708-El-Sayed-_b
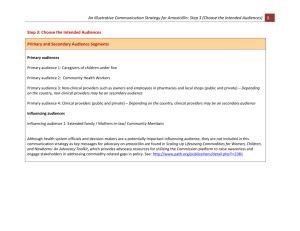
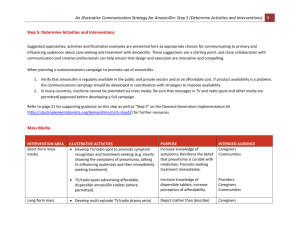
advertisement

Assessment of the Effectiveness and Safety of Outpatient Treatment of Severe Pneumonia Among Egyptian Children with Oral Amoxicillin (MASS Study - Egypt Chapter) Third International Conference for Improving Use of Medicines “ICIUM 2011” Antalya, Turkey, November 14-18th, 2011 Hesham El-Sayed, Narendra Arora, & Ahmed El-Gohary Faculty of Medicine Suez Canal University, Egypt Study Rationale Two million children <5Y die each year from ARI. ARI are the major cause of OP and Emergency Department visits and hospital admissions. Standard ARI case management [IMCI] recommends hospitalization of patients with sever pneumonia (chest indrawing & rapid breathing). APPIS study reported equivalent response of pneumonia patients to oral amoxicillin compared to injectable penicillin (Addo-Uobo et al, 2004). Pharmacokinetics study showed that amoxicillin twice daily is feasible alternative to thrice-daily dosing & recommended by American Academy of Pediatrics (Fonseca et al, 2003) 2 Study Objectives To assess the effectiveness and safety of home-based, 5-day treatment with oral amoxicillin, for curing severe pneumonia in children To identify baseline clinical predictors of treatment failure in children with severe pneumonia 3 Study Area & Population Ismailia governorate, Egypt, with population of one million inhabitants Seven primary health care centers Children presenting to the outpatient clinics of participating centers Other study sites: (Bangladesh, Ghana, and Vietnam) 4 Ismailia Inclusion Criteria 1. 2. 3. 4. Children aged 3 to 59 months. Patients suffering from Severe pneumonia, defined as lower chest indrawing (LCI) with cough and/or difficult breathing. Patients who are able to drink and do not have central cyanosis, regardless of the respiratory rate. Informed consent by a legal guardian 5 Exclusion Criteria (a) Very severe pneumonia/disease (central cyanosis, abnormally sleepy or difficult to wake, inability to drink, or convulsions) Known prior episodes of asthma or three or more prior episodes of wheezing LCI that resolves after three doses of bronchodilator therapy Severe malnutrition (visible severe wasting or edema) Known anaphylactic reaction to penicillin or amoxicillin 6 Exclusion Criteria (b) 6. Hospitalization in the last two weeks 7. Other diseases requiring antibiotic therapy at presentation (e.g., meningitis, dysentery, osteomyelitis, evident tuberculosis, etc.) 8. Persistent vomiting (vomiting three repeated doses of oral amoxicillin within ½ hour of administration). 9. Previous inclusion in the study or already included in another study 10. Living outside the pre-defined study area 7 Study Design A single-arm, cohort prospective intervention study 8 Baseline Assessment Demographic data History of the present illness ◦ The use of antibiotics ◦ The use of bronchodilators ◦ Immunization status ◦ Breast-feeding Physical examination that included: ◦ Respiratory rate ◦ Lower chest indrawing. ◦ Auscultatory wheezing, crackles (unilateral or bilateral), bronchial breathing, diminished or absent breath sounds. Urine Antibacterial Activity 9 Ambulatory Management Assessing eligibility for enrollment in the study Amoxicillin provided as suspension in a total dose of 80-90mg/kg per day for 5 days in 12 hourly doses The first dose administered by the caretaker under supervision in the health facility No other antibiotics were allowed while the child enrolled in the study Study patients who require additional antibiotics subsequent to enrollment, were declared treatment failures and withdrawn from the study, but follow-up of these patients continued until resolution of the morbid episode. 10 INTERVENTIONS Patient assessment data were collected on standard data collection forms at enrollment and Day 14 in the health centers by physicians, and at days 1,2,3,6 at home by trained nurse. Collected data included clinical assessment, adherence to therapy and adverse events occurrence. If the patient was well on Day 14, the patient was deemed cured and no further follow-up was done. Children who did not show up for their clinic appointment on Day 14 were actively traced for evaluation at home. If the patient is unwell at any time during the 14 days the patient was managed according to the standard clinic or hospital practices. 11 Study Outcome (a) Clinical deterioration occurring at any time after enrollment. 1. (Developing any sign of very severe disease such as central cyanosis, abnormally sleepy or difficult to wake, inability to drink, convulsions, or death) Inability to take oral medication due to persistent vomiting. 2. (Vomiting three repeated doses of oral amoxicillin within ½ hour of administration) Change or addition of antibiotics due to: 3. • • • Developing a co-morbid condition. Persistence of fever > 38oC with lower chest indrawing on day 3 (after 72 hours). Either Fever or lower chest indrawing alone at day 6. 12 Study Outcome (b) 4. Hospitalization related to pneumonia or therapy with amoxicillin. 5. Serious adverse event considered possibly or probably related to amoxicillin 6. Loss to follow up 7. Treatment failure between day 6 and 14 (relapse) 8.Voluntary withdrawal of consent from the study 13 STUDY RESULTS 14 Study Results The study included 237 children (3-59 mo.) Mean age of recruited children (12.42+10.05) months. Over 95% of children adhered to the treatment Clinical Cure rate with 5 days Amoxicillin therapy at Day 6 was 90.7%. Relapses occurred in 3.4% of the patients at Day 14, with Clinical Cure rate of 87.3% Loss to follow up of 3 patients (1.3%), 3 hospitalizations (1.3%) and no deaths Adverse events occurred in 14 children (5.9%) in the form of mild diarrhea and/or vomiting 15 Failure Rate of Treated Patients 16 Comparison of Baseline Characteristics of Cured vs. failed Treated Patients at Day 6 Characteristic Cured at Day 6 Failure at Day 6 -Age (months) 12.81+10.45 13.73+6.34 -Weight (Kg.) 9.47+4.86 7.86+2.33 * -Length (Cm.) 71.26+10.91 67.88+10.79 -Temperature © 37.56+1.34 37.66+0.51 -Respiratory rate 49.62+9.99 58.98+8.74 * (per minute) * Statistically Significant Difference (P <0.05) 17 Comparison of Clinical Baseline Characteristics of Cured vs. failed Treated Patients at Day 6 Clinical Finding Cured at Day 6 Failure at Day 6 - Fever Cough Difficult breathing Vomiting Diarrhea 74.9% 96.7% 62.3% 15.3% 5.6% 63.3% 95.5% 63.6% 13.6% 9.1% N.B.: No statistical difference between the two groups 18 Conclusions Oral amoxicillin is effective and safe in treating pneumonia in children in ambulatory setting, when given for 5 days in a dose of 80-90 mg/kg/day in 2 divided doses. Minor adverse effects occurred in small proportion of treated patients and did not affect cure rate. Failure of therapy occurred more frequently in patients of low weight and in those with rapid respiratory rate (>50/minute) at recruitment. 19 Potential Study Limitations It is an observational study, which did not have control arm to compare outcomes, however we compared our findings with prior studies conducted with similar protocols. We must be cautious in treating these children as they do need to be monitored for clinical deterioration through follow-up visits. We could only test 42% of patients’ urine for antibacterial activity that decreased our power to assess the effect that prior antibiotic use had on treatment failure The multicenter study did not include any area with high HIV prevalence or any sites from Latin America, where the population characteristics or disease ecology may differ from the included study sites, which may effect generalizability of our results. 20 Mutlicenter Study Strengths Large sample size provided good precision to our estimates of treatment failure rates The diversity of geographic settings, study implementation staff and prevalence of co-morbid conditions demonstrates that home-based therapy is applicable to a variety of public health settings Over 95% of children adhered to the treatment, while fewer than 5% of subjects were lost to follow-up. There were no deaths, and none had a serious adverse event related to study drug The study findings have important policy and programmatic implications for the treatment of pneumonia by reducing hospital referrals and admissions, which will reduce health care costs and hospital-acquired infections Acknowledgement The study was supported by grant from INCLEN Inc., USAID, Johns Hopkins University & WHO Technical support 22