Muscular dystrophy
advertisement
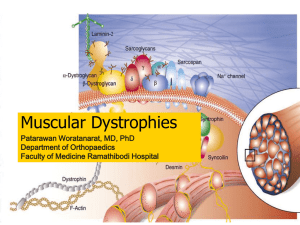
X-linked Muscular Dystrophy Sonja Li, Nancy Liu, Yu Chen Amy Sung, Michelle Tam PHM142 Fall 2014 Instructor: Dr. Jeffrey Henderson What is muscular dystrophy? Genetic disease affecting skeletal muscles Characterized by progressive muscle weakness and wasting, and loss of motor skills X-linked recessive most common: Duchenne and Becker More than 1 in 3500 males born Onset age from infancy to adulthood Most end up wheelchair-bound Duchenne muscular dystrophy Most common type: 1 in 3500 Early onset: signs appear before 6 years of age Delayed development of motor skills Weakness/fatigue Difficulty in keeping balance Pseudohypertrophy Contractures Wheelchair dependent by ~12 years of age DMD - Gower Maneuver Becker muscular dystrophy Milder form of Duchenne 1 in 18,518 males Onset age: 5 to 15 years of age Loss of muscle mass and motor skills Weakness/fatigue Pseudohypertrophy Contractures Wheelchair dependent by 25-30 Other Conditions Caused Scoliosis Cardiac Dilated cardiomyopathy Arrhythmia Shortness of breath and fatigue Respiratory Curvature due to contractures and muscle weakness Progressive weakening of the diaphragm Cognitive (non-progressive) Dystrophin Predominant DMD transcript in striated muscle Gene mutations, deletions or duplications result in a loss of expression Rod shaped, cytoplasmic Forms dystrophin-glycoprotein complex (DGC) http://upload.wikimedia.org/wikipedia/commons/6/64/PBB_Protein_DMD_image.jpg Dystrophin Domains C-terminal end Cysteine rich domain Links to glycoprotein complex Central rod-like domain Triple α-helical coiled-coil N-terminal actin binding domain Dystrophin-Glycoprotein Complex • Serves as a link b/w extracellular matrix and subsarcolemmal cytoskeleton • Protects the sarcolemma against stress during muscle contraction or stretch • Dystroglycan: interacts with Cys-rich domain and EC matrix • Syntrophin: directly binds to dystrophin C-terminus • Sarcoglycan complex: subcomplex of four single transmembrane glycoproteins Normal Muscle Duchenne Muscular Dystrophy • Degeneration in DGC leads to tearing of sarcolemma, causing a disturbance in CK and Ca2+ concentrations Causes of Muscular Dystrophy Muscular dystrophy = mutation of DMD gene Inability to produce functional dystrophin protein Constant muscle contraction and relaxation → weaken + destroy muscles Two types of muscular dystrophy 1. Becker muscular dystrophy – inability to produce functional dystrophin Dystrophin – not 100% non-functional Limited function → less severe 2. Duchenne muscular dystrophy – inability to produce dystrophin No dystrophin production/production of only non-functional dystrophin No function → more severe Causes of Muscular Dystrophy Main cause = parents X-linked disease – caused by mutation in X-chromosome Inherited Recessive mutations Females affected only if both X-chromosomes mutated Single mutation = enough functional dystrophin produced Usually from parents unaffected → carrier of disease Double mutation = affected, but unlikely Males – single X-chromosome Mutation in X-chromosome = no dystrophin production Inheritance of Muscular Dystrophy Unaffected carrier mother + unaffected father Mother = 1 mutated X-chromosome + 1 normal X-chromosome Father = 1 normal X-chromosome + 1 normal Y-chromosome 1. Unaffected female 2. Carrier female Normal X-chromosome from father + mutated X-chromosome from mother Normal X-chromosome = enough functional dystrophin produced 3. Unaffected male http://mda.org/sites/default/files/X-linkedrecessive_chart.jpg Normal X-chromosome from mother + normal X-chromosome from father Normal X-chromosome from mother + normal Y-chromosome from father 4. Affected male Mutated X-chromosome from mother + normal Y-chromosome from father No normal X-chromosome = no dystrophin production Diagnosis Blood Creatine phosphokinase (CPK) test Electromyography (EMG) Measuring electric signaling to and from the muscle can rule out neurodegenerative diseases and confirm a muscle disease. Muscle biopsy Damaged muscles can release creatine kinase into blood. Elevated levels signify muscle injury: trauma or muscular dystrophy. The microscopic analysis of a sample of muscle tissue can identify presence of muscular dystrophies and its form. Genetic testing Testing of mutations in muscular dystrophy related genes can determine the exact form of muscular dystrophy. Therapies for Muscular Dystrophy Physical therapy Respiratory therapy Monitor respiratory conditions Occupational therapy Physical and stretching exercises help keep muscles flexible and strong Teach use of assistive devices eg. wheelchairs Corrective surgery For certain conditions from muscular dystrophy eg. pacemaker for myotonic muscular dystrophy or heart problems Drug therapy for Duchenne Muscular Dystrophy No known cure Drugs effective only in transiently alleviating the symptoms, delaying muscle degeneration and increasing force of strength Two most common are corticosteroids: deflazacort and prednisone Both suppress the body’s immune system and release substances which cause inflammation Mechanisms unknown Prednisone Common dose is 0.75 mg/kg of body weight per day Increases utrophin and dystrophin protein expression in some dystrophic muscles to increase muscle strength Helps increase number of regenerating fibers after injury of skeletal muscle (prone to occur in patients with DMD) By increasing myoblast and myotube density as well as number of proliferating myoblasts General effect: loss of ambulation postponed to mid-teens or twenties and better preservation of respiratory and cardiac function Side effects: weight gain, rounded face (Cushingoid appearance), acne, cataracts, GI symptoms and behavioural changes X-Linked Muscular Dystrophy Summary Overview Duchenne and Becker muscular dystrophy: most common forms of muscular dystrophy; affects skeletal muscles and cardiac muscles, leading to their degeneration. Signs and symptoms include: muscle weakness, loss of muscle coordination and balance, pseudohypertrophy, contractures, and Gower’s sign. Duchenne is more severe, with earlier onset age and quicker progression, while Becker is like a milder form of Duchenne. Affected patients gradually loses muscle mass and mobility, end up wheelchair bound and have increased motility Other conditions caused as a consequence of Duchenne and Becker: Scoliosis, Dilated cardiomyopathy, respiratory complications, and cognitive impairments (which unlike other symptoms, is non-progressive) Dystrophin Mutations, deletions or duplications of the dystrophin gene most frequently result in a loss of dystrophin expression in muscle of patients afflicted with DMD Consists of 4 domains: C-terminal end – binds to syntrophin Cysteine rich domain – links the cytoskeleton to the extracellular matrix via the membrane with dystrophin-associated glycoprotein, dystroglycan Central rod-like domain – made from a triple α-helical coiled-coil N-terminal actin binding domain (very short) Dystrophin works to protect the sarcolemma against stress through a dystrophin-glycoprotein complex Includes dystroglycan, syntrophin, and sarcoglycan complex Degeneration in DGC leads to tearing of sarcolemma, causing a disturbance in CK and Ca2+ concentrations Causes Muscular dystrophy = recessive genetic mutation in X-chromosome → inherited from parents (most likely mother) Females – affected if only both X-chromosomes mutated → far less likely to have dystrophy Males – single mutation required (only one X-chromosome) → most cases of muscular dystrophy are males Diagnosis Ways to diagnose muscular dystrophy include: Blood Creatine phosphokinase/CPK test, EMG test, biopsy, and genetic testing, which is most specific and non-invasive Treatment Various therapies available to alleviate symptoms of muscular dystrophy include physical, respiratory, speech, occupational and drug therapies. Drug treatments for Duchenne Muscular Dystrophy: There is no known cure – medication only helps to alleviate symptoms and delay muscle degeneration Most common drug used is prednisone, which is a corticosteroid Active form is prednisolone Prednisone: Increases utrophin and dystrophin protein expression in some dystrophic muscles – increases muscle strength Helps increase number of regenerating fibers after injury of skeletal muscle by increasing myoblast and myotube density as well as number of proliferating myoblasts General effect: loss of ambulation postponed to mid-teens or twenties and better preservation of respiratory and cardiac function Side effects: weight gain, rounded face (Cushingoid appearance), acne, cataracts, GI symptoms and behavioural changes References Angelini, C., & Peterle, E. (2013). Old and new therapeutic developments in steroid treatment in Duchenne muscular dystrophy.Acta Myologica, 31(1), 9-15. Baltgalvis, K., Call, J., Nikas, J., & Lowe, D. (2009). The effects of prednisolone on skeletal muscle contractility in mdx mice.Muscle & Nerve, 40(3), 443-454. Becker Muscular Dystrophy. Muscular Dystrophy Canada. Retrieved from http://www.muscle.ca/fileadmin/National/Muscular_Dystrophy/Disorders/Becker_E.pdf Beenakker, E., Fock, J., Van Tol, M., Maurits, N., Koopman, H., Brouwer, O., & Van der Hoeven, J. (2005). Intermittent Prednisone Therapy in Duchenne Muscular Dystrophy: A Randomized Controlled Trial.Archives of Neurology, 62, 128-132. Campellone, J.V. (2014). Becker Muscular Dystrophy. Medline Plus. Retrieved from http://www.nlm.nih.gov/medlineplus/ency/article/000706.htm Calvo, S, et al (2012, February). DMD-associated dilated cardiomyopathy. Genetics Home Reference 2014. Retrieved from http://ghr.nlm.nih.gov/condition/dmd-associated-dilated-cardiomyopathy Calvo, S, et al (2012, February). Duchenne and Becker Muscular Dystrophy. Genetics Home Reference. Retrieved from http://ghr.nlm.nih.gov/condition/duchenne-and-becker-muscular-dystrophy Causes/Inheritance. Muscular Dystrophy Association 2014. Damon, S., et al (2007). Prevalence of Duchenne/Becker Muscular Dystrophy Among Males Aged 5--24 Years --- Four States, 2007. Centres for Disease Control and Prevention. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5840a1.htm Ervasti, J. M. Structure and Function of the Dystrophin-Glycoprotein Complex. Madame Curie Bioscience Database 2000. Haldeman-Englert (2014). Duchenne Muscular Dystrophy. Medline Plus. Retrieved from http://www.nlm.nih.gov/medlineplus/ency/article/000705.htm Learning about Duchenne Muscular Dystrophy (2013, April 18). National Human Genome Research Institute. Retrieved from http://www.genome.gov/19518854 Merlini, L., Cicognani, A., Malaspina, E., Gennari, M., Gnudi, S., Talim, B., & Franzoni, E. (2003). Early prednisone treatment in Duchenne muscular dystrophy. Muscle & Nerve, 27, 222-227. Muscular Dystrophy (1995). Cleveland Clinic. Retrieved from http://my.clevelandclinic.org/health/diseases_conditions/hic_muscular_dystrophy Nicolas, A. et al. Becker muscular dystrophy severity is linked to the structure of dystrophin. Human Molecular Genetics 2014; 23: 1-13. Signs and Symptoms of Muscular Dystrophy. MDA. Retrieved from http://mda.org/disease/duchenne-muscular-dystrophy/signs-and-symptoms Signs of Duchenne. Parent Project Muscular Dystrophy. Retrieved from http://www.parentprojectmd.org/site/PageServer?pagename=understand_about_signs Straub, V., & Campbell, K. P. Muscular dystrophies and the dystrophin-glycoprotein complex. Current Opinion in Neurology 1997; 10: 168-175. What are the treatments for muscular dystrophy? (2012, November 11). Retrieved November 16, 2014, from http://www.nichd.nih.gov/health/topics/musculardys/conditioninfo/Pages/treatment.aspx