Oregon POLST • Rochester MOLST • Values, Goals, Expectations • Implementation & Education • Questions www.compassionandsupport.org Evolving Realities • Life expectancy has increased • Increased prevalence of chronic disease • Increased comorbidities and frailty with advancing age adding to complexity • Changing families, healthcare systems, society and marketplace demands • Death is “optional” Gaps and Quality Issues “Approaching Death: Improving Care at the End-of-Life” location of death pain management treatment preferences hospice admissions Institute of Medicine Report, 1997 Community-wide End-of-life/ Palliative Care Initiative Advance Care Planning – Community Conversations on Compassionate Care Honoring Preferences – Medical Orders for Life-Sustaining Treatment (MOLST) Pain Management and Palliative Care – Community Principles of Pain Management – CompassionNet Education and Communication – Education for Physicians on End-of-life Care (EPEC) – Community web site: www.compassionandsupport.org North Country Malone! Plat tsburgh Franklin Clinton ! Potsdam ! Watertown St. Lawrence Jefferson ! Watertown Lewis Central Genesee Niagara * * Western Buff al o ! Erie Chautauqua ** Cattaraugus ** * * Orleans Rochester ! Monroe Batavia ! Genesee Wyoming Liv ingston !Hornell Steuben Allegany Jamest own ! Yates Rome Oneida ! Seneca Auburn Cayuga Schuyler *** Chemung !Elmi ra Tioga Ut ica ! Herkimer Washington Fult on Amsterdam Montgomery ! Madison Tompkins Cort land Chenango Ithaca ! * Utica-Rome ** Syracuse ! Onondaga Wayne Hamilton Warren Oswego Ontario Essex * Binghamt on ! Broome Otsego Oneonta Saratoga Schenectady Rensselaer Al bany Albany Schoharie Columbia Greene Delaware Ulst er Southern Tier Tri-Cities Dutchess Sullivan Poughkeepsie Ro chester regio n Southern Tier reg ion * ACP/CCCC Putnam Westchester * MOLST Syracuse region Rockland Suffolk * CPPM Utica region Western reg io n Orange * EPEC Nassau North Country Malone! Plat tsburgh Franklin Clinton ! Watertown Potsdam ! St. Lawrence Jefferson ! Watertown Lewis Central Western Buff al o ! Erie Chautauqua * Cattaraugus Orleans Batavia ! Genesee Wyoming Rochester ! Monroe * Oswego Ontario Liv ingston !Hornell Steuben Allegany Syracuse ! Onondaga Wayne Yates ! Seneca Auburn Cayuga Schuyler Jamest own ! * Utica-Rome Rome Oneida Ut ica ! Herkimer Washington Fult on Amsterdam Montgomery ! Madison Tompkins Cort land Chenango Ithaca ! Chemung !Elmi ra Hamilton Warren Genesee Niagara Essex Tioga Binghamt on ! Broome Otsego Oneonta Saratoga Schenectady Rensselaer Al bany Albany Schoharie Greene Delaware Columbia Ulst er Southern Tier Tri-Cities Dutchess Sullivan Poughkeepsie Rochester region Southern Tier region Syracuse region Utica region Western region Orange Putnam Westchester * MOLST Rockland Suffolk Nassau Advance Care Planning: A Gift Clarify values, beliefs Choose a spokesperson Understand lifesustaining treatments Compassion and Support at the End of Life Practical issues Advance Care Directives For All Adults For Those Who Are Chronically Ill or Near the End of Their Lives Health Care Proxy Form Living Will Organ Donation (optional) Nonhospital Do Not Resuscitate (DNR) Order Medical Orders for Life Sustaining Treatment (MOLST) form POLST in Oregon • Taskforce formed in 1991 • Goal: ensure patient’s end-of-life care wishes are honored when patient is not able to speak for him or herself • Surrogate decision makers may communicate treatment preferences Philosophy of POLST • Individuals have the right to make their own health care decisions • These rights include: – Making decisions about life sustaining treatment – Describing desires for life sustaining treatment to health care providers – Comfort care while having wishes honored POLST in Oregon • Bright pink medical order form for seriously ill patients • Signed by MD, DO or NP • Turns patient preferences into orders • Goal: ensure wishes are honored POLST Research • Study of 180 nursing home residents – comfort measures only – do not resuscitate (DNR) order – transfer to hospital only if comfort measures fail Tolle, Tilden, Nelson, & Dunn (1998). A prospective study of the efficacy of the POLST, JAGS, 46: 1097 POLST Research • Findings – – – – no one received CPR, ICU care or vent 63% had orders for narcotics 2% hospitalized to extend their lives 13% overall hospitalized • Summary – POLST CPR orders respected – high comfort care – low rates of transfer for aggressive lifeprolonging treatments POLST : Research • Study of 58 older adults enrolled in a Program for All-Inclusive Care for the Elderly (PACE) • Reviewed POLST form and records from last two weeks of life Lee, Brummel-Smith, Meyer, Drew and London (JAGS 2000) POLST : Research • Findings – CPR use: consistent with directions for 91% of participants – Medication use: consistent for 46% of participants • 33% less invasive, 20% more invasive – Antibiotics given: consistent for 86% who had infections – Feeding tube use: consistent for 94%, IV fluids for 84% POLST : Research • Summary – effective in ensuring treatment wishes are honored about CPR, antibiotics, IV fluids and feeding tubes – less effective for medical interventions – more consistently followed than previously reported for advance directive forms Lee, Brummel-Smith, Meyer, Drew and London (JAGS 2000) POLST Outcomes: Completed ACD • 1993: 70% of Portland NH residents had DNR orders (Teno, et al) • 1996: 91% with written DNR orders in 8 Oregon NH’s (Tolle, et al) • 1997: 475 randomly selected Oregon decedents: – 67% with written AD – 93% family felt they knew wishes Site of Death “If dying patients want to retain some control over their dying process they must get out of the hospital they are in, and stay out of the hospital if they are out.” George Annas, Bioethicist POLST Outcomes: Site of Death Oregon residents who die in hospital • 1980: 50% • 1993: 35% (national average: 56%) • 1999: 31% (lowest rate in the US) Site of Death: National and State Data Deaths Deaths in a Deaths in at home Hospital a NH Oregon (Nat'l Benchmark) 35.10% 32.50% 32.40% National Mean (Average) 24.90% 50.00% 25.10% New York 21.20% 61.80% 17.00% POLST is Spreading Parts of: * * * * * * * * * * * Georgia, Kansas, Missouri, New Mexico, Utah, Washington, West Virginia, Wisconsin, New York, Pennsylvania From Oregon POLST to Rochester MOLST Medical Orders for Life-Sustaining Treatment MOLST • Created by the Communitywide End-of-Life/Palliative Care Initiative • Adapted from Oregon’s POLST form • Combines DNR, DNI, and other Life-Sustaining Treatments • Incorporates NYS law www.compassionandsupport.org MOLST vs. POLST POLST – Proprietary about exact form – Mainly researched in LTC – Did not fit many New York State criteria MOLST – Adapted to New York State law – Combines DNR, DNI and other Life-Sustaining Treatments – Meets all regulatory requirements Pink MOLST Form • Consistent color: easily identifiable – facilitate appropriate care desired by patient • Accuracy: clear, unambiguous medical orders • Flexible: changes can be made sequentially – Does not need to be done with each admission • Portable: transfer PINK across systems • Availability: Original PINK MOLST with the patient; make copy to retain in the chart Health Care Proxy/Living Will and MOLST Health Care Proxy/Living Will – completed ahead of time – applies only when decision-making capacity is lost MOLST – – – – applies right now not conditional on losing decision-making capacity set of physician orders may carry more weight in medical settings What Does MOLST Replace? • Replaces previous DNR/DNI forms • Old forms still valid • It does NOT replace NY State Health Care Proxy forms (or a living will) • Preferences for other life-sustaining therapies DNR Order State of New York Department of Health Nonhospital Order Not to Resuscitate (DNR Order) Person's Name:___________________________________ Date of Birth: _____/_____/_____ Do not resuscitate the person named above. Physician's Signature ____________________ Print Name _________________________ License Number ____________________ Date _____/_____/_____ It is the responsibility of the physician to determine, at least every 90 days, whether this order continues to be appropriate, and to indicate this by a note in the person's medical chart. The issuance of a new form is NOT required, and under the law this order should be considered valid unless it is known that it has been revoked. This order remains valid and must be followed, even if it has not been reviewed within the 90 day period. DOH-3474 (2/92) It Does NOT Replace the NYS Nonhospital Order Not to Resuscitate form (DNR Order) MOLST Values, Goals and Expectations Clarify Values and Beliefs • Every one has a personal sense of – who we are – what we like to do – control we like to have – goals for our lives – things we hope for Hope, Goals, Expectations • Hope, goals, expectations change with illness • Physician’s role to clarify goals, treatment plan • Members of the team’s role to support patient’s goals Potential Goals of Care • Cure of disease • Relief of suffering • Avoidance of premature • Quality of life death • Maintenance or improvement in function • Prolongation of life • Staying in control • A good death • Support for families and loved ones Multiple Goals of Care • Multiple goals often apply simultaneously • Goals are often contradictory • Goals are sometimes unrealistic • Certain goals may take priority over others Goals May Change • Some take precedence over others • Gradual shift in focus of care • Expected part of the continuum of medical care 7-Step Protocol 1. Create the right setting 2. Determine what the patient and family know 3. Explore what they are expecting or hoping for 7-Step Protocol 4. Suggest realistic goals 5. Respond empathetically 6. Make a plan and follow-through 7. Review and revise periodically Reviewing goals,treatment priorities • Goals guide care • Assess priorities to develop initial plan of care • Review with any change in – – – – health status advancing illness setting of care treatment preferences MOLST Implementation and Education MOLST: Who Should Have One? • Anyone choosing: – Do not resuscitate – Allow natural death • Anyone choosing to limit medical interventions • Anyone eligible/residing in LTC facility • Anyone who might die within the next year Pre-Hospital & Acute Care MOLST LTC Office MOLST • Implementation Issues – Development of policies and procedures – Integration of Policies and Procedures across the continuum of care – Discharge or Transfer – Accountability MOLST • Education – Staff • • • • Medical Hospital Long Term Care EMS – Community • Community Conversations on Compassionate Care MOLST Summary • Individuals have the right – – – – – – – make their own health care decisions patient-centered care focused on patient goals of care reflect patient values and beliefs discuss their preferences information is documented information is clear, unambiguous, flexible, portable, available, honored MOLST Summary • “Portable” medical order form • Travels with patient • Can translate an advance directive into physician’s orders • DOES NOT replace an advance care directive • DOES NOT replace the NYS Nonhospital Order Not to Resuscitate form (DNR Order) Resources • MOLST form, supplemental documentation, detailed MOLST review and FAQ’s are available as a copyrighted download-able PDF file at – www.compassionandsupport.org – pink forms available from Health Plan …fax reorder form to 585238-4400 MOLST Questions