Pediatric Cardiology in the ED
advertisement

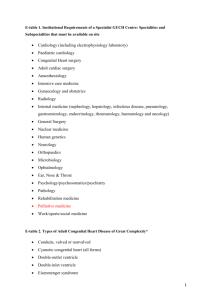
Pediatric Cardiology in the ED Jenn D’Mello and Roger Galbraith Objectives • Have an approach to neonatal/infant presentations of CHD (shock, CHF, tet spell). • Have an approach to the older child with acquired CHF/cardiogenic shock. • Have an approach to pediatric ED patients presenting with syncope, palpitations, or chest pain. • Tips for looking at CXRs when evaluating a child in the ED for cardiac pathology. • Have an approach to the child with known CHD presenting to the ED. Case 1 • 10 day-old infant brought to ED by mother for rapid breathing and poor breast feeding, worsening over past 24 hours. • Previously well with unremarkable prenatal history. • Becoming more lethargic. Initially gasping with feeds, now just not interested in feeding. Case 1 • Afebrile. HR 180, RR 80, BP 85/50, sats 88%. • Infant looks unwell, in respiratory distress, fussy, and has a weak cry. • Nasal flaring and occasional grunting. • Pale, decreased cap refill centrally and in all extremities, and sweaty to touch. • What is your differential diagnosis for neonatal shock? Neonatal Cardiac Physiology Congenital Heart Lesions- Cyanotic vs. Acyanotic? • • • • • • • ASD VSD TOF TGA PDA TAPVR PAPVR • • • • • • • Truncus Tricuspid atresia Ao stenosis Pulmonary stenosis Ebstein’s anomaly Hypoplastic left heart Coarctation of aorta Congenital Heart Lesions- Cyanotic vs. Acyanotic? • • • • • • • ASD VSD TOF TGA PDA TAPVR PAPVR • • • • • • • Truncus Tricuspid atresia Ao stenosis Pulmonary stenosis Ebstein’s anomaly Hypoplastic left heart Coarctation of aorta Age of CHD presentation by lesion First Week • TGA • TAPVR • HLH • Tricuspid atresia First Month (ductal dependent lesions) • • • • 1-6 months (often lead to CHF) • VSD • PDA • Coronary anomalies • TOF • AV canal defect Later Coarctation • ASD Severe AS • PAPVR Severe PS TOF with pulmonary atresia • Valve stenosis Crashing Neonate • CHD presenting as neonatal shock in the first 1-4 weeks is usually due to closure of the ductus arteriosus in a ductal dependent lesion. • Pulmonary or systemic blood flow becomes rapidly compromised. • Most common lesion to present this way is a coarct- make sure you feel the femorals and check a 4 limb BP if in doubt. Management of Neonatal Shock • • • • ABCs Oxygen IV access and fluids, investigations and ? abx PGE1 infusion -start at 0.05 mcg/kg/min, titrate up to 0.2. -should see an effect within 15 minutes. • Call cardiology/arrange transport. PGE1 Side Effects • • • • • Apnea Hypotension Fever Flushing So be prepared to intubate!! Case 2 • 8 week old infant presents with 2 days of cough and congestion. • Today breathing more quickly, sucking in chest, having a hard time feeding than usual. • No fever, vomiting, or diarrhea. • 3 year old sibling has a URTI. Case 2 • Afebrile, HR 160, RR70, BP 80/50, sats 90%. • Nursing describes an alert infant with nasal congestion and respiratory distress with moderate indrawing and retractions. • Sounds like bronchiolitis….but how do you know it’s not CHF? • What do you need to know on history and exam to help you find out? Infant in CHF • Inability of heart to pump adequate blood to meet circulatory and metabolic needs. • Structural causes= VSD, PDA, ASD, AV canal defect, Ao stenosis, PAPVR, anomalous coronary. • Other cardiac causes= SVT, AV block, cardiomyopathy, myocarditis. • May present when pulmonary vascular resistance has dropped to near normal levels so there is gradually increasing L → R shunting. • Can also present when they are tipped into failure by a new illness (e.g. bronchiolitis) Infant in CHF • Need a detailed feeding history. • History of tiring and sweating with feeds or taking a long time to finish feeds should alert you. • May have FTT. • Exam may show grunting, tachypnea, hepatomegaly, FTT, abnormal cardiac exam. • Should always be on your ddx for a wheezing infant. Unrepaired Large VSD Management of Infant in CHF • • • • • • • • • ABCs- may need to support ventilation. Elevate head/chest Oxygen Cardiorespiratory monitoring IV access and blood work EKG and CXR Diuretics (reduce preload) Inotropes if in shock Admit/consult cardiology/arrange echo • http://www.youtube.com/watch?v=YsBM8ep2-M&feature=related • What’s happening? Why? Tet Spell • Occurs in children with CHD causing reduced pulmonary blood flow- classically in TOF. • An episode of severe hypoxia caused by increased R to L shunting and decreased pulmonary blood flow. • Etiology often unclear, can be precipitated by release of valsalva maneuvers when there’s a sudden increase in venous return. Tet Spell • One or more of the following will lead to increased R → L shunting and decreased pulmonary blood flow: – increase in venous return to R heart – decrease in SVR (lower L heart pressures) – increase in PVR (higher R heart pressures) – increase in RV outflow tract obstruction Tet Spell • Child presents with a paroxysm of hyperpnea, prolonged crying, intense cyanosis, and decreased intensity of the murmur of pulmonic stenosis. • They often squat to try and increase their SVR. • Once the spell starts it leads to a vicious cyclethe hypoxia and acidosis cause hyperventilation which further decreases SVR. • This is a medical emergency- it can lead to syncope, seizure, stroke and death. Tet Spell Management • Need to try and decrease hyperventilation, increase SVR, decrease hypoxia. • Knee-chest position • Give oxygen • Try to calm infant- avoid pokes if you can. • If not improving get IV access, give fluids. • Sedate with morphine. • Propranolol 0.2mg/kg over 5 min. • Phenylephrine and bicarbonate. • Likely need ICU/cardiology involvement. May need to use a general anesthetic. Case 3 • 10-year-old boy presents with shortness of breath. • 5 days of cold and cough symptoms, now has worsening fever and cough. • Could just be a pneumonia, but could be acquired heart disease- how will you know? • What types of heart disease are acquired by children? Myocarditis • Inflammation of the myocardium resulting from infectious, toxic, and autoimmune etiologies. • Usually infectious, presents in the winter following a viral prodrome. • Inflammation causes myocardial destruction and results in ventricular dysfunction. Myocarditis • Consider myocarditis in any child with: – Weakness – SOB – Chest pain – Especially if associated with preceding prodromal viral illness – Wheezing child not responding to bronchodilators – Distant heart sounds – Enlarged heart on CXR Myocarditis Management • • • • • • • • • • • ABCs- may need to support ventilation. Elevate head/chest Oxygen Cardiorespiratory monitoring IV access and blood work EKG and CXR Inotropes usually needed- dopamine, dobutamine, milrinone Consider diuretics, afterload reduction (nitroprusside) Don’t forget antibiotics, ?antivirals ICU, cardiology, may need ECMO Basic management is similar to CHF but they are more likely to need inotropes, can deteriorate more rapidly. Other Acquired Heart Disease • Acute Rheumatic Fever – Preceding strep infection – Carditis, migratory arthritis, subcutaneous nodules, erythema marginatum, chorea • Pericarditis – Can look very similar to myocarditis, chest pain may be more prominent – Can develop tamponade Acquired Heart Disease • Endocarditis – Child usually has predisposing factor like artificial valve or central line. – Look for signs of septic emboli. • Kawasaki’s Disease – Fever, irritability +++, conjunctivitis, lymphadenopathy, mucous membranes, palms/soles, rash. – Can develop myocarditis or MI from coronary artery thrombosis. Peds Cardiology- CXR Tips Cardiomegaly • Think about: – CHD – Myocarditis – Pericarditis (effusion, tamponade) – Cardiomyopathy – Ischemia (Kawasaki, congenital) – Arrhythmia – High output failure (anemia, thyrotoxicosis, AVM) Vascularity • Shouldn’t see vessels extending all the way out into the periphery of the lungs- normal is about 2/3. • Most CHD or acquired cardiac pathology causes ↑ blood to go to the lungs but in some there is restriction of pulmonary blood flowpulmonary vascularity on CXR can help you distinguish. Increased Pulmonary Vascularity Decreased Pulmonary Vascularity • • • • • • • • • • • • • • • ASD VSD PDA TGA TAPVR HLHS Truncus Myocarditis Pericarditis Cardiomyopathy Pulmonary hypertension TOF Tricuspid atresia Ebstein’s Pulmonary atresia/stenosis Increased Vascularity ← Decreased Vascularity → CXR Anatomy Classics- The Boot Egg on a string…sure Snowman Big Circle Bigger Circle Biggest Circle Case 4 • 16 year old male presenting with chest pain. • Not in distress, normal vital signs • What cardiac causes of chest pain do you need to rule out? • How will you rule them out (history, exam, investigations)? Chest Pain • Very broad differential- cardiac, respiratory, MSK, GI, psych. • Most commonly it’s related to MSK, respiratory infections, asthma, or GE reflux but there are serious causes that need to be ruled out. • Life-threatening non-cardiac causes to think about= traumatic injury, pneumothorax, pulmonary embolism, asthma, sickle cell crisis. Cardiac Chest Pain • Accounts for <5% of all chest pain. • Causes: – – – – – – Pericarditis Myocarditis MI (Kawasaki, ALCAPA, cocaine use) Arrhythmias Aortic aneurysm HOCM • Should be able to distinguish with exam, ECG, and CXR. • Chest pain on exertion should be referred for further work-up. Case 5 • 13 year old female presents with “heart beating funny” and feeling faint. • Was at karate practice, felt fine prior. During practice felt like she might faint. Sat down and felt better but noticed heart beat felt strange. • Didn’t go away after practice so came to ED. • Has felt this many times before in past 6 months but not concerned because it goes away and “all kinds of strange things have been happening since puberty started”. • Also her mom gets the same thing so obviously nothing to worry about right?.... Case 5 • Has normal vitals except for HR 130. • In no distress, exam normal except for irregularly irregular heart beat and pulse with discordance. • EKG done. Palpitations • May be benign but generally warrant a fairly extensive work-up to be sure. • Prevalence of WPW ~1/500, long QT ~1/5000. • If it’s still occurring ECG should obviously give you the diagnosis. • ECG may also be helpful in sinus rhythm for WPW or long QT. Palpitations • In addition to ECG, also consider: – – – – – CBC Electrolytes (with calcium, magnesium, glucose) Tox screen Thyroid function CXR • Even if work-up is normal, should consider cardiology referral unless there’s an obvious benign etiology. • Recurrent palpitations or palpitations with exercise should always be referred to cardiology. Case 6 • 14 year-old girl presents to ED after fainting at a school dance. • Pale but normal vital signs, alert and embarrassed. • What are cardiac causes of syncope? • How will you rule them out (history, exam, investigations)? Syncope • Much more common and potentially diagnostically challenging ED presentation. • Usually a benign etiology (vasovagal, orthostatic, hyperventilation, or breath holding), but can represent life-threatening pathology. • Approximately 10% are related to migraines, 8% are actually seizures, and 5% have a cardiac cause. Syncope • Cardiac warning signs: – History of known heart disease. – Sudden fainting without prodrome. – Syncope during exercise. – Incontinence during syncope. – Significant injury resulting from syncope. – Family history of sudden death (including single person MVC, drowning). – Family/personal history of deafness. Syncope • Don’t want to miss long QT or HOCM. • ECG should always be part of your work-up. • Consider referring those with normal ECGs but cardiac warning signs (especially syncope during exercise and significant family history) to cardiology. • Anyone with known heart disease and syncope should probably get an urgent echo. Case 7 • A 4 month old infant presents with increasing cyanosis. • Had low grade fever, cough, rhinorrhea and poor feeding for preceding 4 days. • Today developed increased WOB and progressively worsening cyanosis. • Has a history of tricuspid atresia and a BlalockTaussig shunt. • T 38.3, HR 170, RR 70, BP 80/50, sats 75%, infant is crying, cyanotic, grunting and has retractions. • Other than change your pants, what should you do??? What could be going on? Known CHD in the ED • In one study 50% of patients with CHD that presented to the ED required admission, and 10% of those admitted died. • These patients often have complex physiology and are at risk of decompensation for a number of reasons. • So yes, you should panic. CHD in the ED • Most common presentations of CHD patients to the ED are for: – Respiratory tract infection – Dehydration – CHF – Arrhythmia – Tet spell – PLE – Endocarditis CHD in the ED • Patients with poor pulmonary blood flow due to their underlying pathology become profoundly hypoxic with any increase in their PVR (eg. bronchiolitis) and behave like a tet spell. • Patients that already have limited or passive pulmonary or systemic blood flow due to their underlying pathology are very intolerant of any dehydration. CHD in the ED • Bottom line: – You probably won’t have enough time or information to figure out exactly what’s causing their problem- an extensive inpatient work-up is often required. – Have a low threshold for admission, possibly ICU. – Have a low threshold for cardiology consult. – Don’t be stingy with fluids and oxygen, they often need one or both, just monitor their response closely. The End • Savitsky et al. Emergency department presentations of pediatric congenital heart disease. Journal of Emergency Medicine 2003; Vol 24:239-45. • Fleisher et al. Textbook of Pediatric Emergency Medicine 5th edition. • APLS- Advanced Pediatric Life Support Cardiovascular System Lectures I and II • Thanks to Gavin Burgess and Roger Galbraith