Integrated Health: Creating Successful Outcomes Through
advertisement

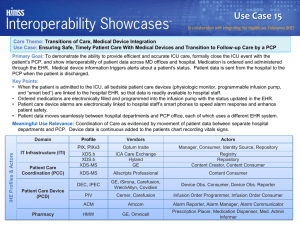
Integrated Health: Creating Successful Outcomes Through Technology Innovations Mary Jo Whitfield, MSW VP Behavioral Health Services Cheri DeBree, MC Integrated Health Director Robin Trush, MA Director of Special Projects Presentation Objectives Gain insight into successful integrated health programmatic elements: Clinical & Operational Learn how the JFCS electronic health record (NextGen) assists in clinical decision making Learn how to operationalize data and outcomes to manage program elements Increase audience knowledge about technology advancements and the use of data exchanges Why Integrate Physical and Behavioral Health Care? • Behavioral and physical health care have historically operated in silos. • Health care integration is designed to: • • • • Improve patient access to care in a setting where patients are most comfortable. Reduce health care disparities. Contain costs by promoting a whole health approach. Improve patient outcomes through coordination of care. Key Drivers of Integrated Health • Patient Protection and Affordable Care Act • State Health Insurance Exchanges • Mental Health Parity • Medicaid Expansion National Driver: Affordable Care Act • Health Insurance Exchanges • Mental Health Parity • Medicaid Expansion Models of Integrated Care & Benefits • Coordinated Care • Co-Located Care • Transformed/Full Integration • Virtual Integration Jewish Family and Children’s Services …Who are we? • Outpatient Behavioral Health Provider - Maricopa County • In operation since 1935 • JFCS is Currently serving 5,025 adults and 4,838 children and has about 90% Medicaid client population • Our enrollment reflects the cultural diversity of our county • Magellan Behavioral Health of Arizona • Community Re-investment Grant Integrated Health Program Data • Adult Program began May 1, 2012 • Children’s Program began August 1, 2013 • 1750 adult clients served • 134 Child clients served to date • 750 active clients in the program typically • 2,800 Health Risk Assessments have been collected • 60% opt in rate as new clients to JFCS Integrated Health Program Data •Collaborative relationship with MIHS since August, 2010, a Federally Qualified Health Center look alike • 4 clinics across Maricopa County • 11 Health Navigators Integrated Health Client Demographics Ethnicity of all Clients at JFCS 2% 1% 10% 29% 58% Ango/White Hispanic/Latino African American Native American Other 1% Overall Gender Breakdown Female 46% Male 54% Children’s Population Girls 32% Boys 27% Children Only Age 0 -2 6% Age Demographics Age 14 – 17 30% Age 3 – 5 22% Age 0-2 Age 3-5 Age 6-13 Age 14-17 Age 6 – 13 42% Currently Serving 4,800 Children All Clients Age Demographics 1% 23% 4% 13% Age 0-2 Age 3-5 Age 6-13 9% 25% Age 14-17 Age 18-30 7% 18% Age 31-49 Age 50-64 Age 65 + Mental Health Diagnosis Analysis For Children 3% ADHD/ADD 4% Mood Disorder 10% 3% 2% 26% Other Neglect of Child Bipolar Disorder 7% Anxiety 13% Depression Adjustment Disorder 16% 16% Autism PTSD Medical Conditions Analysis for Children 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% 80% 7% 4% 2% 2% 1% 4% Behavioral Health Diagnosis Analysis for Adults Chronic Disease Analysis for Adults Integrated Health Objectives Objective 1: Assist behavioral health recipients in establishing/maintaining an ongoing, lasting relationship with a primary care provider. Objective 2: Facilitate improvements in the physical health of behavioral health recipients including EPSDT for children Objective 3: Improve the mental health of behavioral health recipients. Objective 4: Enable behavioral health recipients to increase control over their health. Objective 5: Improve collaboration between behavioral health and the client’s medical team through the use of a health information infrastructure that includes an electronic medical record and shared health information. PCP Relationship • Investigate families current relationship with Primary Care Physician (PCP) and other medical providers • Is client is satisfied with current PCP • Maricopa Integrated Health System • Assist client in changing PCP with AHCCCS • PCP Notification – auto faxed from EHR • Release of information with medical provider to share information • Assist client in scheduling first appointment with MIHS • Attend medical appointments with family as an advocate • Assist foster families in retrieving medical history Improving Physical Health • Explore families recent medical visits and history • Satisfaction with current PCP • Maricopa Integrated Health Systems • EPSDT for children • Nutrition Basics and for specific diagnoses • Transportation to appointments if needed • Compiling of medical records • Medical decision making • The importance of physical exercise • Improved coordination and collaboration between medical and behavioral health through HIE and other efforts Improving Mental Health Educating families on the importance of taking care of their physical health also improves their mental health and vice versa. • Working with the BH teams • The Bully Project • Nutrition for specific mental health diagnoses • Relaxation • Medication reconciliation • Tobacco education Client Quote on Integrated Care Services “I have been a patient at JFCS for several years now and have received exceptional care. My life has improved since I first came here and I am grateful. However, since I was first introduced to Integrated Health by my peer navigator, the care I receive has become much more meaningful. Not just the behavioral health care, the physical health care I receive has improved as well. I say this because Adrienne has enlightened me to the fact that physical and emotional well being are inter-connected and cannot improve if either is neglected.“ - Anonymous satisfaction survey comment Increased Control in Overall Health • • • • • • • • • • Teaching self management skills Health education Informed decision making skills Health literacy skills equips the entire family to improve ability to manage health Empowerment and assertiveness skills Nutrition, exercise, and self care Information Resources Social support development Family and child only exercise programs Flex funds for program related items, ie: karate Social Supports One of the most important components of human resiliency is social support. Research supports the importance of social supports in health outcomes. Relaxation and Stress Management Classes Quote from a enrolled client: “The relaxation class helps me to cope with my problems better and helps me think in a more positive way. I really enjoy coming and being a part of this two days a week. I feel like it is empowering me, making me stronger as a person, more positive, and healthier in my lifestyle. This is a wonderful program.” - SF, Adult Integrated Health Client Nearly 60-90% of visits to healthcare professionals are either caused or exacerbated by stress for adults. The Relaxation Response Research shows the Relaxation Response is an essential resiliency self-management skill that is as predictable as medication in immediately reversing the stress-induced flight-or-fight response. -Benson, H. The Relaxation Response, William Morton and Company, 1975 Let’s Do It! EMPOWERING CLIENTS Helping clients gain the knowledge, skills, and attitudes for coping with changes in lifestyle and circumstances • Learning to help themselves and their family members, manage their own care • Greater confidence in themselves • Increases clients and parents understanding of the medical system • Greater ability for the client to meet their own needs and/or the needs of their children • Gives clients knowledge that they can share with others Continuity of Care Document: A patient summary containing data of the most relevant administrative, demographic, and clinical information facts about a patient's healthcare, covering one or more healthcare encounters. It provides a means for one healthcare practitioner, system, or setting to view all of the pertinent data about a patient and forward it to another practitioner, system, or setting to support the continuity of care. Six Mandated CCD Data Elements: 1. Header/Document Identifying Information 2. Patient Identifying Information. 3. Patient’s Insurance and Financial Information. 4. Health Status of the Patient 5. Care Documentation includes some detail on the patient-clinician encounter history, such as the dates and times of recent and pertinent visits and the purposes of the visits and names of clinicians or providers 6. Care Plan Recommendation includes planned or scheduled tests, procedures or regimens of care. Health Information Exchange JFCS and MIHS Sharing client data between JFCS and MIHS on two fronts utilizing the current CCD standard: •JFCS can pull CCD from MIHS and bring in to EHR •JFCS can pull CCD from our EHR and fax over to MIHS for inclusion in their client record Health Risk Assessment Date completed: Printed Name Person completing form: Name: Date of Birth: Male ____ Parent/ guardian name providing info.: Female ___ Age: Contact phone number: Vital Signs: Are all immunizations up to date? Yes_____ Hei ght: Does your child/youth have any allergies: No_____ Wei ght: BMI: Does your child/youth have at least one friend he/she sees regularly? Yes ____ Bl ood Pressure (> 3 y.o.): Has your child/youth ever been the victim of bullying? Yes Pul se Rate: On average how much daily physical activity does child/youth get per week? Respi ratory Rate: 0 to 1 hours: _______ 1 to 2 hours: _______ Has your child/youth ever been to the dentist? Yes______ No ______ Has he/she seen a dentist in the last 6 months? Yes______ No ______ Are you aware of any unresolved dental issues (cavities, misalignment)? Date of last visit to primary care physician: ______ No____ No ______ 3+ hours: _______ Yes______ No ______ PCP name and phone number: Has a consent for records to include EPSDT form and laboratory tests been completed? If yes, date faxed to PCP office: Yes______ Have records been received from PCP? Did your child/youth have a different PCP before the one named above? Yes______ No ______ Yes______ No ______ No ______ If yes, previous PCP name and phone number: Has your child/youth had a visit to a medical ER or hospital in the past 6 months? Yes _______ No _______ Does your child/youth have any of the following chronic medical conditions: Asthma Yes______ No ______ Ski n Probl ems Yes______ No ______ Heart di sease Yes______ No ______ Di abetes Yes______ No ______ Eati ng Probl ems Yes______ No ______ Hi gh bl ood pressure Yes______ No ______ Sei zures Yes______ No ______ Sl eepi ng Probl ems Yes______ No ______ Heari ng Probl ems Yes______ No ______ Anemi a Yes______ No ______ Obesi ty Yes______ No ______ Speech Probl ems Yes______ No ______ List all current medications that your child/youth takes: Name of Medi cati on Dose Frequency Has your child/youth ever had blood work done? Yes ______ No ______ If yes, were any results abnormal? Yes ______ No ______ Which ones were you told were abnormal? Significant life events: To be completed by BHMP Chi l d Protecti ve Servi ces i nvol vement Yes______ No ______ HDL: Legal system i nvol vement Yes______ No ______ LDL: Death of fami l y or fri end Yes______ No ______ Total chol esterol : Di ffi cul ti es i n school Yes______ Willingness to Participate: In the next si x months woul d you parti ci pate i n a program that woul d Yes______ hel p you i mprove your overal l If avai l abl e, woul d you l i ke fol l owup servi ces and i nformati on to Yes______ i mprove Concerns you have about child's/youth's health: No ______ Tri gl yceri des: Fasti ng gl ucose: No ______ No ______ Ye s Le ve l no Reporting HRA Report HRA Comparison Report Integrated Health Update Report Client Caseload Tracker Report Daily staff productivity reports Billed services and unit reports Appointments kept, no billing has occurred Outcomes PCP Relationship Outcomes and Baseline: • We have assisted 66% of clients needing a better relationship with their PCP • 75% of surveyed clients reported IH Program helped them develop better PCP relationship • 86% of surveyed clients reported better coordination of care amongst health providers Improved Physical Health: • We have delivered resources and information regarding health and wellness to 80% of our clients in the IH program • 39% of clients needing screening or routine testing received it • 55% Of clients walking in with untreated chronic medical disease, received medical appointment within 45 days of beginning the program • 33% of clients that reported not managing their diabetes are now successfully managing it and have reduced their A1C levels to below 9% • 77% of surveyed clients report they feel an improvement in overall physical health Outcomes PCP Relationship Outcomes and Baseline: • We have assisted 66% of clients needing a better relationship with their PCP • 75% of surveyed clients reported IH Program helped them develop better PCP relationship • 86% of surveyed clients reported better coordination of care amongst health providers Improved Physical Health: • We have delivered resources and information regarding health and wellness to 80% of our clients in the IH program • 39% of clients needing screening or routine testing received it • 55% Of clients walking in with untreated chronic medical disease, received medical appointment within 45 days of beginning the program • 33% of clients that reported not managing their diabetes are now successfully managing it and have reduced their A1C levels to below 9% • 77% of surveyed clients report they feel an improvement in overall physical health Technology Landscape HITECH Act Office of the National Coordinator (ONC) EHR Interoperability: Data Set Selection Electronic Health Records (EHR): Certification Meaningful Use – Incentives Privacy: HIPAA and 42 CFR Part 2 Heath Information Exchange: State Grants $16 M Hospital Lab Specialist HIE PCP Pharmacy HIE Benefits Connects multiple organizations with data Coordinates care through information exchange Shares information real time and efficiently Improves quality and costs of services Avoiding duplication of tests Improved decision making based on data availability Improved experience for the individual: safety impact HIE Data Items Demographics Diagnosis Allergies Prescribed Medications Lab Results **Documents: Progress Notes, Treatment and Crisis Plans, Summaries Community Education State Adoption and Use Varies Behavioral Health: Nebraska and AZ Medical Provider Use – Who is Using an HIE? Informed Consent Opt In – Must opt-out, in HIE by default Opt Out – Must opt – in, out of HIE by default Education Strategies Marketing Campaign Education of Health Care Professionals Education of Heath Care Recipients Medical v. Behavioral Health Differences Arizona Lessons Learned Input from Audience Patient Portal Psych Pharmacy Hospital BHINAZ HIE Crisis Provider OP BH Clinic ER Resources http://www.healthit.gov HIE Grants by State Programs and Advisory Committees Patient and Families Information