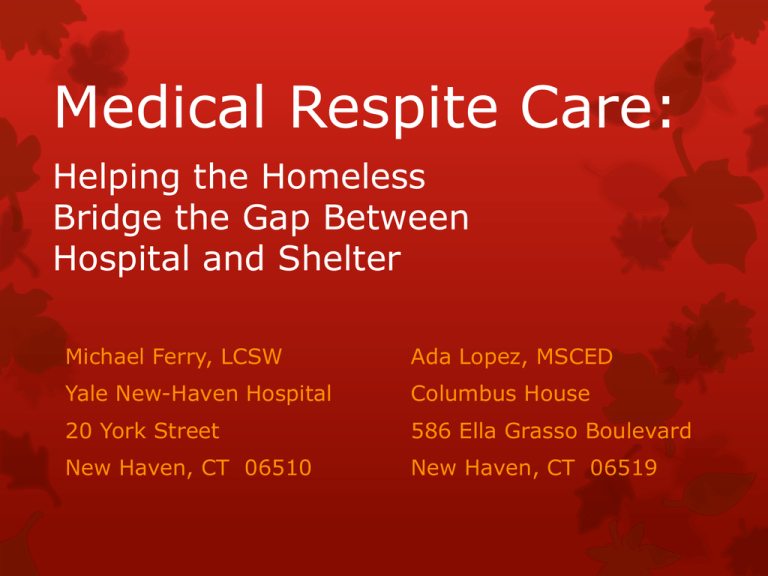
Medical Respite Care:
Helping the Homeless
Bridge the Gap Between
Hospital and Shelter
Michael Ferry, LCSW
Ada Lopez, MSCED
Yale New-Haven Hospital
Columbus House
20 York Street
586 Ella Grasso Boulevard
New Haven, CT 06510
New Haven, CT 06519
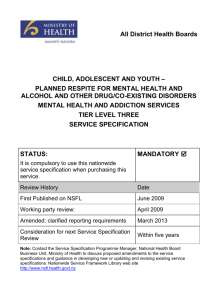
Defining Homelessness:
Homelessness includes those who are
Staying at a shelter
Staying on the streets, outside, or some
other place not meant for habituation
Doubled up with friends or family, or
temporarily staying in a motel/hotel AND
are unable to return or secure alternate
arrangements
Includes both chronic and transitional lack
of housing
Homelessness in New Haven
Homeless in New Haven: 700 people on average
Robert Woods Johnson study by Kelly Doran, MD
Statistics from a sample of 113 homeless individuals:
Age (mean): 49 years
Sex: 73% male, 27% female
Insurance: 75% Medicaid
Substance abuse history
Figures provided by Kelly Doran, M.D.
Entrance to Yale-New Haven Hospital
Readmission Rates
Of the homeless patients that were
hospitalized:
53.8% were readmitted within 30 days
Of these readmitted patients:
54% were readmitted within 1 week
75% were readmitted within 2 weeks
The collective population of Medicaid patients (which
includes the homeless) during this same period had a
30-day readmission rate of 18.7%
Figures provided by Kelly Doran, M.D.
Timing of Readmission
54% within 1 week
75% within 2 weeks
Days to Readmission
Figures provided by Kelly Doran, M.D.
Medical Respite Programs
A literature review found that they:
Improve care delivery and health
outcomes
Decrease future Emergency Department
visits and inpatient hospitalizations
Decrease length of stay and costs
Allow for the opportunity to connect
patients with supportive housing and
other services to break the cycle of
homelessness
Information provided by Kelly Doran, M.D.
Description of the Medical Respite
Program at Columbus House Shelter
Location: Third floor of Columbus House
Number of Beds: 12
Funding: Pilot grant from the State of
Connecticut
Length of stay: Projected to average 21
days, but stays permitted up to 30 days
Referrals: From YNHH inpatient and
observation units
Staffing: 24-hour supervisory staff,
Visiting nursing for medical care
Entrance to Columbus House
Learning a Hospital Patient has
been Identified as Homeless
Self-disclosure
Consultation by Medical Staff
Review of Documentation:
Address and phone fields
Physician Diagnoses
Nursing Evaluations
Social Work evaluations
Eliciting Circumstances of
Homelessness
“During the past two months, have you been living in
reliable housing that you own, rent, or stay in as part of
a household?”
If yes, “Are you worried that in the next two months
you may not have reliable housing?”
If no, “Where have you lived for most of the past two
months?”
“Are you able to return and stay there following
discharge?”
If yes, “Are you able to receive a visiting nurse
there?”
If no, will this patient have a post-discharge medical
need requiring respite?
Approaching Discharge
Staff identify an expected post-discharge
medical need requiring skilled nursing.
The care manager verifies that the patient
meets eligibility criteria for the Respite
Program.
The social worker assesses the patient,
introduces the idea of Medical Respite,
and obtains approval for a Columbus
House patient navigator to interview them
via a signed release of information.
Medical Eligibility for Respite Care
Requires skilled care, such as that provided by a
visiting nurse, but not so much as to need a stay in
rehab or hospice
Are independent with their ADLs
Transfers & ambulates independently, or using
mechanical assistance such as wheelchair, crutches or
cane
Are continent of bowel and bladder
Do not require IV hydration. IV treatment is acceptable
Are free from influenza or tuberculosis
Medical issue is reasonably expected to resolve in 30
days or less
Psycho-Social Eligibility for
Respite Care
Lack suitable housing
Are alert, oriented, and psychiatrically stable enough
to receive care and not interrupt the care of others
Are cognitively able and willing to comply with
treatment requirements, visiting nurses, shelter case
managers, etc.
Are willing to remain substance-free during their stay
If detoxified during their hospital stay, they must be
free of symptoms for at least 48 hours
Methadone patients are permitted
Medical Respite Care Brochure
.
Evaluation and Transfer Process
The patient is interviewed by the Patient
Navigator
Upon approval for Medical Respite, the care
manager submits referrals to a local medical
clinic (or other designated medical provider)
and a home nursing agency.
A detailed discharge checklist is used to
minimize complications afterward
Upon discharge, Columbus House staff escorts
the patient from the hospital to the shelter.
Typical Concerns Before/After Discharge
Patients are sometimes discharged without all necessary
prescriptions/wound care/diabetic supplies
Patients may not have active prescription coverage with which to fill
or refill their prescriptions
Prior medications being continued may not be verified as within the
possession of the patient
The patient may not not have the resources to secure non-covered
or over-the-counter medications
The new and/or ongoing medications may not being prescribed in
sufficient quantity to last until the patient’s next appointment
Patients are sometimes discharged without a named doctor,
occasionally only a clinic, and sometimes only a follow-up
appointment with a specialist
Prescriptions for Medical Respite patients are sometimes sent to
pharmacies other than our Apothecary, sometimes creating
delivery/procurement issues
Patients are sometimes discharged without established medical
appointments, and are instead being told to make their own
appointments
The patient’s primary care physician sometimes cannot be
contacted, or is unwilling to prescribe prior to an initial appointment
Discharge Checklist
Respite Patient’s Room
Continued Care
Weekly Case Review meetings which include
Social workers, case managers, and pharmacy from
Yale-New Haven Hospital,
Staff from the Medical Respite Care program, and
Staff from local clinics and home nursing agencies
Patient care, safety, and transitions to additional
services are discussed
Ongoing exchange and tracking of information
regarding the identification, progress, and
outcome of patients.
Ongoing steering committee meetings address
systemic issues impacting the program and
patient care
Preliminary Data
From October 7 to April 30:
493 patients were identified as homeless
and screened (includes repeat patients)
The above screenings resulted in 321
unique patients
Average Age = 48.6 Years
Sex
Race
Preliminary Insurance Numbers…
(Includes repeat patients)
Covered by Medicaid = 83.4%
Covered by Medicare = 15.8%
Covered by private insurance = 1.8%
No insurance = 9.9%
Patients with Medicare or Husky C and
thus are either aged or disabled = 37.5%
Preliminary Mental Health and
Substance Abuse Numbers…
Patients assigned a
mental health
diagnosis, even if not
currently experiencing
symptoms = 62.0%
Patients abusing
alcohol: 53.6%
Patients using illicit
drugs: 54.8%
Combining the alcohol
& drug numbers,
77.6% of patients were
actively abusing
alcohol or using illicit
drugs, while 22.4%
were not misusing
either.
Preliminary Medical Numbers:
(Includes repeat patients)
Patients without a Primary Care Provider upon admission
= 37.9%
Average number of Emergency Department visits during
the prior 365 days = 14.2
Most common presenting issue = Alcohol
Intoxication/Withdrawal (17.9%)
Runner-up presenting issue = Chest Pain (10.5%)
Most common chronic condition = Diabetes (16.4%)
Average number of medications prescribed at discharge
= 6.7
Preliminary Disposition Numbers…
Out of 474 discharges (includes repeat patients):
50 patients were admitted to Medical Respite (10.5%)
32 patients went to a skilled nursing facility (because their
needs were more than could be managed at Respite) (6.8%)
93 patients had family or friends willing to take them in
(19.6%)
155 patients went to standard shelter services, due to not
meeting criteria (typically due to lack of a medical need
requiring recuperation) (32.7%)
61 patients declined respite or shelter services choosing the
street instead (12.9%)
37 patients identified as homeless had a residence or
acquired housing at discharge (7.8%)
38 patients went on to other forms of care, e.g. inpatient
psychiatric or substance abuse treatment (8.0%)
8 patients could not be included, e.g. due to rapid discharge
or demise (1.7%)
Initial Impact
Average number of Emergency Department visits during
the prior 365 days = 14.2, for all screenings
12 of 26 Medical Respite patients (46%) who completed
the program returned to the Emergency Department at
least once following discharge from the program
8 of 26 patients (31%) that completed the Medical Respite
program returned to the hospital within next 30 days
Annualized rate of Emergency Department visits following
discharge from Medical Respite = 7.7 visits
Excluding our most unusual outlier patient, the annualized
rate of Emergency Department visits following discharge
from Medical Respite = 4.6
Recommendations
Comprehensive training
regarding the program and
identification/referral of
homeless patients
Thorough assessment of
patient ability and
motivation for selfcare/medical compliance
Marketing materials for
patients unfamiliar with or
reluctant to return to the
shelter
Comprehensive treatment
plan prior to discharge, with
special attention to
insurance and medications
Ongoing and open channels
of communication re:
Readmissions
Progress/obstacles
Safety issues
Weekly multi-disciplinary
team case review and
planning meetings
Thorough investment and
cooperation from home
nursing agencies
Medical review of
challenging/recurring cases
Ongoing data collection