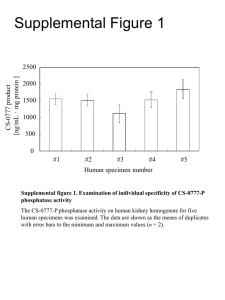
(i) C1 inhibitor concentrates
advertisement
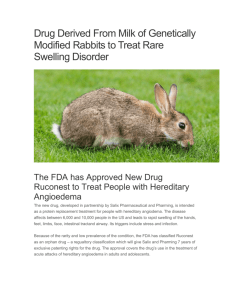
Authors: Allen P. Kaplan, USA Connie H. Katelaris, Australia Paul C. Potter, South Africa Timothy J. Craig, USA Updated: June 2011 Global Resources in Allergy (GLORIA™) Global Resources In Allergy (GLORIA™) is the flagship program of the World Allergy Organization (WAO). Its curriculum educates medical professionals worldwide through regional and national presentations. GLORIA modules are created from established guidelines and recommendations to address different aspects of allergy-related patient care. World Allergy Organization (WAO) The World Allergy Organization is an international coalition of 89 regional and national allergy and clinical immunology societies. WAO’s Mission WAO’s mission is to be a global resource and advocate in the field of allergy, advancing excellence in clinical care, education, research and training through a world-wide alliance of allergy and clinical immunology societies • First described by Quincke in 1882 • Well-demarcated non-pitting edema • Often caused by same pathological factors that cause urticaria • Reaction occurs deeper in dermis and subcutaneous tissues • Face, tongue, lips, eyelids most commonly affected • May cause life-threatening respiratory distress • • • • • • • • • Allergic: Foods, drugs, insect stings/bites Radiocontrast media NSAID and ASA Associated with anaphylaxis Autoimmune Idiopathic: – May be histamine induced or bradykinin induced ACE inhibitors Bradykinin-induced with normal C1-inhibitor (HAE-3) C1 inhibitor deficiency – Hereditary – Types I, II – Acquired • Physical causes – – – – – Cold Cholinergic Solar Vibratory Pressure • Other causes – Some contact reactions – Systemic diseases (e.g., systemic lupus erythematosis) • • • • Now most common exogenous cause of angioedema seen in emergency rooms Usually has no associated urticaria Due to increased bradykinin levels because kinin degradation is inhibited Can cause dramatic swelling of tongue, pharynx, or larynx – may require intubation or tracheostomy acutely • Angioedema develops in 0.1% to 0.5% of those receiving the drug • Onset from 1st week of use to 2-3 years of use • Symptoms resolve with cessation of drug, but may persist days • Described with all ACE inhibitors • Genetic factors may be important • Subjects with a history of angioedema from other causes are more susceptible to ACE-induced angioedema • Face, lips and tongue most commonly involved but laryngeal edema reported • Risk factors include obesity, prior endotracheal intubation and face and neck surgery • ACE inhibitors will trigger attacks in those with HAE, so avoid in these patients Bradykinin = Arg Pro Pro Gly Phe Ser Pro Phe Arg ACE Arg Pro Pro Gly Phe Ser Pro Phe Arg Bradykinin Arg Pro Pro Gly Phe Ser Pro + Phe-Arg ACE Carboxypeptidase N Arg Pro Pro Gly Phe + Ser Pro + Phe Arg Arg Pro Pro Gly Phe Ser Pro Phe + Arg Arg Pro Pro Gly Phe + Ser Pro Phe ACE Management • Stop drug and use other classes of antihypertensive agents • ALL ACE inhibitors are to be avoided • Management of angioedema depends on site of involvement – securing the airway by intubation may be necessary • ARB receptor antagonists are generally considered to be safe • Consider off label use of icatibant or ecallantide to treat swelling Johnson SP, Jacobsen J, Monster TBM et al. Am. J.Med.118:1428-1429, 2005 • 1888 – family described by William Osler • 1963 – Donaldson and Evans described the biochemical defect responsible – absence of C1 inhibitor • Defective gene located on chromosome 11 Epidemiology • 1:10,000 – 1:50,000 with no racial or gender predilection Clinical Presentations • • • • • Usually manifests in 2nd decade May be seen in young children Edema may develop in one or several organs Presentation depends upon site of swelling Attacks last 2-5 days before spontaneous resolution Nzeako Arch Intern Med, 2001 • Angioedema may develop in subcutaneous tissues of extremities, genitalia, face, trunk • Gastrointestinal tract and upper airway are also potential targets • Symptoms of bowel wall edema can be confused with an acute abdominal emergency – White blood count may be normal or abnormal and symptoms resolve within 72 hours without therapy • Submucosal edema of larynx (or, rarely, pharynx) may cause asphyxiation – this may occur on first presentation Laryngeal Edema Commonest cause of mortality in HAE • Time from onset of swelling to death 1-14 hours (mean 7 hours) • May be presenting feature • Death may occur in those with no previous laryngeal edema episodes • Increased risk within certain families • Early symptoms: lump in throat, tightness in throat • Hoarseness, inspiratory stridor, progressive dyspnoea • Hereditary – Autosomal dominant – 85% decreased C1 inhibitor - often gene deletion, insertion, stop codon, frame-shift mutation (Type 1 HAE) in the SERPIN Gene on Chromosome 11 (p11.2q13) – 15 % normal or increased C1 inhibitor protein but decreased function typically due to single nucleotide mutation (Type 2 HAE) – Suppression of the one normal gene product (theoretically should be 50%) to 35% or less causes swelling Zuraw. WAO Journal. Sept 2010 • • • • • Autosomal dominant; all patients heterozygous Each child of affected patient has a 50% chance of having HAE 20% no prior family history – spontaneous mutations More than 150 different mutations reported Varied clinical pattern may be explained by variable effect of mutations on C1 inhibitor synthesis and secretion as well as differences in Bradykinin metabolism Clinical presentation is key • For screening – C4 is cost effective and is low during attacks and in most people between attacks • Quantitative and functional assays of C1 inhibitor are usually indicated • C2 levels reduced in acute attack • • C1 should be normal No role for CH-50 Lunn M, Allergy and Asthma Proceedings 2010 C1 Inhibitor • Single chain glycoprotein; 478 amino acids molecular weight 104,000; serine protease family (SERPIN) • Important regulatory protein of complement cascade • Inactivates C1 esterase complex • Regulates coagulation, fibrinolytic, kinin, complement systems Nielson Immunopharmacology 1996 • Lack of C1 inhibitor leads to abnormal activation of complement pathway, reduced C2 and C4 levels • Hageman factor induces formation of kallikrein from prekallikrein • Bradykinin is released from high molecular weight kininogen • Bradykinin binds to the bradykinin receptor resulting in a marked increase in micro vascular permeability to cause angioedema Kaplan JACI 2002 Trace factor XIIa Prekallikrein HK Factor XII Factor XIIa surface surface HK HMW Kininogen (HK) Kallikrein Bradykinin Factor XI Factor XIa Factor XII Intrinsic Coagulation HK Factor XIIa Factor XIIf Autodigestion Kallikrein C1 Inhibited by CĪ INH CĪ C4 & C2 Digestion • • • • • • • • No response to steroids or antihistamines Avoid oral contraceptives, ACE inhibitor medications Pre-medicate before procedures including those requiring radiocontrast media or streptokinase as they may decrease C1 inhibitor levels Reassurance; address issues such as ongoing stress Treat infections promptly Genetic counseling and screening Hepatitis B vaccine in anticipation of receiving blood products Influenza vaccine Bowen, Allergy Asthma and Clinical Immunlogy 2010 Principles • Action plan for acute episodes • Strategy for long term prophylaxis • Short term prophylaxis for high risk procedures (e.g. dental work using C1 inhibitor concentrate 20 units /kg right before procedure) • Regular follow up for education and monitoring side effects of therapy Bowen, Allergy Asthma and Clinical Immunlogy 2010 Acute Attacks A (i) C1 inhibitor concentrates (a) Berinert 20 units/kg intravenous infusion (FDA approved 2009) (b) Cinryze 1000 units/patient (not FDA approved) (ii) Rhucin (50-100 units/kg) A recombinant C1 esterase inhibitor protein (not FDA approved) • Excellent and prompt response in most patients • Most patients respond well within 2 hours of infusion Craig, JACI 2009 • The earlier the patient is treated in an attack with C1 inhibitor the more rapid is the resolution • Home therapy for trained patients using C1 esterase inhibitor concentrate is a safe method for dealing with attacks of angioedema particularly where access to emergency care is difficult Bowen 2010 B Bradykinin Receptor Antagonism - - - Icatibant is a synthetic decapeptide functioning as a potent, selective competitive antagonist of the bradykinin 2 receptor Given by subcutaneous injection 3ml (30mg), half life 1-2 hours Approved in Europe, Australia and Brazil (and approval in USA imminent) Rapid onset usually within an hour, systemic side effects rare and local side effects at site of injection are common but transient Cicardi, NEJM 2010 C Kallikrein Inhibition - Ecallantide Approved by FDA (Dec 2009) for acute attacks 60 amino acid with high affinity to kallikrein Subcutaneous injection 30mg (three10mg injections) Significant clinical improvement reported within 4 hours of injection 2.7% risk of anaphylaxis within 60 minutes (good response to medical treatment in all reported cases) 12% develop anti-ecallantide antibodies including antiecallantide IgG and IgE, but IgG does not neutralize effect Cicardi, NEJM 2010 • Acute attacks when C1 inhibitor concentrate, ecallantide or icatibant are not available: – Intubation and respiratory support may be necessary when laryngeal edema present – Fresh frozen plasma (FFP) has been used successfully for acute attacks. Exacerbation of symptoms by supplying more kallikrein substrate is a consideration and is occasionally seen Prematta, Annals of Allergy Asthma and Immunology 2008 Long Term Prophylaxis – Adults • 20% of patients have attacks sufficiently frequent or severe that prophylaxis is needed using attenuated androgens (danazol, stanozolol, oxandrin) • C1 inhibitor concentrate, e.g. Cinryze, 1000 units intravenously twice a week with 50% reduction of attacks may be used in those unable to tolerate androgens • May substitute Berinert, but it is not approved for this indication • Higher doses of C1-INH may be necessary * Zuraw NEJM 2010 • • When using androgens titrate to lowest effective dose to control attacks – for danazol it may be possible to reduce to 200 mg every second day, and in some patients to 50 mg every second day Use the lowest effective dose, to reduce side effects Regular monitoring of liver enzymes • Serum lipid levels • – Blood pressure – Weight • Ultrasound of the liver annually may detect early hepatic adenomas and has been recommended Craig, Proceedings of Allergy and Asthma 2007 Long Term - Children • Anti-fibrinolytic agents, e.g. tranexamic acid and aminocaproic acid have been used as first line prophylaxis, but the latter is poorly tolerated • Low dose danazol in selected patients • C1-inhibtor dosed by weight 20 units per kg (Berinert) is off label indication for children • For adolescents 1000 units twice a week is approved (Cinryze) Nzeako, Arch Intern Med 2001 Short Term Prophylaxis Minor Manipulations Major Procedures or Intubation If plasma-derived C1 inhibitor (pdC1INH) immediately available: -No prophylaxis needed Plasma-derived C1 inhibitor (pdC1INH): -Give one to six hours before procedure* (optimum dose not yet established – see text). -Second dose of pdC1INH should be immediately available If pdC1INH not available: -Prophylaxis for five days before and two to 5 days post event -Danazol (avoid during fist two trimesters of pregnancy; 2.5-10 mg/kg/day, maximum 600 mg daily) -Stanozolol 4-6 mg/day Bowen T, Brosz J, Brosz K, Herbert J, Ritchie B. Management of hereditary angioedema 2010: Canadian approach. Allergy Asthma Clinical Immunology, 2010; 6: 20 If pdC1INH not available: -Danazol prophylaxis as per minor and Solvent/detergent treated plasma (SDP; if not available, then fresh frozen/frozen plasma but less safe than SDP) one to six hours before procedure* -10 ml/kg; 2-4 units (400-800 ml) for an adult *as close to procedure as feasible Pregnancy • Avoid attenuated androgens • Concentrates of C1 esterase inhibitor should be available and used to treat attacks • In severe cases chronic use of C1-INH twice a week at doses 1000 to 1500 units IV • FFP can be used with caution for attacks Bowen T, Brosz J, Brosz K, Herbert J, Ritchie B. Management of hereditary angioedema 2010: Canadian approach. Allergy Asthma Clinical Immunology, 2010; 6: 20 • Newer management strategies aim to address pathogenesis more specifically • Medications are being developed to decrease adverse reactions (for example, avoiding viral contamination of blood products by using recombinant products) • Oral bradykinin antagonist is being studied • Depot subcutaneous C1-INH is being developed to eliminate need for IV infusion Frank M. WAO Journal, 2010 Recombinant C1 inhibitor for the treatment of hereditary angioedema. • Type I: Seen most commonly with B cell lymphoma or monoclonal gammopathy. Rare cases may occur with autoimmune disorders with B cell hyperreactivity • Type II: Most commonly due to IgG antibody to C1 inhibitor which prevents its ability to inactivate enzymes such as plasma kallikrein and factor Xlla. The monoclonal proteins are antibody directed to C1 inhibitor There is an overlap in the two types, since most cases with lymphoma also have anti-C1 INH Cicardi, Publication pending • Decreased C1q levels distinguish AAE from HAE (C1q should be normal in HAE): C1 q is low in about 70% of those with acquired C1 INH deficiency and is very helpful but not totally reliable in distinguishing between HAE and acquired forms • Treatment of underlying condition may result in resolution • For acute attacks, C1 inhibitor concentrate, where available, should be used, but may require very large doses secondary to high titer of anti-C1-INH Cicardi, publication pending • Attenuated androgens, antifibrinolytics and/or immunosuppression therapy • Plasmaphoresis may be effective • Icatibant and ecallantide are also expected to be effective • Main treatment is treating the associated lymphoma Cicardi, publication pending C4 C1 INH Concentration C1 INH Functional Activity C1Q Type I Low Low Low Normal Type II Low Normal Low Normal Type III Normal Normal Normal Normal Low Low Low Low AAE Acquired C1 INH deficiency - Type I Acquired C1 INH deficiency - Type II C1-INH Function <30% <30% C1-INH Antigen Low Low C1Q Low Low C4 Low Low Absent Present* C1-INH Antibody Type II acquired C1 inhibitor deficiency (IgG C1 inhibitor) has a decrease in C1 inhibitor size on SDS gel electrophoresis from 105 Kd to 95 Kd *Bouillet L. Diagnosis and therapy of HAE. Jerini Satellite Symposium Proceedings XXVI EAACI, Goteborg, 2007 • Recurrent angioedema, no recognized exogenous precipitant, normal C4 levels, may or may not be associated with urticaria • Typically: episodes of swelling of lips, cheeks, eyes, tongue, pharynx, extremities, genitalia • Sub-types: – Respond to antihistamines – Non-responsive to antihistamines. Possible role of bradykinin? • Normal Complement – C1, C4, C1 inhibitor protein and function • Negative testing for antibody to IgE receptor • Anti-thyroid antibodies elevated in some; perhaps less frequently than in chronic urticaria • No obvious cause on history or exam • May not respond to antihistamines or corticosteroids if secondary to bradykinin • Non-sedating antihistamines (e.g. fexofenadine, desloratadine, cetirizine, loratidine) – up to 4 times the doses used for allergic rhinitis • Diphenhydramine 50 mg (for more severe attacks) – repeat in 4 hours • Prednisone 50 mg x 2 doses and stop without any taper • Epinephrine – if rapidly advancing • H2 antihistamines and leukotriene modifiers can be added • • • • • • • A non-sedating antihistamine; possible to use up to 4 times the usual dose for allergic rhinitis Add H2-antagonist high dose BID May try leukotriene modifier If ineffective, diphenhydramine or hydroxizine at 50 mg QID If antihistamines alone are ineffective, try corticosteroids Rarely, corticosteroid sparing agents such as cyclosporine may be tried Avoid known triggers Zuberbier T, Asero R, Bindslev-Jensen C. Allergy, 2009; 64: 1427-1443 • • • • Most often occurs in association with urticaria When angioedema occurs alone, consider idiopathic angioedema, ACE inhibitors, hereditary and acquired C1 inhibitor deficiencies HAE is a rare disease, but must be identified as it can be life-threatening New treatments for attacks of HAE, e.g. purified inhibitor, bradykinin antagonists and kallikrein inhibitor offer quick resolution of angioedema • Prophylaxis for HAE is also effective • ACE-inhibitor induced angioedema is an important cause of angioedema and is treated with avoidance • Acute cases of ACE-inhibitor induced angioedema may respond to icatibant or ecallantide • Patients with acquired angioedema should be referred to the appropriate specialist for ongoing management For more information on the World Allergy Organization (WAO), please visit www.worldallery.org or contact the: WAO Secretariat 555 East Wells Street, Suite 1100 Milwaukee, WI 53202 United States Tel: +1 414 276 1791 Fax: +1 414 276 3349 Email: info@worldallergy.org