Prevention in practice – an initiative between BASCD and
advertisement
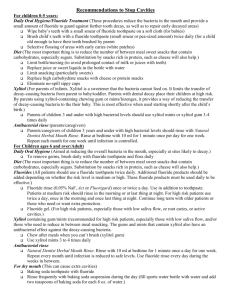
Prevention in practice – an initiative between BASCD and Department of Health Sue Gregory Consultant in Dental Public Health The task • DH want to focus on prevention - How can prevention be built into the new contract? • What help can be given to PCTs to help them commission more effectively? • Can we maximise the yield from the preventive tools we have and the knowledge on how they work? Following the publication of Choosing Better Oral Health 3 supporting documents: • ‘Smokefree and Smiling’ - Guidance to PCTs on smoking cessation and how it fits in with dental practice – Richard Watts, May 2007 • Guidance on improving oral health among adults and children with disabilities – Colette Bridgman, to be launched soon • ‘Delivering Better Oral Health’ - Provision of evidence-based information to support the commissioning of preventive services – Sue Gregory, Sept 2007 September 2007 Contents 1. 2. Reference cards - Summary guidance Supporting chapters: • • • • • • • • • Principles of toothbrushing for oral health Increasing fluoride availability Healthy eating advice Identifying sugar-free medicines Improving periodontal health Stop smoking guidance Accessing alcohol misuse support Prevention of erosion Supporting references Distribution • • • • General practices Salaried services Consultants in Dental Public Health Also available online Development of ‘Delivering Better Oral Health’ The Team • • • • • • • • • • • • Chair – Sue Gregory (BASCD president) Secretary – Semina Makhani Derek Richards (BASCD) Gill Davies (BASCD) Keith Milsom (National Oral Health Unit) Rowena Pennycate (BDA) Baldeesh Chana (FGDP) Nigel Carter (BDHF) Richard Watt (OHPRG) Tom Dyer (GDP) Tony Jenner / Jerry Read (DH) Rosemary Khan, Jan Clarkson The Principles • Statements must be supported by evidence – the stronger the better • The potential benefits of prevention have not been maximised – Not doing enough – Prevention not evidence based • Challenges the ‘high risk’ approach in favour of a practice ‘population’ approach The Principles • Messages would be in line with wider health messages – The common risk factor approach • Providing information for – The whole dental team – Dental care at primary, secondary and tertiary level – Primary Care Organisations to assist with commissioning The outputs Grade Strength of evidence I Strong evidence from at least one systematic review of multiple well-designed randomised control trials e.g Cochrane reviews. II Strong evidence from at least one properly designed randomised control trial of appropriate size e.g. comparison of 2 toothpastes. III Evidence from well-designed trials without randomisation, single group pre-post, cohort, time series of matched case-control studies e.g. plaque reduction studies. IV Evidence from well-designed non-experimental studies from more than one centre or research group. V Opinions of respected authorities, based on clinical evidence, descriptive studies or reports of expert committees. Prevention of caries in children age 0 – 6 years Advice to be given Children aged up to 3 yrs All children aged 3-6 yrs Children giving concern; E.g those likely to develop caries, those with special needs EB •Breast feeding is best for babies From 6 months of age infants should be introduced to drinking from a cup, and from age one year feeding from a bottle should be discouraged Sugar should not be added to weaning foods Parents should brush / supervise toothbrushing Use only a smear of toothpaste containing no less than 1000 ppm fluoride As soon as teeth erupt in the mouth brush them twice daily I III Brush last thing at night and on one other occasion, Brushing should be supervised by an adult Use a pea size amount of toothpaste containing 1350-1500 ppm fluoride Spit out after brushing and do not rinse The frequency and amount of sugary food and drinks should be reduced and, when consumed, limited to mealtimes. Sugars should not be consumed more than four times per day Sugar free medicines should be recommended I V V, I All advice as above plus: Use a smear or pea size amount of toothpaste containing 1350-1500 ppm fluoride Ensure medication is sugar free Advise that dietary supplements containing sugar and glucose polymers are given at mealtimes when possible and not last thing at night Professional intervention EB Apply fluoride varnish to teeth twice yearly (2.2% F-) I Apply fluoride varnish to teeth 3-4 times yearly (2.2% F-) Prescribe fluoride supplement and advise re maximising benefit Reduce recall interval Investigate diet and assist to adopt good dietary practice Ensure medication is sugar free or given to minimise cariogenic effect V V V I IV IV III I V V II V III V Prevention of caries in children aged from 7 years and young adults All children and young adults Those giving concern – E.g. those likely to develop caries, those undergoing orthodontic treatment and those with special needs Advice EB Professional intervention Brush twice daily I • Brush last thing at night and on one other occasion V Apply fluoride varnish to teeth twice yearly (2.2% F-) • Use fluoridated toothpaste (1350 ppm F or above) I • Spit out after brushing and do not rinse IV • The frequency and amount of sugary food and drinks should be reduced and, when consumed, limited to mealtimes. Sugars should not be consumed more than four times per day III Fissure seal permanent molars with resin sealant Apply fluoride varnish to teeth 3-4 times yearly (2.2% F-) For those 8+ years with active caries prescribe daily fluoride rinse For those 10+ years with active caries prescribe 2800 ppm toothpaste For those 16+ years with active disease consider prescription of 5000 ppm toothpaste Investigation of diet and assistance to adopt good dietary practice All the above, plus : Use a fluoride mouth rinse daily (0.05% NaF) at a different time to brushing I EB I I I I I I III Prevention of caries in adults All adult patients Those giving concern – E.g. those with current active caries, exposed roots, dry mouth, other predisposing factors, those with special needs Advice EB Brush twice daily with fluoridated toothpaste I Use fluoridated toothpaste with at least 1350 ppm F- I Brush last thing at night and on one other occasion V Spit out after brushing and do not rinse IV The frequency and amount of sugary food and drinks should be reduced and, when consumed, limited to mealtimes. Sugars should not be consumed more than four times per day III All the above, plus : Use a fluoride mouth rinse daily (0.05% NaF) at a different time to brushing I Professional intervention EB I Apply fluoride varnish to teeth twice yearly (2.2% F-) For those with active caries prescribe daily fluoride rinse For those with active disease prescription of 2800 or 5000 ppm toothpaste Investigation of diet and assistance to adopt good dietary practice I II II III Prevention of periodontal disease – to be used in addition to caries prevention Risk level Advice EB Professional intervention All adolescents and adults V Demonstrate methods of improving plaque control V - manual brush with a small head and round end filaments, a compact angled arrangement of long and short filaments and a comfortable handle OR - a powered toothbrush with an oscillating/ rotating head V V III Investigate possible improved control of predisposing systemic conditions Take a history of tobacco use, give brief advice to users and signpost to local Stop Smoking Service Investigate diet and assistance to adopt good dietary practice Brush teeth systematically twice daily with either a Do not smoke I Use toothpastes containing triclosan with copolymer or triclosan with zinc citrate to improve levels of plaque control I I Clean inter-dentally using inter-dental brushes or floss V Eat a well balanced diet V EB V V Prevention of oral cancer Risk level Advice EB Professional intervention All adolescents and adults Do not smoke Do not use smokeless tobacco E.g. Paan, chewing tobacco, gutkha III III Take a history of tobacco use, give brief advice to users and signpost to local Stop Smoking Service Reduce alcohol consumption to moderate (recommended) levels IV III Signpost to local Alcohol Misuse Support Services Maintain good dietary practice in line with Balance for Good Health Increase fruit and vegetable intake to at least 5 portions per day V III EB V Erosion • Currently the evidence is based upon laboratory studies or observational studies. No evidence could be found which measured the effectiveness of providing preventive advice in a clinical setting. • Until such evidence emerges guidance will be provided in the Appendix 8 in the Supporting Information With acknowledgement of the original work carried out by: Mrs J T Duxbury Miss M A Catleugh Prof R M Davies Dr G M Davies Brand ppm fluoride Crest Range – (Freshmint, mildmint, tartar control,) 5Complete 1450 Colgate – Sensitive – Fresh stripe, whitening 1450 ASDA range – Total care, Sensitive, whitening 1450 Boots’ Sensitive 1450 Pearl Drops – Daily whitening 1300 Aquafresh multi-action whitening 1100 Oral B Stages 1100 Tesco’s Daily care range 1090 Mentadent P 1000 Morrison’s Kids – Strawberry and milk teeth 1000 Boots’ Smile 500 Crest milk teeth 250 Sensodyne original None Boots fluoride free None Mu’min Halal Health and Beauty None Commissioning Implications • Fluoride varnish costs 30 pence per application • 3 x per year, yields 3 UDAs • Skill mix (hygienists & therapists) • Effective Prevention better than Cure Thank you