File 1
advertisement

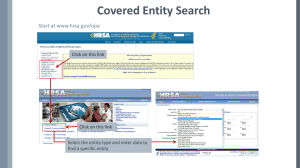
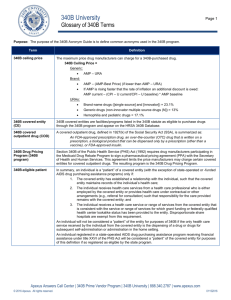
Optimizing The 340B Program Promoting Integrity, Access, & Value To deliver clinically and cost-effective pharmacy services This educational product created by: Health Resources and Services Administration | Office of Pharmacy Affairs 340B Peer-to-Peer Program 340B Program Integrity The Medicaid Exclusion File and Avoiding Duplicate Discounts Purpose of Activity The purpose of this module is to explain the purpose of the Medicaid Exclusion File and provide strategies on how states and covered entities can avoid duplicate discounts. Topic Guide Describe the role of the Medicaid Exclusion File in preventing duplicate discounts Describe situations in which a duplicate discount might occur in error Identify the data entities provide for insertion in the Medicaid Exclusion File Explore how to use the Medicaid Exclusion File 340B Background Established in 1992 statute (section 340B of the Public Health Service Act) Requires manufacturers to sell “covered outpatient drugs” to certain “covered entities (CEs)” at greatly reduced price Includes 2 major prohibitions: • Diversion to non340B patients • Duplicate discounting Requires mechanism t ensure that entities comply with duplicate discount prohibition Duplicate Discount on 340B Drugs When does a duplicate discount occur? When the same drug is: Purchased with an up-front 340B discount And Credited with a back-end transaction Medicaid rebate Examples of Duplicate Discounts Example 1: Take-home prescription Example 2: Provideradministered • Patient receives 340B medication (prescription from outpatient procedure) • Medication is billed through the pharmacy’s billing system • National Drug Code (NDC) level data are transmitted to state Medicaid agency • Medicaid agency submits NDC claim information to manufacturer for rebate • Patient is administered medication (by outpatient procedure provider) • Medication is billed through hospital or clinic billing system • NDC level data are transmitted to state Medicaid agency through billing system • Medicaid submits NDC level claim for manufacturer rebate Examples of Duplicate Discounts (Cont’d) • Patient of Medicaid managed care organization (MCO) fills outpatient prescription at 340B pharmacy • MCO submits NDC level data from pharmacy claims to Medicaid agency Example 3: Managed Care • Medicaid agency submits data from these claims to Affordable manufacturers for rebates Care Act MCO 340B Exemption 1. • Section 2501(c) amends section 1927(j)(1): “… certain covered outpatient drugs in this section are not subject to the rebate requirements … [if] subject to discounts under section 340B of the Public Health Service Act.”1 CMS. Letter re: medication prescription drug rebates. April 22, 2010. Available at: www.ncsl.org/documents/health/42210PPACADrug_Rebate_SMD.pdf. Accessed November 22, 2011. Medicaid Exclusion File Congress 340B Legislation Department of Health and Human Services DRUG-PRICING PROGRAM Must Create Mechanism Purchasing Drugs for Medicaid Patients 340B entities may: purchase drugs at 340B prices OR purchase drugs at non-340B prices (“off contract”) using a separate account The Medicaid Exclusion File Health Resources and Services Administration Office of Pharmacy Affairs Maintains Medicaid Exclusion File 340B Entities & Their Associated Medicaid Provider Numbers National Provider Identifies (NPI) Criteria for Listing in Medicaid Exclusion File Condition 1: Purchase drugs at the 340B price Condition 2: Transmission of NDC level data to state Medicaid office If both conditions are met, Medicaid provider number and NPI must be listed in Medicaid Exclusion File Billing Medicaid 340B entities must decide whether or not to use 340B drugs for Medicaid patients YES, use 340B drugs for Medicaid NO, don’t use 340B drugs for Medicaid 340B entities must decide how to bill Medicaid in a way that is consistent with their state’s Medicaid program All-inclusive Rate Managed Care Medicaid Traditional Fee-forService Medicaid Medicaid Exclusion File & 340B Contract Pharmacies 340B Entity Bill to Drugs Medicaid prescriptions filled using the contract pharmacy’s own non340B inventory No need to list pharmacy’s Medicaid number in OPA database Ship to Contract Pharmacy Entity’s 340B-purchased drugs are not used to fill Medicaid prescriptions 340B Enrollment Form Where should CEs indicate the required Medicaid billing information? A 340B covered entity is required to indicate on the 340B Enrollment Form if it intends to bill Medicaid for Drugs purchased at 340B prices. http://opanet.hrsa.gov/opa/CERegister.aspx