File - Respiratory Therapy Files
advertisement
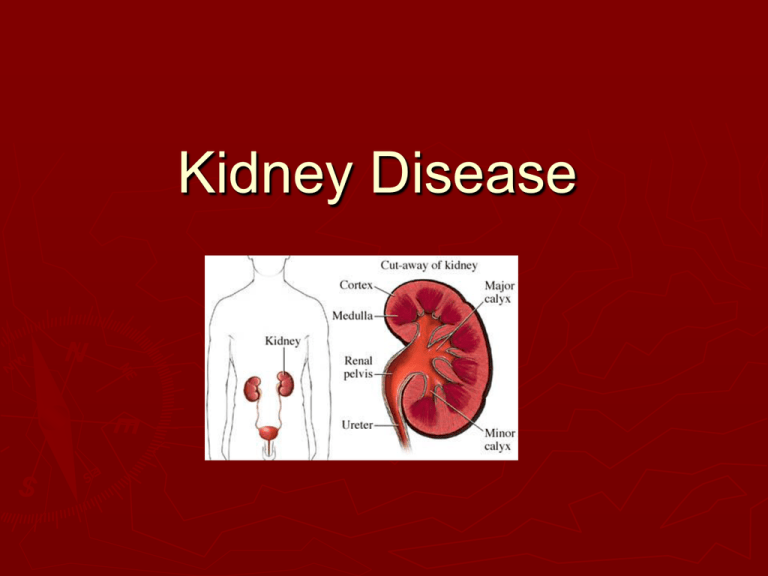
Kidney Disease Terminology CRF: Chronic Renal Failure ARF: Acute Renal Failure ESRD: End stage renal disease ESRF: End stage renal failure GFR: Glomular filtration rate Azotemia: Retention of nitrogenous waste products as renal insufficiency develops The Kidney Three of the biggest jobs that the kidneys have are: (1) to cleanse the blood, (2) to regulate and maintain an appropriate fluid and chemical balance in the body, and (3) to produce the urine. Each of these functions is closely related to the other two, not only because each involves the removal or addition of fluid and chemicals from the blood, but also because each of these functions takes place in the kidney's nephrons. The starting point in the nephron for each of these functions is the glomerulus. It is the "gateway" that the blood must pass through in order to be cleansed by the kidneys. The Kidney There are 1 million nephrons in each kindey The kidney has an innate ability to maintain GFR by hyperinfiltration and compensatory hypertophy of the remaining healthy nephrons Acute Renal Failure is a rapidly progressive loss of renal function, generally characterized by oliguria (decreased urine production, quantified as less than 400 mL per day in adults, less than 0.5 mL/kg/h in children or less than 1 mL/kg/h in infants); and fluid and electrolyte imbalance. AKI can result from a variety of causes, generally classified as prerenal, intrinsic, and postrenal. An underlying cause must be identified and treated to arrest the progress, and dialysis may be necessary to bridge the time gap required for treating these fundamental causes Causes of ARF Prerenal causes of AKI are those that decrease effective blood flow to the kidney. These include systemic causes, such as low blood volume, low blood pressure, and heart failure, as well as local changes to the blood vessels supplying the kidney (clots, stenosis…) Sources of damage to the kidney itself are dubbed intrinsic. Intrinsic can be due to damage to the glomeruli, renal tubules, or interstitium. Common causes of each are glomerulonephritis, acute tubular necrosis (ATN), and acute interstitial nephritis (AIN), respectively Postrenal is a consequence of urinary tract obstruction. This may be related to benign prostatic hyperplasia, kidney stones, obstructed urinary catheter, bladder stone, bladder, ureteral or renal malignancy Chronic Renal Failure The most common causes of CKD are diabetes mellitus, hypertension, and glomerulonephritis.Together, these cause approximately 75% of all adult cases http://www.youtube.com/watch?v=ikGl7DPX UK0&feature=related Chronic Renal Failure Presence of markers of kidney damage for three months, as defined by structural or functional abnormalities of the kidney with or without decreased GFR, manifest by either pathological abnormalities or other markers of kidney damage, including abnormalities in the composition of blood or urine, or abnormalities in imaging tests. The presence of GFR <60 mL/min/1.73 m2 for three months, with or without other signs of kidney damage as described above. Am J Kidney Dis 2002; 39:S1 Diabetes A group of metabolic diseases in which a person has high blood sugar, either because the body does not produce enough insulin, or because cells do not respond to the insulin that is produced. This high blood sugar produces the classical symptoms of polyuria (frequent urination), polydipsia (increased thirst) and polyphagia (increased hunger). There are three main types of diabetes: Type 1 diabetes: results from the body's failure to produce insulin, and presently requires the person to inject insulin. Type 2 diabetes: results from insulin resistance, a condition in which cells fail to use insulin properly, sometimes combined with an absolute insulin deficiency. Gestational diabetes: is when pregnant women, who have never had diabetes before, have a high blood glucose level during pregnancy. It may precede development of type 2 DM. GFR Volume of fluid filtered from the renal glomerular capillaries into the Bowman's capsule per unit time. Glomerular filtration rate (GFR) can be calculated by measuring any chemical that has a steady level in the blood, and is freely filtered but neither reabsorbed nor secreted by the kidneys. The rate therefore measured is the quantity of the substance in the urine that originated from a calculable volume of blood The GFR test measures how well your kidneys are filtering a waste called creatinine, which is produced by the muscles. When the kidneys aren't working as well as they should, creatinine builds up in the blood. Stages of CKD Stage 1*: GFR >= 90 mL/min/1.73 m2 Normal or elevated GFR Stage 2*: GFR 60-89 (mild) Stage 3: GFR 30-59 (moderate) Stage 4: GFR 15-29 (severe; pre-HD) Stage 5: GFR < 15 (kidney failure) Am J Kidney Dis 2002; 39 (S2): S1-246 Epidemiology 19 million Americans have CKD Approx 435,000 have ESRD/HD Annual mortality rate for ESRD: 24% Am J Kidney Dis 2002; 39(S2): S1-246 Signs & Symptoms General Fatigue & malaise Edema Anorexia Nausea/vomiting Dysgeusia Ophthalmologic AV nicking HTN Heart failure Hyperkalemia Pericarditis CAD Skin Pruritis Pallor Cardiac GI Neurological MS changes Seizures Uremia Is the clinical and laboratory syndrome, reflecting dysfunction of all organ systems as a result of untreated or undertreated acute or chronic renal failure Changes in the blood The kidneys work to filter toxins and waste products out of the blood. When kidney function declines, waste products begin to build up within the blood. Creatine and urea build up. Phosphate also accumulates in the blood. A build up of hydrogen ions may also occur, leading to acidosis. Changes in electrolytes Because of the resulting changes to the blood chemistry, the electrolyte balance of the blood and cells is disrupted. Fluid retention also results. Often fluid retention is the first noticeable sign that the kidneys are beginning to shut down. The resulting water weight gain and edema in the hands and feet signal that the kidneys are not removing waste products and fluids as they should. Pulmonary Edema as acute renal failure worsens, fluids continue to build within the body and may begin to collect in the air sacs of the lungs. This condition, known as pulmonary edema, can result in difficulty breathing, restlessness, anxiety and wheezing. Untreated pulmonary edema can ultimately lead to respiratory failure. Most deaths that occur in cases of renal failure are due to either a systemic infection or respiratory failure that results from the initial failure of the kidneys. Why does edema occur in patients with kidney disease? Edema forms in patients with kidney disease for two reasons: 1. a heavy loss of protein in the urine, or 2. impaired kidney (renal) function. Heavy loss of protein in the urine The heavy loss of protein in the urine (over 3.0 grams per day) with its accompanying edema is termed the nephrotic syndrome. Nephrotic syndrome results in a reduction in the concentration of albumin in the blood (hypoalbuminemia). Since albumin helps to maintain blood volume in the blood vessels, a reduction of fluid in the blood vessels occurs. The kidneys then register that there is depletion of blood volume and, therefore, attempt to retain salt. Consequently, fluid moves into the interstitial spaces, thereby causing pitting edema. Heavy loss of protein in the urine The treatment of fluid retention in these patients is to reduce the loss of protein into the urine and to restrict salt in the diet. The loss of protein in the urine may be reduced by the use of ACE inhibitors and angiotensin receptor blockers (ARB's). Both categories of drugs, which ordinarily are used to lower blood pressure, prompt the kidneys to reduce the loss of protein into the urine. Impaired kidney (renal) function Patients who have kidney diseases that impair renal function develop edema because of a limitation in the kidneys' ability to excrete sodium into the urine. Thus, patients with kidney failure from whatever cause will develop edema if their intake of sodium exceeds the ability of their kidneys to excrete the sodium. The more advanced the kidney failure, the greater the problem of salt retention is likely to become. The most severe situation is the patient with end-stage kidney failure who requires dialysis therapy. Management Identify and treat factors associated with progression HTN Proteinuria Glucose control Treat pulmonary edema (Bipap) Hypertension Target BP <130/80 mm Hg Consider several anti-HTN medications with different mechanisms of activity ACEs/ARBs Diuretics CCBs HCTZ (less effective when GFR < 20) Metabolic changes with CKD Hemoglobin/hematocrit Bicarbonate Calcium Phosphate PTH Triglycerides Metabolic changes… Monitor and treat biochemical abnormalities Anemia Metabolic acidosis Mineral metabolism Dyslipidemia Nutrition Anemia Common in CRF HD pts have increased rates of: Hospital admission CAD/LVH Reduced quality of life Can improve energy levels, sleep, cognitive function, and quality of life in HD pts Treating Anemia Epoetin alfa (rHuEPO; Epogen/Procrit) HD: 50-100 U/kg IV/SC 3x/wk Non-HD: 10,000 U qwk Darbepoetin alfa (Aranesp) HD: 0.45 g/kg IV/SC qwk Non-HD: 60 g SC q2wks Metabolic acidosis Muscle catabolism Metabolic bone disease Sodium bicarbonate Maintain serum bicarbonate > 22 meq/L 0.5-1.0 meq/kg per day Watch for sodium loading Volume HTN expansion Mineral metabolism Calcium and phosphate metabolism abnormalities associated with: Renal osteodystrophy Calciphylaxis and vascular calcification 14 of 16 ESRD/HD pts (20-30 yrs) had calcification on CT scan 3 of 60 in the control group NEJM 2000; 342(20): 1478-83 Nutrition Think about uremia Catabolic state Anorexia Decreased protein intake Consider assistance with a renal dietician CV disease 70% of HD patients have concomitant CV disease Heart disease leading cause of death in HD patients LVH can be a risk factor Kidney Int 1995; 47(1): 186-92 Acid Base Balance http://www.youtube.com/watch?v=i_pTaTve CCo&feature=related