MERCY PRESERVATION PROJECTS
advertisement

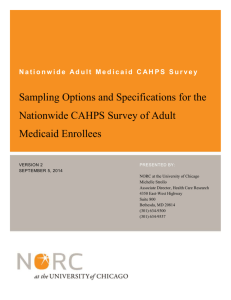
Can Health Care Savings Drive a New Funding Model For Affordable Housing? Shifts in Health Care Industry Provide Opportunity for a New Funding Model 1. Industry moving from “pay for volume” to “pay for value” 2. Shift from access to “sick care” to health care” and “well care” 3. Public Purchasers are shifting their patients to managed care plans • Capitated rates with cost savings and risk potential for health plans • Better potential for aligning costs and savings Figure 4 Medicaid Managed Care Penetration Rates by State, 2008 VT NH WA ME MT ND MA MN OR ID NY SD WI MI CT WY PA IA NE NV IL UT CA CO KS IN DE WV VA IL MO KY NC TN OK AZ NM AK MD DC SC AR MS TX NJ OH AL GA LA FL HI U.S. Average = 70% 0-50% (5 states) 51-70% (20 states including DC) 71-80% (9 states) 81-100% (17 states) Note: Unduplicated count. Includes managed care enrollees receiving comprehensive and limited benefits. 4 SOURCE: Medicaid Managed Care Enrollment as of December 31, 2008. Centers for Medicare and Medicaid Services. RI Proposed Health and Housing “Products” 1) Care Management services: generally focused on increasing services and improving outcomes for existing residents or in new properties using traditional HUD/LIHTC deal structures 2) Supportive Housing– service-enriched housing, typically for formerly homeless individuals, including seniors, veterans and/or disabled 3) Service-enriched senior housing: Unlicensed housing with support services that do not reach the level of care and supervision of assisted living or skilled nursing Funding Considerations Funding Model Options 1) Traditional approach (current): Reliant on public funding for capital, services, and operations. Health and housing integration and innovation occurs at project level with some philanthropic support 2) Fee for service (proposed approach): directly contract with a health plan or provider for a monthly fee that covers health and housing costs in an integrated payment that is not dependent on health outcomes. 3) Pay for Success: Seek contract with public agency to pay fee in return for specific outcomes (e.g.. avoided hospitalizations, lower costs, etc.). Would require partnership with investor that would pay for the upfront costs of the housing and services in return for share of savings. Factors that influence revenue potential Cost Savings Potential Access: what is the process by which residents gain access to apartments $60,000 $50,000 Annual Medicaid Expense $40,000 $30,000 Cost $20,000 $10,000 $25% 50% Alignment / Access Control 100% Alignment: Degree to which the residents are members, enrollees, patients of the health partner Potential business models Opportunity #1: Care Management • service-enriched housing communities are a platform for comprehensive health promotion and risk reduction • On-site staff can deliver targeted care coordination services in a community-based setting • Coordinators also facilitate access to residents for third party services such as health screenings • Mercy Housing has the expertise and opportunity to reach individuals who elude clinic-based case management Core Wellness Practices and Programs • Health and Wellness Interview • Preventative and Primary Health Care • Behavioral Health Care • Health Benefits Acquisition • Health Education and Risk Reduction • Food • Physical Activity • WellBeing Checks • Activates for Daily Living Screening and Support • Transition Plan to and From Hospitals/Institutions Examples of Third Party Services Coordinated by Mercy Housing • Health screenings and immunizations • Services to promote healthy pregnancies and help children with special needs • Hospice • In-home Support Services/ Adult Day Health • Food services: Meals on Wheels; Food Bank Fee-for-service senior housing Hot-spotter approach: Small percent of “high cost” individuals drive health care costs • High-cost Medicaid enrollees (over $25,000 annual spending) are 4% of all enrollees, 49% of all spending • 49% are elderly and 43% are disabled. •nursing homes or other long-term care represent 77% of cost attributable to elderly “high-cost enrollees” of Medicaid Problem: Traditional “medical” solutions are unlikely to avoid key cost drivers of highest cost enrollees • Nursing homes or other long-term care represent 77% of cost attributable to elderly “high-cost enrollees” of Medicaid •There is currently no affordable alternative to skilled nursing • Homeless individuals and other extremely low-income individuals are often difficult to treat for illness and/or discharge from hospitals because they lack stable housing and often fail to access behavioral health supports. “Market Failure” Medicaid will pay for skilled nursing or residential care facilities at three to four times the monthly cost of Mission Creek • •Medicare will pay 20X the daily cost of Mission Creek for hospital beds for patients that lack a home to be discharged to. •Once the patient’s medical needs have been met, hospitals pay the cost of “housing” the dual eligibles in their $1,000/night beds Case Study: Mission Creek Senior Community San Francisco • Service-enriched independent living alternative to nursing home beds at Laguna Honda • 50 of 140 units direct referral of SF Dept of Public Health from skilled nursing, hospitals and shelters • SF DPH pays $700/month operating subsidy for exclusive access to those units. Case Study: Mission Creek Senior Community San Francisco • Mercy’s on-site team provides a holistic “blended” approach to services and property management Service Coordination Health Education Physical Activity Transition Plans Health Interview Food banks Well-being Checks Benefits Acquisition • SF DPH also provides access to a roving team that can meet the “medical” needs of residents Study Findings: San Francisco Department of Public Health • Medicaid/Medicare costs of the 50 original DPH referrals shrank from $1.7 million per year to $253,000 • Per capita, $29,000 annual savings, Medicaid and Medicare • Savings: reduced hospitalizations and skilled nursing stays Value Proposition: Estimated Total Costs & Savings Net Savings Health care cost $65k-100k per year Impact of Independen t Long Term Care Fee Ongoing health cost Pre-Intervention With Independent Long-Term Care How else might we understand pricing? Residential Care Options low Average high 5,463 5,418 4,889 4,195 4,133 3,518 2565 2,865 2,568 2,575 1,300 Mercy LTC Model RCFE base rate - RCFE Base Rate ALWPP Rate:** Los Angeles* + Add. Services:* Skilled Nursing Skilled Nursing Facility: LA Facility: Statewide