CALGB 9741
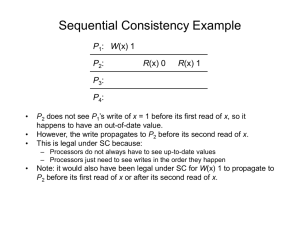
advertisement

C 9741 Marc L. Citron, MD Clinical Professor of Medicine Albert Einstein College of Medicine CALGB Breast Committee C 9741 CALGB: John Carpenter, Donald Berry, Constance Cirrincione, Clifford Hudis, Eric Winer, David Hurd, James Holland, Barbara Smith, Carolyn Sartor, Eleanor Leung, Richard Schilsky, Hyman Muss, Larry Norton. ECOG: William Gradishar, Nancy Davidson. NCCTG: Edith Perez, James Ingle. SWOG: Silvana Martino, Robert Livingston. NCI: Jeffrey Abrams C 9741-CALGB 9741 A Randomized Trial of Dose Dense vs. Conventionally Scheduled and Sequential vs. Concurrent Combination Chemotherapy as Post-Operative Adjuvant Treatment of NodePositive Primary Breast Cancer C 9741 • Dose Density: Administration of drugs with a shortened intertreatment interval. • Sequential Therapy: Application of treatments one at a time rather than concurrently C 9741 Trial Design: Sequential ATC • Based on Hudis et al. Doxorubicin 90 mg/m2 (JCO,1999. 17: 1118) Paclitaxel 250 mg/m2 Cyclophosphamide 3.0 gm/m2 9 cycles, 14 day intervals, G-CSF supported C 9741: • Doxorubicin reduced to 60mg/m2 • Paclitaxel reduced to 175mg/m2 • Cyclophosphamide reduced to 600mg/m2 CALGB 9344 Adjuvant Study N=3,170 Node+ Statification: Premenopausal & Postmenopausal R A N D O M I Z E P4 A60 C 4 A75 C 4 A90 C 4 No P A = Doxorubicin (doses shown) C = Cyclophosphamide (600 mg/m2) P = Paclitaxel (175 mg/m2 – 3 hour infusion) ER+ or PR+ patients received Tamoxifen 5 y C 9741: Trial Design (I) Sequential: A q 3 wk T q 3 wk C q 3 wk (II) Sequential: +filgrastim A q 2 wk T q 2 wk C q 2 wk (III) Concurrent: AC q 3 wk T q 3 wk (IV) Concurrent:+ filgrastim AC q 2 wk T q 2 wk INTERGROUP C9741 2X2 Factorial Design q 2 wk +Filgrastim SEQUENTIAL q 3 wk 24 weeks 36 weeks SEQ Q2 SEQ Q3 16 weeks 24 weeks CONCURRENT CON Q2 doxorubicin 60 mg/m2 cyclophosphamide 600 mg/m2 paclitaxel 175 mg/m2 over 3 hours CON Q3 C 9741: Eligibility Criteria • Stage: T0-3, N1-2, M0 • Primary Surgery: Lumpectomy + axillary dissection or MRM with clear margins • Labs: ANC > 1000/µl platelets > 100,000/µl bilirubin = normal • Other: Normal CXR & EKG C 9741: Endpoints • Primary: Disease-free survival (DFS) Defined as date of study to Local or distant recurrence Or death without relapse • Secondary: Overall survival (OS) Toxicity C 9741: Statistics • 2 X 2 factorial design: - Dose density: 2 weeks vs. 3 weeks - Treatment: concurrent vs. sequential • Target accrual = 1584 pts in 22 mos. • First planned analysis at 3 years after complete accrual • Provided 90% power to detect a 33% reduction in hazard for either main effect C 9741: Methods •Radiation: –After completion of chemotherapy –Per institutional guidelines C 9741: Tamoxifen • Recommended 20mg per day starting within 12 weeks of completion of chemotherapy • Premenopausal patients with ER+ cancers and all postmenopausal patients irrespective of receptor status C 9741: Results • 2005 pts accrued 9/97 & 3/99 • Increased number to compensate for faster than expected accrual • 32 pts did not receive therapy • 1973 pts evaluable & analyzed First Protocol-Specified Analysis MEDIAN FOLLOW-UP 36 MONTHS 600 500 EVENTS RELAPSE OR DEATH 515 400 300 315 200 100 0 CALGB 8541 C 9741 Patient Characteristics N= 484 493 501 495 I II (G-CSF) III IV (G-CSF) No. Nodes+ 1-3 4-9 ≥10 Premenopausal 59% 29% 12% 50% 59% 29% 12% 48% 60% 28% 11% 49% 59% 29% 11% 48% Postmenopausal 48% 51% 50% 50% Patient Characteristics N= I 484 II 493 III 501 IV 495 ER- 34% 35% 33% 32% Tumor > 2cm 60% 55% 58% 58% Lumpectomy 33% 35% 37% 37% Pre- got tam 66% 66% 62% 64% Post- got tam 74% 76% 73% 78% Disease-FreeDisease-Free Survival by Density Survival 1.0 By Density 0.8 0.2 0.4 0.6 q3 0.0 Proportion Disease-Free q2 0 1 2 3 Years From Study Entry q 2 wks q 3 wks N= 988 N= 985 Events= 136 Events= 179 4 Overall Survival Overall Survivalby Density 1.0 By Density 0.2 0.4 0.6 q3 0.0 Proportion Surviving 0.8 q2 0 1 2 3 Years From Study Entry q 2 wks q 3 wks N= 988 N= 985 Events= 75 Events= 107 4 Multivariate Cox Proportional Hazards Model: DFS (N=1892) 1.00 RISK RATIO 0.90 1.00 1.00 0.93 0.80 0.74 0.70 0.60 0.50 0.40 0.30 P=0.58 P=0.010 0.20 0.10 0.00 Seq vs. Con q 3 vs. q 2 wk Multivariate Cox Proportional Hazards Model: OS (N=1892) 1.00 RISK RATIO 0.90 1.00 1.00 0.89 0.80 0.69 0.70 0.60 0.50 0.40 0.30 P=0.48 P=0.013 0.20 0.10 0.00 Seq vs. Con q 3 vs. q 2 wk Estimated Annual Hazards: Q 3wk and Q 2wk .10 Q 3wk .08 .06 Q 2wk .04 .02 .00 0 1 2 Yrs 3 4 Hazard Ratio: Q3wk to Q2wk 1.0 .75 .50 .25 .00 0 1 2 Yrs 3 4 Major Toxicities No. Treated I II III IV Seq q 3 Seq q 2 Con q 3 Con q 2 488 493 501 495 No. Data Granulocytes < 0.5/ul Febrile Neutropenia Hospitalized 99 24% 3% 96 3% 2% 101 43% 5% 101 9% 2% Red Cell Transfusion Platelet Transfusion Neurologic: Severe Sensory Loss or Motor Weakness 0% 0% 1.9% 2% 0% 1.9% 3% 0% 3.9% 13% 0% 4.5% Secondary AML/MDS: % by year Year 1 2 3 9741 0.051% 0.11% 0.18% 9344 0.13% 0.15% 0.17% In 9741, incidence of AML/MDS does not appear to be influenced by filgrastim (slightly higher in q 3-week regimens) Dose Reductions REGIMEN I II III IV During A 7% 5% 3% 3% C 1% 3% 5% 5% T 1% 7% 4% 5% Summary (I) 36 Months Median Follow-Up • Primary Endpoint: Dose-dense treatment associated with a 26% proportional reduction in relapse (p=0.010) • 4- year DFS was 82% for dosedense and 75% for the every three-week regimens Summary (II) 36 Months Median Follow-Up • Secondary Endpoint: Dose dense treatment associated with a 31% proportional reduction in mortality (p=0.013) • 3-Year OS was 92% in the dosedense and 90% in every 3-week regimens Summary (III) • No impact for sequentially or concurrent treatment • Grade 4 granulocytopenia (<500/µl) was more frequent on the q 3-week regimens • Toxicities were acceptable Conclusions (I) • Improved DFS and OS warrant this communication • Advantages of dose density were not accompanied by increase in toxicity • Baseline granulocyte count of 1000/µl is safe for administering chemotherapy Conclusions (II) Caveats: • Additional follow-up needed to confirm survival benefit • Maximum follow-up only 5 years & treatment-related patterns of recurrence and toxicity may emerge • Filgrastim adds cost Conclusions (III) • Results consistent with mathematical models of tumor kinetics • Mathematical concepts may be applied to other drugs and diseases Acknowledgements CALGB: John Carpenter, Donald Berry, Constance Cirrincione, Clifford Hudis, Eric Winer, David Hurd, James Holland, Barbara Smith, Carolyn Sartor, Eleanor Leung, Richard Schilsky, Hyman Muss, Larry Norton. ECOG: William Gradishar, Nancy Davidson. NCCTG: Edith Perez, James Ingle. SWOG: Silvana Martino, Robert Livingston. NCI: Jeffrey Abrams C 9741 Marc L. Citron, MD Clinical Professor of Medicine Albert Einstein College of Medicine CALGB Breast Committee