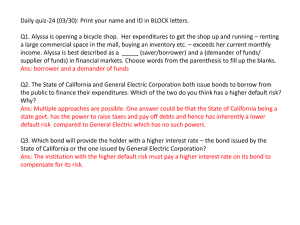
"Best Practice" Tools and Resources to Improve
advertisement

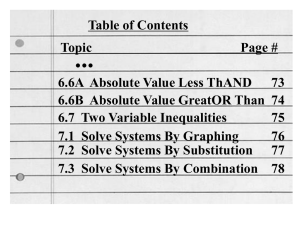
IMPLEMENTING “BEST PRACTICE” TOOLS AND RESOURCES TO IMPROVE NUTRITION 2011 Indiana Healthcare Leadership Conference on Improving Nutrition March 31, 2011 in Indianapolis, Indiana. Brenda Richardson MA, RD, LD, CD Objectives- Attendees can: • Identify “Best Practice” for Nutrition • Know Resources • Implement at the Facility Level 2 •Federal •State •Professional Organizations •Identify the Team •Team Responsibilites •Staff/Residents/ Families •Programs •Policies/Procedures • Training/Education • QI Customers •Vendors/Contracts I. Know what II. Facility III. Facility ”Best Practice” Team Systems and Management Processes Is for LTC 3 RESOURCES: •Federal • State • Professional Organizations I. Know what Nutrition ”Best Practice” Is for LTC 4 Examples of Resources for Best Practice VISULIZE ACTIVITIES WITH TIMELINES! State and Federal Gov Agencies (CMS, ISDH, Health Dept, AoA, etc) SOM MDS QUALITY HEALTH DEPT Professional Organizations (ADA, AMDA, NPUAP, CDC, etc. NPUAP ADA CONSUMER & Consumer Organizations (AARP, NCOA, etc) DMA AAHSA Others: QIOs, Pioneer Network, USDA, CDC, FDA, AMDA, ASPEN, etc. AHCA AARP Remember that “whatever nutrition assessment and care planning resources are used, they are expected to be: - current, - evidence-based or expertendorsed research and clinical practice guidelines/resources” 6 • • • • • • • • II. Facility Team Management Identify a Nutrition “Oversight” Team Nursing Registered Dietitian Dietary Manager/ Diet Technician Registered Speech Language Pathologist Quality Improvement Medical Director CNAs Others (Pharmacist, Occupational Therapist, etc.) 7 Identify Team Responsibilities • Nursing/ Director of Nursing, Unit Mgrs, CNAs, others • Registered Dietitian (Indiana Certification, Skills and Competencies, Professional Involvement) • Dietary Manager/ Diet Technician Registered • Speech Language Pathologist • Quality Improvement • Medical Director • Others (Pharmacist, Occupational Therapist, etc.) 8 • • • • • • • • Communication with Staff, Residents and Families Memos In-services Newsletter In-Services Department Head Meetings Change in Shift Meetings Care Plan Meetings Others (Website, etc) 9 III. Systems And Processes • Key Facility Nutrition Programs • Nutrition Manuals • Menu and Vendor Programs • Customer Satisfaction • Quality Improvement 10 III. Systems And Processes • Key Facility Nutrition Programs - Food service program - Dining program - High Risk Nutrition - Weight monitoring program - Hydration program - Skin and wound care program - Nutritional supplement program - Quality Improvement program 11 III. Systems And Processes Manuals: • Policy/Procedure Manuals: • Current, Best Practice, Reflect What your Facility Does, Staff is educated/trained. • Diet Manual: • Current and Best Practice (Indiana Dietetic Association Diet Manual, Company, Others) 12 III. Systems And Processes Manuals: State Operations Manual (SOM) •Requirements in 42 CFR Part 483, Subpart B, • Know The Survey Process, Survey Forms, Appendix P - Survey Protocol for Long Term Care Facilities - Part I and Appendix PP- Guidance to Surveyors for LTC Facilities • Know the Deficiency Criteria and Determination and the Plans of Correction 13 III. Systems And Processes Manuals: • RAI Manual • Additional References • Client Education Material 14 III. Systems And Processes Menus: Seasonal Reflect input from Clients Reviewed and Approved by RD Vendor/Manufacturer Programs Meet requirements, services, resources, team player. 15 III. Systems And Processes Customer Satisfaction - Resident Council, Newsletters, Surveys - Be present during all meals and get input. - Provide follow-up and responsiveness. Culture Change: - Eden Alternative, Pioneer Network, Advancing Excellence in NH Campaign, CMS Survey & Certification Process Quality Improvement: - Nutrition Programs, Weights, Heights, QMs, Meal Serice, Dining, etc. 16 Using a “Best Practice” Clinical Practice Guideline American Medical Director’s Association (AMDA) “Altered Nutritional Status in the Long-Term Care Setting” Revised in 2010 17 Altered Nutritional Status (ANS): Unintended and unexpected change in weight that is likely to indicate an undesired alteration in intake or utilization of nutrients. CPG Guidelines (27 steps): RECOGNITION – Steps 1 - 3 ASSESSMENT – Steps 4 - 14 TREATMENT – Steps 15 - 22 MONITORING – Steps 23 - 27 Definition of Altered Nutritional Status (ANS): Unintended and unexpected change in weight that is likely to indicate an undesired alteration in intake or utilization of nutrients. Note: Differentiate Protein-Energy Undernutrition (PEU), Cachexia, and Sarcopenia from Altered Nutritional Status (ANS). (Although these may present as ANS) 19 STEP 1 Perform a baseline evaluation of the client’s nutritional status. - Admission Weight - Height - BMI - Eating Preferences - Baseline testing - MDS - MNA© - SF RECOGNITION 20 STEP 2 Identify Risk Factors. - History of recent weight loss - Functional disability - Pressure Ulcer - Terminal Illness - Depression - Medication - Therapeutic Diets - Nausea/Vomiting/ Diarrhea - Fluid Retention/Edema - Underlying Infections RECOGNITION 21 STEP 3: Observe routinely for changes in weight or food intake that may indicate ANS. - Wt changes: ≥ 5% in 1 month, 7% in 3 months, 10% in 6 months - Decline in food/fluids (not to exceed 7 days) - BMI approaching underweight - Persistent, unexpected, and unintended weight loss for 3 consecutive months - Pressure Ulcer - Abnormal Labs - Uncontrolled disease processes RECOGNITION 22 STEP 4 Confirm existence of a nutritional problem that requires additional assessment. - Validate measurements - Weight change is truly unintentional or unexpected - Evaluate client willingness to undergo a diagnostic assessment * If client or family chooses to not intervene then decision and rationale should be clearly documented (see step 13) ASSESSMENT 23 STEP 5 If there is weight loss: Establish that the client is eating the food received. - Anorexia (Go to step 6) - Weight loss despite normal intake (Go to step 9) - Hyperphagia (Go to step 9) ASSESSMENT 24 STEP 6 If food intake is inadequate, screen for functional impairments. - Observe while eating - Evaluate for oral pain - Observe swallowing ability - Evaluate adequate feeding assistance ASSESSMENT 25 STEP 7 If food intake is inadequate, screen for social and environmental factors, dietary restrictions, and food preferences. - Reassess food preferences - Review necessity for dietary restrictions - Evaluate environment where meal is served: homelike, noise, odor, lighting, eating alone - Evaluate time of meals and portion sizes ASSESSMENT 26 STEP 8 If food intake is inadequate, screen for medical conditions associated with anorexia or dehydration. - Consider fluid electrolyte imbalance - Changes in mood or behavior - Review all meds - Presence of infections - Gastrointestinal pathology and motility disorders - Order chest x-ray and labs if indicated ASSESSMENT 27 STEP 9 If there is weight loss despite normal intake, screen for a malabsorption syndrome and for conditions that increase nutritional needs. - Inadequate caloric intake - Increased metabolic need - Malabsorption ASSESSMENT 28 STEP 10 Screen clients who gain weight for conditions related to fluid retention. - 1-2 L of fluid (2-5 pounds in weight) can infiltrate lower extremity tissues before edema is evident - ↓ fx - Advanced organ system disease - Aggressive IV therapy ASSESSMENT 29 STEP 11 For clients who lose weight: Evaluate whether a continued search for the cause of weight loss is appropriate. - Repeat client hx and physical exam in light of recent wt change - Order additional labs and radiologic studies on the basis of any new findings in the “second-look” hx and physical exam ASSESSMENT 30 STEP 12 For clients who gain weight: Evaluate whether a continued search for the cause of weight gain is appropriate. - Determine if related to fluid retention - Determine if gain has negatively affected fx, quality of life, or management of comorbid conditions. ASSESSMENT 31 STEP 13 Identify and document unavoidable ANS. Unavoidable when 1 or more applies: - No remediable cause for the change in weight - Although cause is identified, client has not responded to therapeutic interventions (steps 15-20) - Further interventions may harm with no reasonable expectation of benefit. ASSESSMENT 32 STEP 14 Summarize the results of the assessment of the client’s ANS. - Document ANS - Describe all conditions contributing to ANS - Project prognosis and likely clinical course - Update care plan to indicate all palliative care interventions with concurrent document to evaluate effectiveness. ASSESSMENT 33 STEP 15 Address each identified risk factor and potential cause of ANS identified in Steps 1-13. - For each identified risk factor establish a planned intervention TREATMENT 34 STEP 16: Address factors that may affect the eating environment in the LTC facility. - Pleasant and conducive for dining - Foods attractive and palatable - Consider having more than one meal setting - Flexibility in staffing where clients need assistance - Use non-nursing staff and volunteers to assist set-up and socialization - Happy hour before meals - Use smell to stimulate appetite TREATMENT 35 STEP 17 Tailor meals and foods to individual preferences. - Individualize meal plan - Promote flexibility in meal times - Allow eating at client pace - Invite family to bring client’s favorite foods in - Honor resident preferences- ethnic, regional and personal - Appropriate consistency - Provide adaptive devices - Provide Finger Foods for those that cannot use utensils TREATMENT 36 STEP 18 Reconsider any dietary restrictions. - Special diets for diabetes, hypertension, heart failure and hypercholesterolemia have not shown to improve control of or affect symptoms - Late-stage renal insufficiency is exception- protein restriction may delay onset of diabetes (no protein restriction necessary with dialysis) - Altered consistencies TREATMENT 37 STEP 19 Consider ways to supplement the client’s diet. - Increase nutrient density of foods - Offer snacks - Consider giving a multivitamin and mineral supplement - Distribute liquid nutritional supplements during medication pass. TREATMENT 38 STEP 20 Consider use of appetite stimulants on an individual basis. - Increase activity/exercise - Use is controversial - Consider on individualized basis TREATMENT 39 STEP 21 Evaluate risks and benefits of artificially administered nutrition and hydration by tube feeding. - May be clinically appropriate in some circumstances: Clear clinical indication Provides benefit not outweighed by risks Consistent with known values and preferences of client and family - Consider risks and benefits TREATMENT 40 STEP 21-continued Evaluate risks and benefits of artificially administered nutrition and hydration by tube feeding. - Consider risks and benefits complicated by misconceptions: Loved one will “starve” to death Will reduce comfort and promote suffering - Actually may cause diarrhea, abdominal pain, local complications and increase risk of aspiration TREATMENT 41 STEP 22 Summarize the results of treatment interventions on the client’s ANS. Document: -Treatment plan and compliance -Complications or side effects of interventions -Trends in wt loss or gain -Strategy for monitoring response and adjustments -Prognosis and likely clinical course TREATMENT 42 STEP 23 Monitor effectiveness of treatment interventions. - Weight stabilization is primary endpoint - Document at least monthly if persists - Document when resolved MONITORING 43 STEP 24 Monitor all clients regularly to identify ANS as early as possible. - Admission- weigh weekly for first 4 weeks. If weight is stable weight monthly thereafter - Monitor per ANS criteria - MDS monitoring tool - Review advance directives annually and when clinical status changes - Monitor lab values as needed MONITORING 44 STEP 25 Monitor to ensure that each ANS risk factor identified in the admission evaluation is addressed. - Have mechanism for tracking risk factors identified in admission evaluation - Link to a planned intervention - Monitor care plan and effectiveness of the intervention MONITORING 45 STEP 26 Monitor the incidence and prevalence of ANS in the facility. - Significant weight changes - Decline in food intake over several days (not to exceed 7 days) - BMI approaching underweight range - Unexpected and unintentional wt loss persists for 3 consecutive months - Abnormal labs MONITORING 46 STEP 27 Monitor the assessment process. - QI process with mechanism for tracking the assessment process when a client triggers an evaluation for ANS. MONITORING 47 It is imperative that health care providers are aware of nutritional issues and that optimal achievable nutritional status is maintained to ensure the health, well-being, and quality of life for our aging population. Thank You Brenda Richardson, MA, RD, LD, CD Email: brendar10@juno.com 48