Genetics in Primary
Care
Dr. Jude Hayward
GPwSI in Genetics, Bradford
The Genetics Explosion
30 articles in the BMJ in the last 3 months
65 articles in the Guardian in the last 3 months
Range of issues:
Genes
for common diseases e.g. ‘The Fat Gene’
PIGD
GM
crops
Forensic DNA database
HFEA bill – human / animal hybrids
What does Genetics mean to you?
Tricky
Dry
Highly Specialised – sometimes the
patients know more than you do
Interesting challenge
Hard to explain to patients
What does ‘genetics’ mean to you?
Craniofaciocutaneous Syndrome
Mental retardation
ASD / HOCM
Icthyosis
Sparse Hair
High Forehead
Prominent ears
Depressed nasal bridge
What would you like
to know?
Family History – why do we do it?
Think of the patient you most recently
asked for a family history – what was the
situation / presenting problem?
What did you do with that information?
Family History – why do we do it?
To aid with accurate risk assessment - likelihood
of developing a certain disease
To identify those who have an underlying
genetic condition who would benefit from further
information and services
To identify other members of the family who may
be at risk – affected / carrier
This leads to appropriate management
strategies
Objectives for today’s session
To outline the scope of genetics in primary care
To identify some useful guidelines and resources for
clinicians
To identify useful resources for patients
To outline the structure of services providing care to
patients with genetic issues
To touch on common forms of inheritance
To discuss some common presentations of patients with
genetic issues
To encourage ‘thinking Genetics’ where you might not
have done before!
Scope of Genetics in Primary Care
10% of consultations have genetic aspect
Mostly multifactorial disease with genetic
component e.g. CHD, asthma, Alzheimers,
diabetes
Single gene disorders e.g. CF, Huntingdon’s,
(Pharmacogenetics)
Reproductive issues e.g. Hbopathies
Multifactorial Inheritance
Increased risk due
to family history
Environmental factors
‘nurture’
Genetic
Condition
Genetic Factors
‘nature’
Role of Primary Health Care Team
(RCGP)
General Practitioners have a key role in
identifying patients and families who would
benefit from being referred to appropriate
specialist genetic services
Management and support of families with /
at risk of genetic conditions
Consideration of FH in multi-factorial
disease e.g. cancer, DM, CHD
A typical morning
surgery…
A ‘typical’ morning surgery…
Mrs. B, aged 52, attends for a blood pressure
check as she has had 2 raised readings over the
last few months.
Today it is 152 / 96. She says she’s not
surprised it is raised as she has just heard that
her sister has been diagnosed with ovarian
cancer – this has come as a shock as she has
been supporting her other sister through a
course of chemotherapy for breast cancer.
What else would you ask?
Cancer is common
1 in 3
Of the general population will develop cancer
during their lifetime
Breast cancer: 1 in 9 women
Ovarian cancer: 1 in 35 women
Bowel cancer: 1 in 18 men, 1 in 20 women
Incidence increases with age (risk factor)
Multifactorial Inheritance
Increased risk due
to family history
Environmental factors
‘nurture’
Genetic
Condition
Genetic Factors
‘nature’
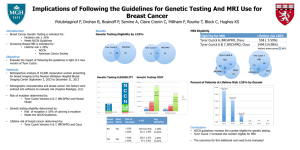
Hereditary Cancer Syndromes
1 in 20 cases of breast, ovarian, CRC cancer are
hereditary.
Breast/ovarian cancer syndromes: BRCA 1 + 2
Ass. cancers: Male Breast Cancer, Prostate Cancer, Certain
melanomas, association with CML / renal cell carcinoma
Colorectal cancer syndromes: FAP / HNPCC
HNPCC associated cancers: ovarian, endometrial, gastric,
biliary, urinary tract
Autosomal Dominant Inheritance
Risk assessment
40-50 patients age 35-64 per 2000 patients in GP have 1
first degree relative with CR, breast, ovarian or uterine
cancer (UK)
Familial Cancer: Primary Care Management of patients
at risk of breast, ovarian or colorectal cancer
Based on NICE and BSG guidelines
OPERA – tool for patients via MacMillan website
Useful information to include in
referral:
Name , DOB, address, NHS number,
(telephone number)
Whatever family history available
Pedigree number / Name(s) of affected
family members if seen by any genetics
team
(Pregnant or non-pregnant)
Genetic Services
Yorkshire Regional Genetic Service
(based at LGI: switchboard 0113 243 2799)
Other specialties: Paediatrics, Midwives
Other services:
Medical Staff: Consultants, Registrars
Genetic Counsellors
Family History Administrators
DNA / Cytology labs
Haemoglobinopathy and Sickle Cell Service
GPwSI in Genetics
What happens when a referral is
made?
Referral received (can be via secondary care)
Questionnaire sent out by family history
administrators and returned by pt
Consultants review referral and FH
Triage to Genetic Counsellor / Consultant
Genetic Counselling (Peter Rose)
Information gathering:
Information provision:
Discuss family history
Identify patient concerns / wishes
Explain risks and genetic contribution
Discuss screening if appropriate
Preventative measures
Discuss tests if appropriate
Decision making:
Guide patient through difficult choices
Instigate management which patient chooses
Genetic Counselling
IS NON-DIRECTIVE
Doesn’t always result in a test!
‘Genetic Counselling is the process by which patients or
relatives at risk of a disorder which may be hereditary
are advised of the consequences of the disorder, the
probability of developing or transmitting it and the ways
in which this may be prevented or avoided’
Familial / hereditary cancer
Family History is used to assess risk
Population risk:
should
be reassured and managed in Primary Care
Moderate / high risk (i.e. above population risk):
Additional
screening (mammogram +/- MRI)
Risk-reducing surgery i.e. prophylactic mastectomy /
oophorectomy
High risk:
may
be offered testing for a particular syndrome
‘Typical’ patient no. 1 – Mrs. B
Could / Should be offered referral to Genetics
High risk for breast and ovarian cancer
Offered screening:
Offered risk-reducing measures:
Yearly Mammogram +/- MRI from 35-50
18 monthly mammogram from 50 onwards
Ovarian screening via research study
Prophylactic Bilateral Mastectomy
Prophylactic Bilateral Oophorectomy
Offered testing:
Given information and testing discussed
A ‘typical’ morning surgery…
Mrs T. attends, and after telling you about her athlete’s
foot she bursts into tears and tells you her mother has
just been diagnosed with cancer – ‘everyone in the
family has it and I’m bound to get it’
What else do you ask?
She tells you:
Mother had breast cancer aged 64
Sister had cervical cancer in her 30’s
Her grandfather had prostate cancer and died in his 80’s
Her uncle developed lung cancer in his 60’s – he had been a
heavy smoker all his life
Role of Primary Care (NICE 2006)
Women at or near population risk should
be cared for in Primary Care
They should receive standard information
(see box in PACE Guidelines)
‘Be Breast Aware’ (NHS Breast Screening
Programme and Cancer Research UK)
‘Are you worried about Breast Cancer?’
(www.macmillan.org.uk/cancerinformation)
Communication…
How would you try to reassure her that she
wasn’t at any greater risk than the rest of
the population?
Aled
Maud
CRC@58
Sian
Huw
Browyn
CRC@57
CRC@54
50
Aled
Olwen
Dai
Wynn
Tom
37
34
34
33
29
John
Died young
?renal Ca
Margaret
Renal Ca@42
Jenny
40
Jane
20
Julian
18
John
38
Becky
16
Lily
13
Roy
Renal Ca@50
Richard
35
Mark
33
Pat
58
Judith
30
28
Other resources for patients
www.macmillan.org.uk/cancerinformation
0808 808 0000
www.cancerhelp.org.uk
www.cctrust.org.uk
020 7704 1137
http://www.macmillan.org.uk/Get_Support/
Cancer_types/Genetic_risk_factors.aspx
Can access OPERA via macmillan
website
The story so far…
Our job is to identify the 1 in 20 patients
with cancer (and their relatives) with a
genetic basis (those in the red blob)
PACE guidelines can help
Only some patients will be offered a
genetic test – management is mainly
information giving, extra screening, riskreducing surgery.
A typical morning
surgery…
When to think about it:
A 34-year-old lady with a history of
depression comes to see you. Her sister
died very suddenly 2 weeks ago at the age
of 42.
She also happens to be your patient, and
when you look in her notes, the cause of
death from PM is Myocardial Infarction
Familial Hypercholesterolaemia
1 in 500 people have Familial
Hypercholesterolaemia
50% CVD risk by the age of 50 in men
30% CVD risk by the age of 60 in women
110,000 cases in the U.K.
Only around 10,000 identified so far
Hot Topic at present…
NICE guidelines:
Familial Hypercholesterolaemia
(August 2008)
When to think about it: Simon
Broome Diagnostic Criteria
TC >7.5, LDL >4.9 AND
Definite FH:
Tendon
xanthomas in 1st or 2nd degree relative
Possible FH:
Family
history of IHD <60 y.o.a. in 1st degree relative,
and <50 y.o.a. in 2nd degree relative
Family history of TC >7.5 in 1st or 2nd degree relative
Cholesterol deposition in patients heterozygous for familial hypercholesterolemia.
(a, b) Tendon xanthomata, and (c) corneal arcus.
Fig. Disease box 11 ©Scion Publishing
Ltd
Photos courtesy of Dr Paul Durrington.
DO NOT USE THESE!
How to manage it:
Manage other risk factors
Aggressively control cholesterol to lower LDL
<50% level at initial measurement
If not controlled with 2 agents, refer:
Donald
Whitelaw (Diabetes and Endocrinology
Consultant, BRI)
Julian Barth / Mike Mansfield (Lipid clinic, LGI)
Assess for symptoms of IHD
What about the Genetics?
Autosomal Dominantly Inherited
Mutation in LDL receptor gene
Individuals should be referred for
genotyping and cascade screening
Resources and Services in response to
NICE……………provision variable, and
cascade screening often not in place
What about the rest of the family?
‘Cascade Screening’ of all 1st and 2nd
degree relatives – several pilot projects
underway to figure out how to do this.
Controversies:
How
do you assess for possible IHD?
Children should be started on a statin as early
as possible, around the age of 10
The story so far…
If someone has a family history of
premature heart disease
or presents with a cholesterol over 7.5:
Think Familial Hypercholesterolaemia
Other inherited cardiac conditions
Specialist clinic at LGI
FH of sudden cardiac death
FH of arrythmia, cardiomyopathy or
connective tissue disease
Can refer directly
Any queries: Kath Ashcroft
0113
3925784 or mobile 07789003997
A typical morning
surgery…
A ‘typical’ morning surgery…
A 36-year-old man comes in ‘tired all the
time’. He has several non-specific
symptoms including palpitations and
general aches, and you are aware he is
having a stressful time at work.
He is concerned, and asks you to do some
blood tests.
Hereditary haemochromatosis
High index of suspicion in younger men who present TATT.
Autosomal recessive disorders, carrier rate 1/8 – 1/10,
prevalence 1/200 – 1/400.
Signs, Symptoms and Complications:
Non-specific – tatt, joint pain, weight loss, (impotence)
Liver disease
Diabetes
Hypogonadotrophic hypognadism
Arthritis
Cardiac Disease (heart failure)
Venesection improves life expectancy - normal if before
development of diabetes and liver cirrhosis
Hereditary haemochromatosis
His ferritin came back as 458. What would
you do next?
Diagnosis:
Ferritin:
will be raised once iron overload occurring.
Can also be raised in acute phase response
If ferritin high, or high index of suspicion consider
checking Fasting Transferrin (earliest marker of HH)
If transferrin > 45%, refer to haematologist
Generally, females >50%, males >55%
Hereditary Haemochromatosis
Genetics:
2
mutations responsible for >95% in U.K.
Many people who inherit the mutations will not
develop clinical disease.
Genetics dept will offer gene testing /
genotyping to 1st degree relatives only.
Other examples!
A 24-year-old man who is diagnosed with
Type 2 Diabetes. He has a normal BMI, is
caucasian, and has no family history.
A 59-year-old man who is caring for his
wife who has just been diagnosed at 57
with early onset Alzheimer’s. Her mother
also had dementia of some sort.
A typical morning
surgery…
Recessive Inheritance
Parents
Carrier
Carrier
Sperm &
eggs
Offspring
Normal
Carrier
Carrier
Affected
Autosomal Recessive Inheritance
– Affects one generation
– Both sexes affected
– Male – male
transmission
National Screening Committee
Timeline
Other conditions…
Any children elsewhere in the family with
difficulties?
For instance hearing or visual impairment?
Problems at school, or have regular outpatient appointments?
Recurrent miscarriage or stillbirth.
Resources for patients
www.cafamily.org.uk
Support
for families in which there is a rare
genetic disorder
This is the slide to remember!
Our role is identify patients at risk or who may have a
genetic condition and would benefit from input from
Genetic Services
We do this by taking and using a family history – core
examples:
A common multifactorial disease (e.g. IHD or cancer) occurring
young, strong family history, atypical presentation
Early pregnancy, or even pre-conceptually
There is lots of information out there regarding individual
conditions
Supporting Genetics Education for Health
www.geneticseducation.nhs.uk
Supporting Genetics Education for Health
www.geneticseducation.nhs.uk
Resources:
Me! judith.hayward@bradford.nhs.uk
YGS via LGI switchboard: 0113 243 2799
www.gpnotebook.com
www.geneticseducation.nhs.uk
‘Recognising the common patterns of
inheritance in families’
www.library.nhs.uk/genepool
www.chime.ucl.ac.uk (apogi sheets
Thank you!
Any questions?
Pedigree Symbols
Male
Marriage / Partnership
(horizontal line)
Female
/
Partnership that has
ended
Person whose sex is
unknown
P
Offspring (vertical line)
Pregnancy
Miscarriage
X weeks
Affected Male & Female
Carrier Male & Female
Supporting Genetics Education for Health
www.geneticseducation.nhs.uk
Parents and Siblings
Family History
Jane (28) is 6 weeks pregnant
Jane’s husband Christopher (29) is an only child
His parents William (60) and Margaret (59) are alive
and well
Jane has one brother John (34), he had one son
David (10) to his first wife Alice (33). Their marriage
ended in divorce
John’s second wife Christine (29) had a miscarriage at
9 weeks and a son Richard (4) who has CF
Jane’s father George Whitehead died at the age of 66
Jane’s mother Joan (64) is alive and well
Supporting Genetics Education for Health
www.geneticseducation.nhs.uk
Joan
William Hobson
60
Margaret George Whitehead
Died age 66
59
Christopher Hobson
29
Jane
28
Joan
64
Alice
33
John Whitehead
34
P
6 weeks
Christine
29
9 weeks
David
10
Assume Jane was tested and found to be a carrier.
Richard
4
Cystic fibrosis
What is the probability that the baby in Jane and Christopher
Hobson’s current pregnancy will have cystic fibrosis?
(Population risk of being
CF carrier for people with North European
Supporting Genetics Education for Health
www.geneticseducation.nhs.uk
ancestry = 1 in 25)