A Six-Session Evidence-Based Protocol for the Treatment of
advertisement

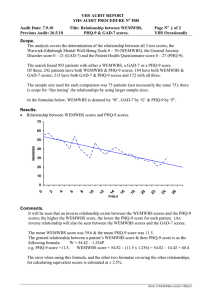
Session #A3a Friday, October 17, 2014 A Six-Session Evidence-Based Protocol for the Treatment of Individuals with Chronic Pain in a Primary Care Setting Abigail Lockhart, PsyD, Postdoctoral Psychology Fellow Laurie Ivey, PsyD, Clinical Psychologist Samantha Monson, PsyD, Clinical Psychologist Collaborative Family Healthcare Association 16th Annual Conference October 16-18, 2014 Washington, DC U.S.A. Faculty Disclosure We have not had any relevant financial relationships during the past 12 months. Learning Objectives At the conclusion of this session, the participant will be able to: • Describe a brief six-session individual treatment intervention that can be implemented by Behavioral Health Providers in integrated care settings. • Describe how to facilitate improved communication with the patient’s PCP and other PCMH treatment providers in order to promote collaborative models of care. • Identify strategies for recruiting patients in primary care. • Describe how to support patients develop sustainable life changes after the six sessions are complete. Bibliography / References Carlson, M. (2014). CBT for Chronic Pain and Psychological WellBeing: A Skills Training Manual Integrating DBT, ACT, Behavioral Activation and Motivational Interviewing. John Wiley & Sons. McCracken, L. M., Sato, A., & Taylor, G. J. (2013). A trial of a brief group-based form of acceptance and commitment therapy (ACT) for chronic pain in general practice: pilot outcome and process results. The Journal of Pain, 14(11), 13981406. McCracken, L.M., & Vellman, S.C. (2010). Psychological flexibility in adults with chronic pain: A study of acceptance, mindfulness, and values-based action in primary care. Pain, 148: 141-147. Vowles, K.E., & Thompson, M. (2011). Acceptance and Commitment Therapy for chronic pain. In L.M. McCracken (Ed.) Mindfulness and acceptance in behavioral medicine: Current theory and practice (pp. 31-60). Oakland: New Harbinger Press. Wetherell, J.L. et al. (2011). A randomized, controlled trial of acceptance and commitment therapy and cognitivebehavioral therapy for chronic pain. Pain, 152: 2098-2107. Learning Assessment • A learning assessment is required for CE credit. • Question and answer opportunities will be incorporated throughout this presentation. Prevalence of Chronic Pain Condition Number of Sufferers Source Chronic Pain 100 million Americans Institute of Medicine of The National Academies (2) Diabetes 25.8 million Americans American Diabetes Association (3) (diagnosed and estimated undiagnosed) Coronary Heart Disease (heart attack and chest pain) Stroke 16.3 million Americans Cancer 11.9 million Americans American Heart Association (4) 7.0 million Americans American Cancer Society (5) American Academy of Pain Medicine, Get the Facts on Pain - http://www.painmed.org/patientcenter/facts_on_pain.aspx Stats Pain is a significant public health problem that costs society at least $560-$635 billion annually Institute of Medicine Report: Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research, 2011 Worldwide, up to 22% of primary care patients suffer from chronic debilitating pain* 53% of chronic pain patients treated on an ongoing basis are treated by primary care physicians* * By the Numbers: Pain Management and Primary Care Published Online: Wednesday, June 27th, 2012. www.painlive.com Colorado Medicaid Study Nearly 15,000 Medicaid patients in Colorado had one or more of those traits in the year analyzed, which put them at a risk of overdose from 9- 14 times higher, depending on the trait exhibited At least 1 of those traits showed up in 174 Medicaid patients who overdosed in the year studied 556 beneficiaries, 15 of whom overdosed, had all 3 traits Evidence Base • “When added to usual care, both ACT and CBT can improve pain interference, depression, and pain-related anxiety in individuals with chronic pain.” Wetherell, J.L. et al. (2011). A randomized, controlled trial of acceptance and commitment therapy and cognitive-behavioral therapy for chronic pain. PAIN, 152: 20982107. 3. Standardized instruments Brief Pain Inventory (Short Form) PHQ-9 GAD-7 Intra-patient data collection 1. 2. Collaborative Model of Pain Management PATIENT CULTURE PAIN PARTNERS PROVIDER PATIENT PATIENT PARTNERSHIP Perspective of letting the patient be the guide to ensure productive outcome Facilitation of communication amongst the team PROVIDER PARTNERSHIP PROVIDER Helpful when providers partner (decreases dread) Co-consult with patient beginning, middle, end Intervention most effective if physician partners Reinforcing skills AMAP Checking in with patient on what is most helpful Supportive partnership/stance in decreasing/maintaining medications or eliminating opiates—holding the Rx line! CULTURE 1. 2. 3. 4. CULTURAL PARTNERSHIP What do you think caused(s) the pain (problem)? Has anyone else helped you with this pain (problem)? How so? Are there things that help you that our doctors don’t know about? What kind of treatment do you think you should receive? Kleinman, A., Eisenberg, L., & Good, B. (1978). Culture, illness, and care: Clinical lessons from anthropologic and cross-cultural research. Annals of Internal Medicine, 88(2) CULTURE CULTURAL PARTNERSHIP Through attuned questioning, you may find… …pain = distress (e.g., trauma response). Session 1 Introduce 6 session outline Partnership Goals, including goals of the intervention: To develop a curiosity for engaging with pain in an alternative way Screening Tools 1. Brief Pain Inventory (Short Form) 2. PHQ-9 3. GAD-7 4. Culture Questions 5. Assess physician/team relationships & lay framework for team Review BPI with patient, focus on how pain is interfering with the patient’s functioning Discuss difference between acute pain and chronic pain Homework – Complete Valued Living Questionnaire Session 1 Introduce 6 session outline Partnership Goals, including goals of the intervention: To develop a curiosity for engaging with pain in an alternative way Screening Tools 1. Brief Pain Inventory (Short Form) 2. PHQ-9 3. GAD-7 4. Culture Questions 5. Assess physician/team relationships & lay framework for team Review BPI with patient, focus on how pain is interfering with the patient’s functioning Discuss difference between acute pain and chronic pain Homework – Complete Valued Living Questionnaire Shared Pain Management Plan: Session 1 1. Relay culture question answers 2. Medication goals (maintenance, decrease, other) Session 2 Review Valued Living Questionnaire Develop functional goals based on individual responses on Valued Living Questionnaire MIND/BODY CONNECTION Negative emotions and pain – pathways intersect in the brain A-B-C Model How you think about pain, it is the way you are going to feel What are your beliefs about pain? What can you do to help? Keep your mind busy, Self-talk Explore thoughts and emotional reactions to sensations in the body – Introduce body scan Homework – Body scan Session 2 Review Valued Living Questionnaire Develop functional goals based on individual responses on Valued Living Questionnaire MIND/BODY CONNECTION Negative emotions and pain – pathways intersect in the brain A-B-C Model How you think about pain, it is the way you are going to feel What are your beliefs about pain? What can you do to help? Keep your mind busy, Self-talk Explore thoughts and emotional reactions to sensations in the body – Introduce body scan Homework – Body scan Shared Pain Management Plan: Session 2 1. Values 2. Functional goals Screening Tools 1. Brief Pain Inventory (Short Form) 2. PHQ-9 3. GAD-7 Session 3 Gate Control Theory of Pain Current stressors that may exacerbate pain Role of sleep in the management of chronic pain Adaptive vs. Maladaptive Coping Skills Discuss Sleep Hygiene and provide handout Evaluate beliefs about medications, opiate use, illicit drug use What adaptive coping skills are you already using? Review “A-B-C’s” (Adding Pleasure, Building Mastery, Coming Back to the Present Moment) Homework - Pleasant and unpleasant events calendar Session 3 Screening Tools 1. Brief Pain Inventory (Short Form) 2. PHQ-9 3. GAD-7 Gate Control Theory of Pain Current stressors that may exacerbate pain Role of sleep in the management of chronic pain Adaptive vs. Maladaptive Coping Skills Discuss Sleep Hygiene and provide handout Evaluate beliefs about medications, opiate use, illicit drug use What adaptive coping skills are you already using? Review “A-B-C’s” (Adding Pleasure, Building Mastery, Coming Back to the Present Moment) Homework - Pleasant and unpleasant events calendar Shared Pain Management Plan: Session 3 1. Barriers Identified 2. Plan to address Session 4 Review pleasant events scheduling homework Discuss barriers Increasing Positive Experiences Nutrition What foods should be avoided Drink recommended amount of water Avoid alcohol and nicotine Exercise Discuss current activity level and explore barriers Why exercise helps Alternative ways to be active Homework – Build in at least one new activity to pleasant events calendar Session 4 Review pleasant events scheduling homework Discuss barriers Increasing Positive Experiences Nutrition What foods should be avoided Drink recommended amount of water Avoid alcohol and nicotine Exercise Discuss current activity level and explore barriers Why exercise helps Alternative ways to be active Homework – Build in at least one new activity to pleasant events calendar Shared Pain Management Plan: Session 4 1. Gains/Positive experiences to date Session 5 Review new activity homework, address barriers RELAXATION Why relaxation helps Review and practice relaxation strategies Diaphragmatic breathing Guided imagery CALM exercise BUILDING NETWORK OF SUPPORT Tree of support exercise Homework – Schedule time to practice relaxation strategies Session 5 Review new activity homework, address barriers RELAXATION Why relaxation helps Review and practice relaxation strategies Diaphragmatic breathing Guided imagery CALM exercise BUILDING NETWORK OF SUPPORT Tree of support exercise Homework – Schedule time to practice relaxation strategies Shared Pain Management Plan: Session 5 1. Additional gains 2. Ongoing support team & plan for future Session 6 Review homework Final session screenings 1. Brief Pain Inventory (Short Form) 2. PHQ-9 3. GAD-7 SUSTAINING CHANGE Create plan for addressing barriers to sustaining change (e.g., flare-ups and bad days) How to involve your network of support How to utilize your PCP Homework – Talk to at least one person in your support network about how they can help you stay on track Session 6 Review homework Final session screenings 1. Brief Pain Inventory (Short Form) 2. PHQ-9 3. GAD-7 SUSTAINING CHANGE Create plan for addressing barriers to sustaining change (e.g., flare-ups and bad days) How to involve your network of support How to utilize your PCP Homework – Talk to at least one person in your support network about how they can help you stay on track Shared Pain Management Plan: Session 6 1. Additional gains 2. Ongoing support team continued…. Patient Pearls I have worked with a number of different mental health providers and no one has ever asked me about my pain.* By asking me to participate in this intervention, you really validated my pain and how much it impacts my health.* • Paraphrased from patient interactions Pearls combat Dread Resources for Patients Managing Pain Before It Manages You, 3rd Edition by Margaret Caudill, MD, PhD, MPH Get Out of Your Mind and into Your Life: The New Acceptance and Commitment Therapy by Steven Hayes, PhD Session Evaluation Please complete and return the evaluation form to the classroom monitor before leaving this session. Thank you!