2011 IDSA Pediatric Pneumonia Guidelines
advertisement
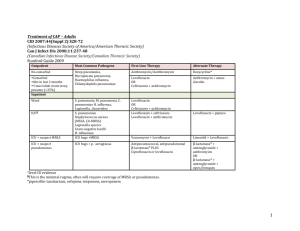
Management of Community Acquired Pneumonia in Infants and Children Older than 3 Months of Age Daniel Urschel, MD, Charles Pace, MD, Sherman Alter, MD Department of Pediatrics, Boonshoft School of Medicine, Wright State University, The Children’s Medical Center of Dayton Clin Infect Dis 2011; 53 (7): 617-630 Objectives 1. List common pathogens causing community-acquired pneumonia (CAP) in infants and children. 2. Discuss appropriate use of diagnostic laboratory and imaging tests in a child with CAP in an outpatient or inpatient setting. 3. Review choice of anti-infective therapy and duration of treatment provided to a child with suspected CAP in the outpatient or inpatient setting. “Teasers are docile male horses, usually old and past prime with undesirable genes, who set up aggressive just off-the-track mares to be bred by the wild testosterone crazed prize stallions whose only job is to deliver the goods, which they do. “ A 3yr old female presents to your office in November with cough and tachypnea. You hear crackles in left lower lobe and minimal retractions. She is alert, talkative, has had good fluid intake. Previously healthy and immunizations up to date. You believe 33% 33% 33% patient may be well enough to manage as an outpatient. Which diagnostic tests should be performed on this patient? 1. 2. 3. 4. 5. Complete blood count Chest radiograph Pulse oximetry Blood culture All of the above 0% 1 0% 2 3 4 5 A 3yr old female presents to your office in November with cough and tachypnea. You hear crackles in left lower lobe and minimal retractions. She is alert, talkative, has had good fluid intake. Previously healthy and immunizations up to date. You believe 33% 33% 33% patient may be well enough to manage as an outpatient. Which diagnostic tests should be performed on this patient? 1. 2. 3. 4. 5. Complete blood count Chest radiograph Pulse oximetry Blood culture All of the above 0% 1 0% 2 3 4 5 A school aged child hospitalized with community-acquired pneumonia can be safely discharged if he meets which of the following criteria? 1. 2. 3. 4. 5. Able to tolerate outpatient meds, greater level of activity, improving appetite. Afebrile for over 24 hours Pulse oximetry measurements >90% in room air at least 12 hours A and C A, B, and C 67% 33% 0% 1 2 3 0% 0% 4 5 Previously healthy 2 yr old diagnosed with pneumonia (faint crackles in the right base) in late October. Respiratory rate is 30 breaths/minute and temperature is 38.5° C. She has received all recommended immunizations. She attends a day care on daily basis. She is interactive and drinking well. Which oral anti-infective therapy should be provided 33% 33% 33% to this child managed as an outpatient? 1. 2. 3. 4. 5. A second-or third-generation cephalosporin (e.g., cefdinir, cefixime) for 10 days. Amoxicillin 90mg/kg/day divided 2 times a day for 10 days Azithromycin 10 mg/kg on day 1, 5 mg/kg on days 2-5 Combined treatment with both amoxicilln and azithromycin as noted above No anti-infective therapy indicated 0% 1 2 0% 3 4 5 A fully-immunized 6 yr old boy is hospitalized at Dayton Children’s. Radiography demonstrates left lower lobe consolidation without an effusion. He has a 92% SpO2 on 30% FiO2, some retractions and poor oral fluid intake. A blood culture is obtained. What first-line 67% antibiotic therapy is recommended? 1. 2. 3. 4. 5. A third-generation parenteral cephalosporin (e.g., cefotaxime or ceftriaxone) Intravenous clindamycin A third-generation parenteral cephalosporin plus azithromycin Intravenous ampicillin Intravenous vancomycin 33% 0% 1 2 3 0% 0% 4 5 A 5 yr old is admitted with a right upper lobe pneumonia. Child is not fully immunized. His blood cultures yield Streptococcus pneumoniae. Susceptibility testing on the blood isolate demonstrates a penicillin MIC of > 4 ug/mL. Appropriate 100% antibiotic therapy directed at this pathogen consists of: 1. 2. 3. 4. 5. Ceftriaxone intravenously at 100mg/kg/day Levofloxacin intravenously at 20 mg/kg/day Ampicillin intravenously at 400 mg/kg/day A or C A, B, or C 0% 1 0% 2 3 0% 0% 4 5 Introduction The Pediatric Infectious Diseases Society (PIDS) and the Infectious Diseases Society of America (IDSA) convened multiple subspecialists and expert consultants to create and review guidelines Guidelines endorsed by AAP, American College of Emergency Physicians, Society of Critical Care Medicine…. The guidelines grade method of recommendation, low or very low evidence situations require clinical judgment Strength of Recommendations Strength of Recommendations Inpatient Criteria Age 3-6 months with a suspicion of bacterial pneumonia Suspicion or documentation of methicillinresistant Staphylococcus aureus (MRSA) pneumonia Concern for follow up or administration of home therapy Patients Requiring Hospitalization Diagnostic approach to the child with pneumonia Outpatient Diagnostics Chest radiography, blood culture, CBC, ESR/CRP not necessary Pulse oximetry should be obtained in all patients If available a rapid test for influenza and for other viral pathogens should be obtained Testing for Mycoplasma pneumoniae should be obtained if suspicious If no improvement on antibiotics for 48-72 hrs, a CXR and blood culture should be obtained Inpatient Workup All pt’s should have CXR Blood culture CBC ESR/CRP Urinary antigen for Pneumococcal infection is not recommended Sputum samples if able (weak; low evidence) Rapid tests for Influenza and viruses should be used Mycoplasma pneumoniae should be tested for if suspicious No reliable test for Chlamydophila pneumoniae Inpatient Diagnostics A routine repeat CXR is not necessary Repeat CXR should be obtained if no clinical improvement is demonstrated by 48-72 hrs If blood culture yields MRSA, a repeat culture is mandatory todocument sterility of the blood. If blood culture is positive for another organism, repeat culture of blood is not mandatory Tracheal aspirate should be obtained in patient with endotracheal intubation Criteria for admission to an ICU Criteria for admission to an ICU Criteria for admission to an ICU Intubation, continuous CPAP or BIPAP Sustained tachycardia or hypotension <92% SpO2 on >50% FiO2 Altered mental status Clinical judgment should be used regardless of scores Discharge Criteria Improved Clinical Status >12 hrs RA with Sp02 >90% >12 hrs No increased work of breathing , tachypnea or tachycardia Able to tolerate outpatient therapy Chest tube out for >12 hrs Outpatient Treatment of Pneumonia Antibiotics not routinely required for preschool-aged children High-dose amoxicillin should be considered first line for presumed bacterial pneumonia in all ages 90 mg/kg/day divided bid TID dosing is required for Pen-resistant pneumococcus (MIC > 2 µg/mL) Macrolides (azithromycin) should be considered in school-aged and adolescents with illness consistent with atypical pneumonia Atypical Gradual onset Malaise, headache, sore throat, ear infections Lower fevers (101-102) Usually nonproductive, persistent cough May or may not have rales vs. Bacterial Gradual or acute onset Fatigue, dyspnea, chest pain Fevers often higher (>103) Cough more often productive Decreased or bronchial breath sounds, rales, dullness to percussion, egophony Manifestations of Mycoplasma pneumonia Outpatient Treatment of Pneumonia For presumed atypical pneumonia, azithromycin is first-line 10 mg/kg on day 1; 5 mg/kg on days 2-5 In season, treat influenza presumptively until a sensitive test is negative 10-day course of antibiotics is usually adequate Azithromycin: 5 day course MRSA will require a longer course (and hospitalization!) Inpatient Treatment of Pneumonia For the fully immunized child in regions that do not demonstrate high-level pneumococcal penicillin resistance: Ampicillin or Penicillin G are first-line Azithromycin for suspected atypical pneumonia (with a beta-lactam if diagnosis is in question) Vancomycin or clindamycin should be added when S. aureus is suspected by labs, clinical findings or imaging Ceftriaxone or cefotaxime are alternatives Inpatient Treatment of Pneumonia For a not fully immunized child or in regions that demonstrate high-level pneumococcal penicillin resistance: Ceftriaxone or cefotaxime is preferred Add azithromycin if considering atypical pneumonia Add vancomycin or clindamycin for S. aureus Ceftriaxone or cefotaxime also preferred for lifethreatening infections and empyema Empiric Inpatient Treatment of CAP Pneumococcal Penicillin Resistance MIC < 0.06 µg/mL: very susceptible MIC 0.12-1 µg/mL: susceptible High-dose oral amoxicillin >90% effective MIC 2-4: resistant High-dose oral amoxicillin effective MIC 1-2: somewhat resistant Standard-dose oral amoxicillin effective Oral therapy likely to fail; IV ampicillin or penicillin MIC >4: very resistant Standard-dose ampicillin likely to fail; ceftriaxone effective Specific Treatment for CAP Specific Treatment of CAP Specific Treatment of CAP Specific Treatment of CAP Specific Treatment of CAP Viral Pneumonia in Children Guidelines suggest not treating a preschool-aged child with suspected viral pneumonia (except influenza) Hamano-Hasegawa, J Infect Chemother (2008) Younger children more likely to have viral pneumonia Evidence of bacterial co-infection in 33% Michelow, Pediatrics (2004) Bacterial co-infections seen in 54% of viral pneumonias 67% of influenza pneumonia 55% of RSV pneumonia Michelow IC, et al. “Epidemiology and clinical characteristics of community-acquired pneumonia in hospitalized children.” Pediatrics. 2004 Apr;113(4):701-7. Michelow IC, et al. “Epidemiology and clinical characteristics of community-acquired pneumonia in hospitalized children.” Pediatrics. 2004 Apr;113(4):701-7. Viral Pneumonia in Children A 2010 retrospective cohort study of 4015 pediatric patients hospitalized with pneumonia 27% developed influenza-associated pneumonia Of these, 2% had a bacterial co-infection 18 identified by blood cultures; 3 by pleural fluid The actual incidence of secondary bacterial pneumonia with influenza is likely much higher Dagwood FS et al. “Influenza-Associated Pneumonia in Children Hospitalized With Laboratory-Confirmed Influenza, 2003-2008.” Pediatr Infect Dis J. 2010 Jul;29(7):585-90. Adjunctive Therapy CXR should be obtained if suspicious for effusion US or CT if CXR is inconclusive Size of effusion and respiratory compromise will determine treatment Pleural Fluid Tests Gram stain (+25-50%) Antigen or PCR if available (S. pneumoniae, S.aureus) Pleural fluid analysis rarely changes management and is not recommended WBC count with differntial helps differentiate source Majority of cultures will be negative Effusion/Empyema Total antibiotic therapy 2-4 weeks or 10 days after resolution of fever If abscess or necrosis is identified tx should begin with IV antibiotics If abscess is peripheral may attempt to drain, most will resolve spontaneously with IV antibiotics Abscess secondary to congenital malformation requires surgery consultation Necrosis should not routinely be managed surgically given high rates of broncho-pleural fistulas A 3yr old female presents to your office in November with cough and tachypnea. You hear crackles in left lower lobe and minimal retractions. She is alert, talkative, has had good fluid intake. Previously healthy and immunizations up to date. You believe 33% 33% 33% patient may be well enough to manage as an outpatient. Which diagnostic tests should be performed on this patient? 1. 2. 3. 4. 5. Complete blood count Chest radiograph Pulse oximetry Blood culture All of the above 0% 1 0% 2 3 4 5 A school aged child hospitalized with community-acquired pneumonia can be safely discharged if he meets which of the following criteria? 1. 2. 3. 4. 5. Able to tolerate outpatient meds, greater level of activity, improving appetite. Afebrile for over 24 hours Pulse oximetry measurements >90% in room air at least 12 hours A and C A, B, and C 100% 0% 1 0% 2 3 0% 0% 4 5 Previously healthy 2 yr old diagnosed with pneumonia (faint crackles in the right base) in late October. Respiratory rate is 30 breaths/minute and temperature is 38.5° C. She has received all recommended immunizations. She attends a day care on daily basis. She is interactive and drinking well. Which oral anti-infective therapy should be provided 67% to this child managed as an outpatient? 1. 2. 3. 4. 5. A second-or third-generation cephalosporin (e.g., cefdinir, cefixime) for 10 days. Amoxicillin 90mg/kg/day divided 2 times a day for 10 days Azithromycin 10 mg/kg on day 1, 5 mg/kg on days 2-5 Combined treatment with both amoxicilln and azithromycin as noted above No anti-infective therapy indicated 33% 0% 1 0% 2 3 0% 4 5 Previously healthy 2 yr old diagnosed with pneumonia (faint crackles in the right base) in late October. Respiratory rate is 30 breaths/minute and temperature is 38.5° C. She has received all recommended immunizations. She attends a day care on daily basis. She is interactive and drinking well. Which oral anti-infective therapy should be provided 67% to this child managed as an outpatient? 1. 2. 3. 4. 5. A second-or third-generation cephalosporin (e.g., cefdinir, cefixime) for 10 days. Amoxicillin 90mg/kg/day divided 2 times a day for 10 days Azithromycin 10 mg/kg on day 1, 5 mg/kg on days 2-5 Combined treatment with both amoxicilln and azithromycin as noted above No anti-infective therapy indicated 33% 0% 1 0% 2 0% 3 4 5 A 5 yr old is admitted with a right upper lobe pneumonia. Child is not fully immunized. His blood cultures yield Streptococcus pneumoniae. Susceptibility testing on the blood isolate demonstrates a penicillin MIC of > 4 ug/mL. Appropriate antibiotic therapy 33% 33% directed at this pathogen consists of: 33% 1. 2. 3. 4. 5. Ceftriaxone intravenously at 100mg/kg/day Levofloxacin intravenously at 20 mg/kg/day Ampicillin intravenously at 400 mg/kg/day A or C A, B, or C 0% 1 0% 2 3 4 5 BMJ 2003; 327:1459-1461