Systemic Lupus Erythematosus (SLE) in Pregnancy
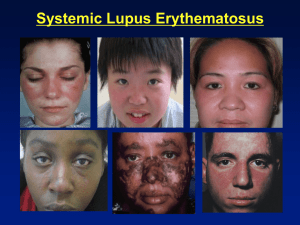
advertisement
Dr. Anupama Kumar Consultant Rheumatologist Sagar Hospital, Bangalore Biological prerogative of every woman Pregnancy in lupus is not contraindicated Many lupus patients deliver healthy babies Many families at least want one child Fertility is not affected in patients with lupus SLE is the most common autoimmune multisystemic disease to affect women in child-bearing years Prognosis for both mother and baby have important implications during pregnancy Marriage, pregnancy and childbirth are burning issues for most patients Characterized by production of antibodies to cell nucleus called ANAs Who is affected 90% are young women 90% of them are in 20 to 40 years age group More patients plan for pregnancy because of improved prognosis Pregnancy outcomes are good when lupus is in remission Ideally lupus should be inactive for six months Serious disease such as active lupus nephritis, myocarditis, seizures is a contraindication Teratogenic drugs like cyclophosphamide, methotrexate should be stopped six months before conception Lupus patients for pregnancy counseling Known lupus cases coming for antenatal care Undiagnosed or misdiagnosed lupus in pregnancy Asymptomatic pregnant patients who have history of neonatal lupus or concerned antibodies Fatigue and fevers Arthritis or arthralgias Malar rash Serositis Raynaud’s phenomenon Proteinuria Vasculitis Leukopenia Thrombocytopenia Seizures Complete blood count Anti Nuclear Antibodies by IF or HEP2 Anti double stranded DNA antibodies Anti Ro and Anti La antibodies Complement studies-C3 AND C4 Urine analysis Renal function tests Lupus anticoagulant and Anti cardiolipin antibodies Mild risk cases-Mild disease, those who are in remission, on no medication except mild ones High risk cases-Severe active disease. Major organ involvement,those with Anti Ro or APL antibodies Moderate risk cases-Majority are in this group H/O Previous pregnancy with complication Underlying kidney, heart or lung disease Active phase of the disease Presence of Anti Ro and Anti La antibodies A history of previous thrombotic event APLA Additional factors like maternal age>40 years and pregnancy with twins or triplets Risks of Lupus to pregnancy Pregnancy loss Preterm delivery Eclampsia Neonatal lupus due to Ro and La antibodies Risks of pregnancy to lupus Lupus flares Progressive renal disease Maternal thromboembolism Miscarriages(before 20 weeks) is the most common form, averaging about 20% Stillbirths are especially increased in Lupus 11% Neonatal lupus and death due to CHB because of Anti Ro and Anti La antibodies APS related repeated pregnancy failures Increased lupus activity at conception or during pregnancy Hypertension Hypocomplementaemia Renal disease Gestational Lupus Spontaneous abortions IUGR Preterm delivery postpartum haemorrhage maternal venous thromboembolism Neonatal death due to fetal heart block High blood pressure in the mother after 20 weeks of pregnancy Occurs in ~13% of women w/ SLE Tx: DELIVERY Delivery may be delayed in some women who are less than 34 weeks to give steroids for lung maturity Occurs in about 2% of babies born to mothers with anti-Ro/SSA and or anti-La/SSB antibodies Caused by passage of the antibodies from the mother’s bloodstream across the placenta to the developing baby after about 20 weeks Signs of neonatal lupus includes red, raised rash on the scalp and around the eyes that resolves by 6-8 months (because the antibodies clear the blood stream) SLE complications in babies: complete heart block and learning disabilities Risk of neonatal lupus in subsequent pregnancy is 17% Fetal bradycardia should be investigated looking for maternal Anti Ro antibodies as mothers may be asymptomatic or may develop lupus later All suspected neonates should have an ECG as CHB recquires permanent pacing Subsequent pregnancies have more risk of neonatal lupus Lupus flares are seen in all trimesters In mild to moderate lupus, 40% show no change, 40% flare and 20% improve Flares are more common when disease is active at conception Renal flares are most feared Postpartum flares are common as beneficial effect of steroid produced by placenta wears off The pattern of the diseases activity is usually repeated in subsequent pregnancies Musculoskeletal and cutaneous flares are common and easier to manage by increasing the dose of prednisolone IV Methylprednisolone may be required for severe flares Use or continuation of Azathioprine is allowed HCQ not to be discontinued as it is seen to cause flares Low, but higher than general population Lupus related deaths are due to HELLP Syndrome Thromboembolism associated with APS Pulmonary hypertension Infection following severe lupus flare Chloasma or malar rash Proteinuria of pre-eclampsia or worsening lupus nephritis Thrombocytopenia in pregnancy (HELLP) or that of lupus exacerbation oedema and fluid accumulation in joints in late pregnancy or arthritis of SLE Prenatal counseling Frequent antenatal check up Monitoring of disease activity-CBC, monthly urine analysis, monthly complements Fetal surveillance by frequent ultrasound Patients may need anticoagulation Combined care: Rheumatologist, Obstretitian and Nephrologist if required Lupus patients are normally fertile Lupus pregnancies are successful two thirds of the time Mild to moderate lupus does quite well in pregnancy Steroids are safe for exacerbation of lupus in pregnancy Hydroxychloroquine should not be stopped in pregnancy