PUD
advertisement
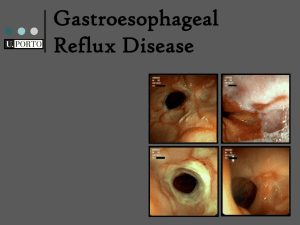
In the name of God Peptic Ulcer Disease By: E. Salehifar (Clinical Pharmacist) Peptic Ulcer Disease (PUD) PUD: 10% of the people in their lifetime Prevalence of active disease: 1-2% Duodenal ulcers Gastric ulcers Others: Ulcers of esophagus Zollinger-Ellison (gastrin-producing tumor) Upper Gastrointestinal Disorders Dyspepsia 25-55% of the people in their lifetime Abdominal pain or discomfort Symptoms of early satiety, bloating, nausea & vomiting Nonulcer Dyspepsia: 60% PUD: 20% GERD: 20% GERD Backflow of GI contents into the esophagus resulting in esophagitis Classic symptom: Heartburn or burping up of stomach contents into the mouth Major concern: Barrett’s esophagus (a predisposing factor for esophagus cancer) Mucus secreting cells Antrum: G cells (Gastrin) Body: Parietal cells (H+, IF), chief cells (Pepsinogen) Stomach physiology Fundus (mucus-secreting cells) Body (80-90%) Parietal cells (acid, intrinsic factor) Chief cells (pepsinigen) Antrum (10-20%) G cells (gastrin) Regulation of acid secretion Increase Decrease ACH Histamine Gastrin PGE Cholecystokinin Glucagon VIP What is the cause of PUD? No acid, No Ulcer! (PH) Helicobacter pylori (HP) NSAIDs Cigarette Smoking HP: A Gram negative spiral bacteria HP Was isolated in 1983 (Campylobacter pylori) Infection is more common in older individual Person to person transmission Is found most consistently in gastric antrum pathogenesis: Urease (↑NH3), cytotoxin, inflammation, breakdown of mucosal defense Why HP is implicated in PUD? 90% of PUD, in the absent of NSAIDs exposure, are associated with HP Is found in 90% of DU & 70% of GU patients Eradication of HP accelerates the ulcer healing and decreases the recurrence rate PUD in HP negatives is rare HP: Is not a single cause of PUD! HP positive: 50-90% of general population 15-30%: PUD 20-40%: Nonulcer dyspepsia 30-65%: Asymptomatic HP infection is not associated with acute perforated DU When PUD occurs? Aggressive factors Defensive factors HP H+ Pepsin NSAIDs (Direct, ↓PGE) Smoking (↑H+ & bile salt reflux, ↓PGE & mucosal blood flow) PGE Somatostatin Mucus HCO3¯ Mucosal blood flow Rapid regeneration Resitution Clinical presentation The most common symptom: epigastric pain Pain is not well localized DU pain commonly occurs with empty stomach and relieves by food and antacid GU pain occurs at any time frequently immediately or 1-3 hours after a meal Clinical presentation (continue) Pain dose not always correlate with ulcer especially in elderly taking analgesics and in patients with high pain tolerance Other symptoms: nausea, vomiting, belching, bloating & anorexia endoscopy is needed for definitive diagnosis PUD: Is there any role for foods? Caffeine, milk, alcohol, spicy foods increase acid secretion and cause dyspepsia, but they can not increase risk of PUD Acute alcohol ingestion can damage the gastric mucosa, leading to GI bleeding, however alcohol has not been proven to cause PUD PUD: Genetic association 20-50% of patients with DU have a positive family history of PUD PUD: Association with Stressful life Stressful life events thought by some to exacerbate PUD Epidemiology (incidence & prevalence) Increase in PUD during the beginning of the 20th century with a peak in 1950s Over the past 2 decade, DU have declined (both outpatient & inpatient episodes) GU has remained stable perhaps due to aging & use of ulcerogenic drugs PUD (Geographic variation) In Japan, GU is 5-10 times more common In the US & European countries, DU is 2 times more common PUD (gender) In 1968, rate of PUD in men was twice, but now is similar for men & women Hospitalization of women with GU have increased markedly for patients older than 65 PUD (age) GU is rare before age 40, and the peak incidence occurs from ages 55-65 The incidence of DU increase with age until the age of 60 years PUD (morbidity & mortality) Mortality of PUD has declined during the past 20 years Less than 2% of patients receiving therapy are expected to have a complication One of the most common GI diseases that results in loss of work and high-cost service Comparison of DU & GU DU Increases with age Common in US Hyperacidity Hypergastrinemia ↑ parietal cell mass Genetic influence Incidence ↓ ↑ frequency in cirrhosis More common in blood O GU Rare before 40 Common in Japan Normal or low acid Normal or sl. ↑ gastrin Normal parietal cell mass No genetic influence No ↓ in incidence No ↑frequency in cirrhosis More common in blood A Treatment Goals Relief of symptoms Promotion of ulcer healing Prevention of ulcer recurrence and complications Treatment Eradication of HP (seropositive DU & GU) Acid suppression (DU) PPIs H2-blockers Antiacids Enhancing mucosal defenses (GU, DU) Sucralfate Treatment In HP (+) patients: Eradication of HP In HP (–) patients: H2 blockers, Sucralfate & antacid are equally effective, but H2 blockers are much easier to use with less drug interactions PPIs may be slightly more effective than H2 blocker and should be reserved for refractory cases H2 Blockers Cimetidine (Tagamet) Tab: 200mg, Inj: 200 mg/2ml Ranitidine (Zantac) Tab: 150 mg, Inj: 50 mg/2ml Famotidine Tab: 20 mg, 40 mg B B B H2 Blockers (indications) DU GU GERD ZE have equal efficacy (70-95% healing rate after 4-8 weeks of therapy) Potency & duration of action of famotidine (& nizatidine) is greater, but all can be used once daily In GERD, all H-2 blockers should be used before meals H2 Blocker dosage for DU & GU Cimetidine: 300 mg QID, 400 mg BD, 800 mg HS Ranitidine: 150 mg BD, 300 mg HS Famotidine: 20 mg BD, 40 mg HS -Dosage adjustment in moderate to severe renal insufficiency -Sr Cr may increase with cimetidine H2 Blockers (Adverse Effects) Are remarkably safe Common: GI (diarrhea, constipation), CNS (confusion, headache, dizziness, drowsiness), Rash Gynecomastia & Impotence: Cimetidine Heptotoxicity: Ranitidine Drug interactions Cimetidine: Phenytoin, Warfarine, theophylline Cimetidine & Ranitidine: Procainamide & NAPA (↓tubular secretion) All H2-Blockers: Ketokonazole, Fe Proton pump inhibitors (PPIs) Omeprazole (Prilosec®) Cap: 10, 20 mg Lansoprazole (Prevacid®) Cap: 15, 30 mg Rabeprazole (Aciphex®) Tab: 20 mg Pantoprazole (Protonix®) Tab: 20, 40 mg - PPIs relieve symptoms and heal ulcer more quickly than H2 Blockers (2-4 W compared to 4-8 W) PPIs (Pharmacokinetic) Enteric-coated granules within capsule Bioavailability: 30-80% Omeprazole & lansoprazole are prodrugs for O. sulfonamide, L. sulfone, hydroxy lansoprazole Despite the short t1/2, antisecretory effects is present 72 hr No dosage adjustment in renal disease PPIs (ADRs) ADRs are relatively negligible Include GI (nausea, diarrhea, abdominal pain), CNS (dizziness, headache), rash, gynecomastia, ↑ SGOT, SGPT No risk of hyperplasia and carcinoid tumor in spite of hypergastrinemia PPIs (Drug Interactions) Omeprazole decreases metabolism of diazepam, phenytoin, warfarin (2C9) Less interaction with Lansoprazole Pantoprazole also is metabolized by sulfotransferase, it appears to interact less with cyp450 Rabeprazole can modestly increase Dig Sucralfate (Carafate®) Protects ulcerated tissue from aggressive factors (pepsin, acid, bile salts) PH 2-2.5 → forms a physical barrier to injury Not absorbed systemically Other protective actions on the mucosa (PG, bicarbonate) Duodenal ulcer (active, maintenance) & Gu Sucralfate (ADR) Constipation Dry mouth Nausea Rash Eradication of H.Pylori Monotherapy not recommended PPI or bismuth + two antibiotics Amoxicillin Clarithromycin Metronidazole Tetracycline OCA (10 days) Omeprazole: 20 mg BD Clarithromycin: 500 mg BD Amoxicillin: 1000 mg BD LAC (14 days) Lansoprazole 30mg bid before meals Amoxicillin 1000mg bid with meals Clarithromycin 500mg bid with meals OC Omeprazole 20mg BID, 30days Clarithromycin 500mg TID, 14days LCM, OCM (14 days) PPI: (Lansoprazole 30 mg BD or Omeprazole 20 mg BD), 2 weeks Clarithromycin: 500 mg BD, 2 weeks Metronidazole: 500 mg BD, 2 weeks Summary Importance of HP in development of PUD Clinical symptoms of DU & GU Treatment principles