Case Studies from the Pulmonary Function Laboratory
advertisement

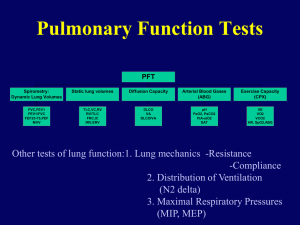
Case Studies from the Pulmonary Function Laboratory Angela Lorenzo, MS, RRT, RPFT Respiratory Care Division School of Health Sciences Focus Conference on Respiratory Care and Sleep Medicine, May 2013 Nashville, TN Indications for PFTs Establish baseline of pulmonary function Determine presence/severity of disease Monitor disease progression/improvement Monitor response to therapy Pre-operative assessment Disability evaluations Occupational lung disease Case 1: Ankylosing Spondylitis and MAC c/o DOE 53 y/o male, Ht 72 “, Wt 90 lbs, Smoker- 39 pk/yr hx, c/o DOE 4 Months ago released from hospital for hemoptysis, Rx’s with antibiotics & Home O2 Chest Imaging: LUL cavitating lesion with an enlarging mycetoma, new densities in RUL & LLL, widespread pulmonary fibrosis Sputum + for M. xenopi in past (now -) Case 1: Ankylosing Spondylitis and MAC c/o DOE Also has Crohn’s Disease and treated with 6MP (mercaptopurine) which in rare cases can cause pulmonary fibrosis Pt had been treated with Remicade in past (antiTNF) associated with TB infections Case 1: Ankylosing Spondylitis and MAC FVC: 1.47 L (28%) FEV1: 1.37 L (33%) FEV1%: 93% MIP: 52% predicted MEP: 26% predicted Unable to perform DLCO or N2 washout due to leak Limited ability to open mouth-could not use mouthpiece Case 2: Alpha-1 Antitrypsin Deficiency 64 y/o male with history of A-1AD Has pulmonary and liver involvement Currently taking Aralast 5 g IV weekly Up to 15% pts have liver involvement Alpha-1 proteinase inhibitor Increased exercise tolerance since beginning A1PI therapy Progressive weight loss has stabilized Case 2: A1AD FVC: FEV1: FEV1%: FEF 25-75% PEFR TLC FRC PL RV DLCO 70%; 4.47 L 2.63 L 59% 0.99 L/sec 8.09 L/sec 7.64 L 5.00 L 3.09 L DLCO/Hb 67%; (98%) (74%) (29%) (93%) (111%) (141%) (129%) DLCO/VA 42% Case 2: A1AD Alpha-1 antitrypsin is produced in the liver Protects the lungs from the effects of elastase A-1A inactivates elastase carried on WBCs in the lungs Elastase destroys alveoli Prolastin, Zemaira, Aralast Case 2: A1AD Year 2009 1/2010 12/2010 FVC 3.53 4.47 4.14 92% 4.05 92% FEV1 2.38 2.63 2.50 70% 2.51 73% FEV1/FVC 67% 59% 60% FRC 2012 62% 4.30 121% 4.53 129% 132% 3.62 149% RV 3.31 3.09 3.17 DLCO 58% 70% 61% 58% Case 2: A1AD Diagnosed 6 years ago presenting with DOE, reactive erythrocytosis 2/2 hypoxia On A1PI 5 years Liver cirrhosis diagnosed 7 years ago, stable at this time Weight loss has stabilized No limitations on activity Case 3 CREST/ILD 64 y/o male with CREST is being evaluated for ILD. Pt also has goiter. Previous PFTs WNL when pt tested to see if goiter was obstructing trachea Case 3: CREST/ILD FVC 2.60 L 60% FEV1 2.11 L 62% FEV1% 81% FEF25-75% 2.15 67% PEF 7.56 89% No bronchodilator Post-loops assessed effect of goiter on airway Case 3: CREST/ILD TLC 4.45L VC 2.75 L FRC N2 2.63L ERV 0.94 L RV 1.69 L RV/TLC 38% DLCO DLCO/VA 66% 63% 74% 65% 69% 98% 58% 52% Case 4: Asthma, Allergies, DM2 54 y/o asthmatic with hx DM tested Pulmonary Medication profile: advair singulair, albuterol prn (used 5 canisters in a 6 month time frame) At age 49 pt sought treatment for a suspected latex allergy Pt had known seasonal allergies. Case 4: Asthma, Allergies, DM2 Allergy skin testing + for pollens, grass, trees, dust mites, feathers, dogs, cats, tree nuts, shell fish, some other foods Blood tests were – for latex x 2, + some foods Pt agreed to Immunotherapy. 1st PFT 4 years prior to beginning IT 2nd PFT 2 years IT FeNO 4 years IT Case 4: Asthma, Allergies, DM2 FVC FEV1 FEV1% FEF25-75 2.68L 1.98L 74% 1.44 85% 75% 27% 6.32 104% L/SEC PEFR Pre/Post Case 4: Asthma, Allergies, DM2 FVC FEV1 FEV1% FEF25-75 2.58L 85% 2.52L 79% 80% 2.82 57% L/SEC PEFR 5.96 134% Case 4: Asthma, Allergies, DM2 2003 FVC FEV1 FEV1% FEF25-75 2.68L 1.98L 74% 1.44 85% 75% 27% L/SEC PEFR L/SEC 2009 FVC FEV1 FEV1% FEF25-75 2.58L 85% 2.52L 79% 80% 2.82 57% L/SEC 6.32 104% PEFR L/SEC 5.96 134% Case 4: Asthma, Allergies, DM2 2012 worsening symptoms after URI 2 weeks after URI, sinus complaints, productive cough. No fever, chills Baseline FeNO 17 ppb Peak symptoms FeNO 54 ppb Advair increased to 250/50: FeNO 34 ppb Advair increased to 500/50: FeNO 17 ppb Baseline dose 100/50 resumed: FeNO 17 ppb Case 4: Asthma, Allergies, DM2 Advair Dose FeNO Resting Blood Sugar 100/50 15-19 100-110 100/50 54 160’s 250/50 34 140’s 500/50 17 100 100/50 17-19 90-110 Case 5 72 y/o physician “curious” to see what cigarettes have done to her lungs and what a PFT feels like. Approx 75 pack year history No respiratory complaints Case 5 Case 5 Case 6: Bronchiectasis 49 y/o male with hx severe COPD, pulm TB for which he began tx 1994 TB relapsed due to noncompliance. Completed multi-drug tx > 1 yr 1996 Now has stable biapical scarring/cavitation Sputum + MAC 3 of 4 cultures, no MAI tx 25 pack year smoking hx, quit 8 years ago Case 6: Bronchiectasis Presents for f/up and sputum induction No wt loss, night sweats, fever, chills Good appetite, good ET >3-4 flights stairs + phlegm varies clear to brownish, no blood Chest CT: extensive bilat old granulomatous disease with bullous and cavitary changes, significant volume loss in upper lobes, bronchiectatic changes, fibrosis/scarring noted Case 6: Bronchiectasis Year 2007 2009 FVC 3.12L 63% 3.89L 76% FEV1 1.27L 32% 1.10L 27% FEV1/FVC 41% 28% SVC 92% 3.89L IC 75% 2.70L ERV 153% 1.19L 70% FRCpleth 130% 4.35L 122% RV 145% 3.17L 144% DLCO/VA WNL 64% R/A Pulsox 97% 98% 76% Pt began Tx with spiriva, foradil, asmanex and albuterol prn in 2007. Asmnex d/c’d 2009 Case 7: Parkinson’s Disease 62 y/o male with hx Parkinson’s disease (1998) eosinophilic PNA 2006-nml eos since 2008 Worsening SOB at rest, band-like radiating chest tightness that has increased over the last several weeks and gets worse as his Parkinson’s meds wear off Parkinson’s meds: carbidopa levodopa (Sinemet) q 2h (past 8 years), Selegiline (4 years); past use comtan d/c’d 2/2 side effects Case 7: Parkinson’s Disease 2 hours later, feeling SOB FVC After Parkinson’s Meds 3.98 L FEV1 2.98 L 1.77 L FEV1FVC 75% 99% 1.79 L Case 7: Parkinson’s Disease Mask facies, tachyneic, speaks in short sentences, lungs clear with shallow respirations As dopa wore off, PFT pattern changed to restricted- muscle rigidity affecting respiratory muscles which is rare Dyspnea is a described side effect of carbidopa levodopa Case 7: Parkinson’s Disease Case 8: Amiodarone 79 y/o male with h/o cardiomyopathy and subsequent Afib. Pt now on amiodarone Pt c/o DOE The following tests were ordered: spirometry and static lung volumes DLCO was not ordered Amiodarone known to cause pulmonary fibrosis Case 8 : Amiodarone FVC FEV1 FEV1% FEF25-75 2.68L 1.98L 74% 1.44 85% 75% 27% 6.32 104% L/SEC PEFR L/SEC Case 8 : Amiodarone TLC 7.49L VC 4.68L FRC PL 3.80L ERV 0.99L RV 2.81L RV/TLC 38% 94% 95% 95% 61% 95% 84% Case 8 : Amiodarone DLCO: 41% predicted Discussion followed: was decreased DLCO due to interstitial edema 2o to cardiac failure or lung disease? Side effects: Interstitial pneumonitis, fibrosis Dyspnea, non-productive cough - common presenting symptoms Decreased TLC and DLCO Case 9: DOE, CLL, Lymphoma 63 y/o male with Small Cell Lymphoma and Chronic Lymphocytic Leukemia c/o DOE and persistent unprod cough, 20 pack year hx, quite 11 years ago Rituximab: cardiac= angina, arrhythmia; pulm = Obliterans bronchiolitis, pneumonitis Fludarabine: pulm- cough, hypersensitivity reactions, pulmonary fibrosis, interstitial infiltrates Cytoxan: cardiac- cardiomyopathy; pulm – interstitial pneumonia Case 9: DOE with CLL, Lymphoma FVC FEV1 FEV1% FEF25-75 PEFR 2.90L 2.12L 73% 1.50 6.02 59% 56% 43% 67% Case 9: DOE with CLL, Lymphoma TLC 4.74L VC 2.97L FRC PL 2.54L ERV 0.77L RV 1.77L RV/TLC 37% DLCO (Hb 10.8) DLCO/VA 63% 60% 68% 47% 70% 90% 44% 49% Anti-Neoplastic Drugs Hypersensitivity reactions: characterized by cough, SOB, bronchospasm, urticaria, allergic alveolitis/pneumonitis Procarbazine, Azathioprine (Imuran), Asparginase Pulmonary fibrosis: Busulfan (Myleran), Cyclophosphamide (Cytoxan), Bleomycin, Chlorambucil (Leukeran), Melphalan Case 10: Lung Cancer/Resection 68 y/o male referred to PFT Lab for pre-op evaluation for LUL lung cancer Pt is a 40 pack year ex-smoker who quit 10 years ago. DOE, Productive cough He presented nearly one year later for follow up PFTs Case 10: Lung Cancer/Resection Pre-op s/p Left Upper Lobectomy FVC 2.44L 53% 2.27L 50% FEV1 1.55L 44% 1.47L 42% FEV1/FVC 64% FEF 25-75 0.58L/Sec 18% 0.73L/Sec TLC 4.18L 59% 3.89L 54% VC 2.56L 59% 2.34L 51% FRCpleth 2.29L 62% 2.24L 61% ERV 0.66L 44% 0.69L 46% RV 1.63L 63% 1.55L 60% RV/TLV 39% DLCO 65% 40%