Community Palliative Care Team
advertisement
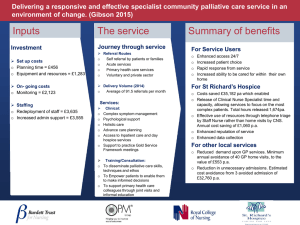
Community Palliative Care Team What do we do? Dr Faith Cranfield Medical Lead, Community Palliative Care Team, St Francis Hospice Background Home care service established by daughters of charity in 1989 – in a portacabin in Capuchin Friary in Raheny 1995 – Inpatient unit (19 beds) opened SFH Raheny Two community teams – East and West 2011 – West team moved to new SFH Blanchardstown Catchment Area Who do we see? Cancer patients. All have incurable, progressive disease. Some continue palliative chemotherapy. Patients with MND Patients with other progressive fatal diseases –terminal care patients receive full service. Others receive Palliative Medicine review to advise GP on symptom management, end of life decisionmaking. Children with life-limiting illnesses Location of care Home Nursing homes Homeless hostels Long term psychiatric hospitals Sheltered accommodation Team members Nurses 14 WTE CNS, including 1 WTE Management (0.5 East CNM, 0.5 West CNM) Medical director ¾ WTE 2 Registrars 2 Full-time Chaplains 2 WTE Social workers Activity 2012 New referrals: 974. New patients taken on: 702. Referral source: GP-204 Beaumont-261 Mater-228 James Connolly-39 Other 260 Nursing visits 8557, Medical visits 693 Deaths 701. Home-323, St Francis Hospice -626, other -390 What The CPC Team Can Offer Specialist palliative care to patients Specialist palliative advice on patient management to professionals (GPs, nursing home staff) Support for patient’s family and professional carers 24 hour availability of telephone advice Working hours Mon- Fri normal working hours – regular phone calls and visits 4:30-9pm Single nurse on call for North Dublin, can do home visit if necessary 9pm til 8:30 am Telephone advice via night nurses in Inpatient Unit in Raheny Accessing the service Referral received Next working day: urgency for visit categorised based on need – diagnosis and disease extent, prognosis, functional status, palliative care needs Waiting time: variable –urgent referrals warrant telephone contact to explain what the need is, identify if a visit is possible. First visit. Once seen, patients given contact details and can access 24 hour advice. Where do we fit in? GP remains primary carer Hospital care continues as appropriate Ongoing nursing telephone support and visits (NB all changes warrant review of effectiveness) PHN continues to review for pressure care needs, dressing needs, assessment and access to community physiotherapy/OT and to home carer support Input by CPC Team Visits by CNS– frequency will depend on needs, patient preference, patients hospital appointments etc. Often weekly. Social work assessments/support At home/at hospice/Family meetings Chaplaincy visits at home Referral to Day care or Inpatient care as appropriate Volunteer Service Introduction of Hospice Often emotional – for patient and family Breaking bad news Dying Anxiety re: changing care/health Sense of abandonment Getting to know new team of health care professionals Challenges Establishing a good rapport – trust Dealing with collusion Balancing patient and family needs Not meeting expectations e.g. hands on care Ensuring consistency amongst healthcare professionals information Assessment Symptom assessment – physical. Clarifying medication. Addressing emotional / psychological / spiritual concerns Address family concerns Offer counselling / support Offer volunteers Daycare In-patient Care Liaise with other health care professionals Physical Symptoms Fatigue/Lack of energy/Weakness Anorexia Pain Dry mouth/sore mouth Nausea Early satiety Vomiting Constipation Diarrhoea Dyspnoea Cough Delirium Poor sleep Restlessness Falls Psychological Issues Loss of role Worry about family Loss of dignity / privacy Fear of dying in pain Financial difficulties The meaning of life Loss of future Helplessness / being a Anxiety burden Fear of death Loss of control Depression Psychological Issues for Family Grief and distress Exhaustion – emotional and physical Coping with competing demands Their loved ones distressed Unfamilarity with death and dying Fear of what is to come Fear of being incompentent Fear of doing harm Disagreement/discord within family Spiritual distress Trying to make sense of things –the Why? Of what is happening. Trying to find meaning Concerns about afterlife Prayer for support Decision making at home -in the event of physical change What do we think is the cause? Information Access to tests. Mostly clinical assessment, +/- CIT Is it reversible? Will treating the cause change the outcome? Does this warrant admission? What are the symptoms and how can we alleviate them? What does the patient want? In light of the change, is the situation sustainable? Medication Huge source of distress Poor swallow Weakness Drowsiness Under dosage Over dosage Nutrition Food important part of life - Shows love and concern - Sharing / nurturing Food becomes a burden Issue of starvation Natural process Burden and benefit Physical Environment House Stairs Downstairs Toilet Unsuitable accomodation Lack of equipment Lack of carers Example –JD, 48 JD, 48 y/o lady with metastatic non-small cell cancer. On chemotherapy. Separated working mother, selfemployed. Two children. Seen at home. Angry, wary. Concerns raised re: teenage daughter – acting up, not aware of extent of disease. Planning for future care of daughters. Chemotherapy poorly tolerated –vomiting, sepsis. Stopped. Recovers partially. Family meeting re: illness. Develops vomiting. Due to see solicitor at home that evening re: will etc SC infusion antiemetic. GP review. Bloods by CIT – hypercalcaemia and uraemia Glad of admission via day ward for fluids and bisphosphonate D/C home on SC infusion. Stopped after a few days. Develops back pain – known bony vertebral disease. Settles with opioids –problematic constipation. Referred to radiation oncology. Receives thoracic XRT. Progressive weakens over weeks. Spending much of the day in bed. Worried re: children. Expressing wish to die in hospice, but stay at home as long as manageable. Back pain escalates over a week –medications titrated with GP. Falls secondary to leg weakness and difficulty passing urine. Catheterised. Listed for admission to St Francis. No bed. Night-nurse organised. Bed becomes available. JD admitted to St Francis for terminal care. Dies after a two week admission. Difficulties For CPC Team Working In Other Institutions Nursing home staff fill dual role – professional carer / locum family member Homecare assumptions re: nurse/carer familiarity with palliative drugs Difficulty meeting family members – unlike home Changes in medication often slower to achieve than in the home Liaising and communicating With whom? The patient The family The GP The PHN Irish Cancer Society Night nursing service CIT The Hospital team A and E Anticipatory planning Misconceptions We visit at anytime We stay all the time We come when someone dies We come in an emergency We replace all other community services – we come in and take over We have immediate access to beds We arrange everything We insist people know we are from the hospice Why do it? Achievement – Enabling family to cope Enabling patient to die at home Improving someone’s subjective quality of life –when time is short, the quality of each day can become very important Challenging Privilege Thank you for listening Any questions?