APS - West Virginia Physical Therapy Association
advertisement

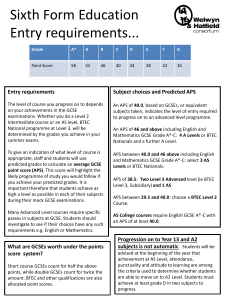
WVPTA 2012 Spring Conference IRG dba APS Healthcare, Inc. Update Presented by: Denise Burton, Utilization Management Coordinator Updates APS (UMC) Background/Introduction Provider Registration with APS Current System based on active Medicaid Manual Chapter 515 Occupational/Physical Therapy Services Upcoming Changes when new Chapter 515 is released (currently under comment) Demonstration- PT portion of APS Medical CareConnection® Denials and Reconsiderations Tips and tricks for Using APS Medical CareConnection® (C3) FAQ’s Contact Information APS Background/Introduction Utilization Management Contractor for WV Medicaid Prior Authorizations Developed direct data entry system for prior authorization request submissions, called CareConnection®, or C3 Sub-contracts WVMI to review requests Provider Registration with APS Providers must register specifically with APS Healthcare in order to access the Medical CareConnection® Providers must be WV Medicaid enrolled in order to register with APS- providers enroll in WV Medicaid through Molina Providers who try to register with APS and ARE NOT WV Medicaid enrolled will be unable to submit prior authorization requests APS Registration Process There is a self-registration portal available at https://c3wv.apshealthcare.com; on the log-in page select self-enrollment Brief instructions on registration are being passed around- for more detailed instructions go to http://apshealthcare.com (WV program medical providers tab) or contact us at: wvmedicalservices@apshealthcare.com Provider Eligibility Verification for Prior Authorization Requests APS will check provider eligibility based on provider enrollment information from Molina (daily file update). The provider enrollment governs the provider’s ability to create requests (access); ability to request certain service types (limited to certain provider types); ability for the prior authorization to be linked to the appropriate Medicaid Provider ID or NPI in the Molina system. The organizations created upon registration with APS are linked to provider enrollment in Molina (one organization can be created in the APS system to link to many Medicaid ID or NPI numbers OR many organizations can be created in the APS system to link to a single Medicaid ID or NPI number). The REFERRING PROVIDER MUST be a WV Medicaid enrolled provider. Current System for PT Prior Authorization Requests BOTH APS Medical CareConnection® AND WVMI Legacy system may be used at present Prior Authorization is presently required after 20 PT/OT visits If using the APS system select clients as “established” Registration with APS is required to use the new system Present Requirements Compared to upcoming Requirements in Proposed Manual Current Manual PA required after 20 visits of PT/OT Both APS and WVMI system available Existing fax forms available for WVMI and new fax forms for APS system mimic web New Manual PA required from 1st serviceinitial authorization requires minimal data for autoadjudication-subsequent visits require PA with current data demand-initial number of visits is not yet determined (WVPTA is recommending 20 as with current system 30 days post “go-live” (date TBA after release of new manual) ONLY APS system may be used and WVMI legacy system is no longer available Only fax forms in use mimic APS system once WVMI system is no longer available Retrospective Review Policy Retrospective review is available in the following instances: Weekends or holidays, or at times when APS/WVMI is closed. Retrospective reviews must be initiated within 72 business hours following the service; Member eligibility has been back-dated and must be initiated within 12 months of the date of service; A procedure/service denied by the member’s primary payer provided all requirements for the primary payer have been followed including the appeals process (must submit EOB, copy of denied payment). Turn around time for processing of retrospective requests is 72 hours (3 business days); reviews that require physician review may require an additional 24 hours, depending upon the nature of complexity of the case. If the retrospective request DOES NOT meet the criteria for processing, it will not be reviewed for medical necessity (policy denial). If the retrospective request meets the criteria for processing, the normal review process will ensue. Denials and Reconsiderations Status can be seen at the authorization record level OR in reports. Denial letters are always found on the Summary & Submit page of C3. If you entered the prior authorization request in C3, you will be messaged to your C3 inbox. Reconsiderations are requested from the action menu for requests that have been denied for medical necessity. Providers have 60 days to request reconsideration, so make sure all appropriate information is provided at the time of the reconsideration request. If you mail your reconsideration chart, wait until it is mailed prior to requesting in system and indicate in the note that the record has been mailed (or faxed if you do not attach at the time of reconsideration request). Timeframes for Reconsideration Provider must request and submit reconsideration with all pertinent documentation within 60 calendar days from member/provider notification of the service denial. APS/WVMI have 14 calendar days to complete the review and notify the provider and member of results. C3 Tips Authorization Start Date must be the earliest Service Start Date if multiple services are requested. You must be registered as the provider type indicated for the review area. If you provide many types of services you must expand your registration as each review area is added to be sure requests can be made. Remember to save your work- some areas (e.g. notes require a save within the page). If you hit save and not save and continue the record will be saved in your work queue. Please be patient. We know the system is slow sometimes, but IT believes the cause of cases not going to the WVMI work queue is submit button being pushed prior to all information being loaded to the Summary & Submit page-there are multiple additional validations at the time of submission so this takes time! Review Statuses Saved: in provider’s work queue/not submitted Pending: in WVMI’s work queue, awaiting review In Process: with nurse/physician reviewer Closed: either duplicate, inappropriate recon request, or TPL case Complete: Case has been reviewed. The denial reason and letter can be found at the record level and the PA number is at the record level OR in the daily report. Submitted: User who worked case has only AUM Provider role/not AUM Manager role so the case has not been submitted to APS. FAQs Who do I contact with questions and concerns? A: Clinical inquiries will continue to be handled by WVMI, technical inquiries (log-on, passwords, registration, C3 assistance, etc.), training requests and questions about CareConnection® will be handled by APS. Complaints should be directed to APS and will be routed to the appropriate parties for follow-up. APS- Medical Services: 1-800-346-8272; Email: wvmedicalservices@apshealthcare.com WVMI-PT/OT Review: 1-800-982-6334, Option 1, Fax #: 1.877.762.4338 Who do I contact if I have a question about a prior authorization? A: If you are trying to determine if the case has been denied or approved, first look in the C3 system. If you do not know how to do this, please call APS and we will teach you how. If you have faxed a request to WVMI, are registered with APS and do not see it in the C3 system, call WVMI. If you are not registered with APS, call APS to get registered. What do we do if we realize the date of service is wrong? A: Contact APS either by phone or email explaining what the correct date of service should be, the authorization request ID, and any other pertinent information related to the case. APS will issue an IT ticket and within 72 hours, you will be able to re-submit your bill. Where do I find what covered services are available to members? A: BMS Manual Chapters are available on the BMS website at www.dhhr.wv.gov/bms. APS Contact Information Main Telephone:1-800-461-0655 Medical Services ONLY:1-800-346-8272 Local: 304-343-9663 Voicemail ONLY: ext. 6954 Fax: 1-866-209-9632 Web Address: www.apshealthcare.com/wv General Medical Services email: wvmedicalservices@apshealthcare.com Helen Snyder, Associate Director ~ hcsnyder@apshealthcare.com ext. 6911 Heather Thompson, UM Nurse Reviewer ~ hthompson@apshealthcare.com ext. 6907 Sherri Jackson, Office Manager ~ shjackson@apshealthcare.com ext. 6902 Denise Burton, Utilization Review Coordinator ~ eburton@apshealthcare.com ext. 6949 Alicia Perry, Eligibility Specialist ~ aperry@apshealthcare.com ext. 6937 Jackie Harris, Eligibility Specialist ~ jharris@apshealthcare.com ext. 6928 LeAnn Phillips, Eligibility Specialist ~ lphillips@apshealthcare.com ext. 6906 Screenshots of Prior Authorization Submission Physical Therapy Search Member Screen Search Member Cont’d Create New Request Screen Member Demographics Screen Provider Information Screen Administrative Screen Service Selection Screen Search Provider Screen Search Provider Screen Cont’d Service Selection Cont’d Service Selection Cont’d Service Selection Completed Diagnosis Screen Diagnosis Screen Cont’d Diagnosis Screen Cont’d Evaluation Screen Treatment Screen Treatment Screen Cont’d Treatment Screen Cont’d Summary and Submit Screen Summary and Submit Screen Cont’d