Diet low in Vitamin D
advertisement
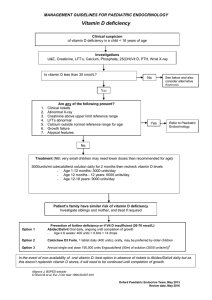
Dr Katy Gardner (Chair, Liverpool Vitamin D group) katyagarnder@btinternet.com June 2012 Works with Calcium to build bones/skeleton Role in muscle function Recent evidence: heart disease, diabetes, Multiple Sclerosis, cancer and TB: recent conference.... 40 diseases!! MS in Scotland: evidence increasing BUT NB almost all = ecological studies “association” Sunlight (90 %) - UVB converted in skin to Vit D3: At least 15 minutes a day on arms/face from April to October: NB more if darker skin Diet (10 %) includes : Oily fish Dairy products, esp. Fortified marge Eggs Breakfast cereal (fortified) Liver and red meat Green veg (small amount) and mushrooms Bone Pain, Muscle Weakness, Waddling gait OSTEOMALACIA Also: Hyperalgesia, Lethargy/ tiredness Falls and fractures in older people Babies: irritability, twitching, convulsions. Rickets…early: delayed closure of fontanelles Rickets…..later: bow legs or knock knees, bone pain, poor growth, delayed walking, tender swollen joints (wrists) Delayed eruption of teeth. Lethargy ... may be assoc with anaemia Skin colour: darker…..in UK: African origin (e.g. Somali), South Asian (e.g. Bangladeshi) or Arabic (e.g. Yemen), Chinese Low exposure to sunlight: e.g. dark skin, mostly covered, spend most time indoors (modern life!!!), fear of sun Diet low in Vitamin D: vegan/vegetarian, lack of fortified foods, use of chapatti flour, unleven bread Medical conditions: Coeliac , Crhons Older people: esp. if mostly indoors Pregnancy and breastfeeding People coming from abroad may be fine for several months........ Winter is the worst time Obesity BMI >30 (Diagnosis and management of vitamin D deficiency : Pearce S, Cheetham T. BMJ 2010;340:b5664) Eg: Mother not identified when pregnant, not picked up again when breast feeding, child not identified till symptoms 2 cases in 2011 in my practice of 4000 patients NB one child: Rickets =family at risk Congenital rickets, mother Vitamin D deficient in pregnancy, parents cleared of murder Missed at post mortem: the severity of his condition and its manifestations were “effectively outside the clinical experience of any of the medical witnesses” (BMJ 2012) Could it happen here? Dept of Health. Vitamin D- advice on supplements for at risk groups. CMO letter 2012 www.dh.gov.uk/health/2012/02/advicevitamin-d/ Liverpool Somali study 2004 292 Somalis in L’pool all ages >age 2 82% deficient Community supplement study: low uptake, unpleasantness of Calcium was a main factor (J Bunn, K Gardner, K Vithlani, B Brabin, M Mohamud, S Salah, I Kahin, J Dutton, B Durham, W D Fraser (2004) “The prevalence of vitamin D deficiency in the Somali community of Liverpool: a significant problem” ) 6% Vitamin D3 levels 11% deficient<14 ng/ml 82.4% insuficiency15-24 adequacy>25 Health promotion messages did not correspond to people’s diet Somalis ate little food containing Vitamin D 75% had someone in family suffering from bone and muscle pain (Maxwell S, Salah S, Bunn J. (2006) Journal of Human Nutrition and Dietetics, 19 (2), p.125-7.) Neighbouring practices very different knowledge and testing rates Guidelines distributed Re audit 2009: increased numbers diagnosed! Test people at risk/with symptoms and treat if deficient Implement DOH, NICE re prevention ensure full uptake of Healthy Start and ......beyond Educate:/lifestyle NB: not enough evidence to treat insufficiency Available at www.northmerseyammc.nhs.uk/publications More info from: katyagardner@btinternet.com Future action: audit uptake and continuing awareness, aim to roll out Healthy Start to all ≤30 nmol/L 31–50 nmol/L >50 nmol/L >150 nmol/L effects deficiency insufficiency adequate possible evidence of adverse BUT remember time of year!!!! Autumn beware false high reading! Loading dose: 300,000 units Colecalciferol 20,000 units daily for 15 days or Colecalciferol 20,000 units 5 x daily for 3 days OR Ergocalciferol 300,000IU IM injection once or twice a year (variable availability) Check levels after 6 months Maintenance: tricky!!! Equiv 800 units daily for life Read Code .C28 Vitamin D deficiency NICE: Maternal and child nutrition 2009 “People at risk of low sun exposure should take 10mcg/400units Vit D daily” (consensus statement 2010) If ineligible for Healthy Start advise 10mcg Vitamin D (400IU) daily – OTC (COMA) Pregnant women at risk should be tested Treat if deficient (follow local guidelines), continue while breast feeding Family members need to be supplemented if woman is deficient Seamless transition from midwives to health visitors and to GPs (recent local audit showed this not always the case) Ideally supplement children under 5 (Healthy Start misses many at risk and uptake low) ABIDEC and DALVIT fine Childrens treatment guidelines expected soon What is the optimal Vit D level? Does it effect pregnancy outcomes? (BMJ 2012) Can higher levels reduce risk of cancer and other chronic diseases? How much sun exposure needed to optimise levels in different skin types? What is the role of diet and supplements in achieving optimum Vit D? Who should we test and treat? How can we ensure that we don’t have our own baby Jayden here?