presentation
advertisement
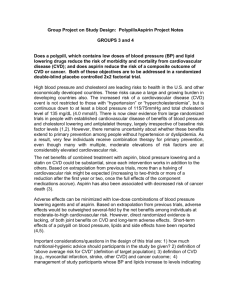
Development and Pilot Testing of a Non-Physician Healthcare Worker Training Curriculum for the Assessment and Management of Cardiovascular Disease Maheer Khan M.Sc. 2014-05-28 Outline • Global Burden of Cardiovascular Disease • Evidence for Task Shifting in Cardiovascular disease management • HOPE-4 Program • Package of Interventions • Training Curriculum • Phases of Development • Pilot Process • Contextual Adaptability • Our Experience • Next Steps - Policy Implications Global Burden of NCDs • Non-communicable diseases (NCDs) caused an estimated 35 million deaths in 2005 • Four major NCDs – CVD, cancer, chronic respiratory disease and diabetes – together are responsible for 28 million deaths a year and make the largest contribution to the NCD burden in low and middle income countries (LMIC) • 60% of all deaths globally are NCDs • 80% of NCD deaths occur in low and middle income countries (WHO 2010) CVD Mortality NCD Global Monitoring Framework • In 2011, WHO developed a global monitoring framework to enable global tracking of NCDs • The mortality target – a 25% reduction in premature mortality from NCDs by 2025 • Mortality target cannot be achieved without reducing the global burden of CVD in LMIC • Currently, most LMIC do not have systematic approaches for screening • Task-shifting to non-physician healthcare workers is one potential solution Evidence for Task Shifting • Task shifting: the rational re-distribution of tasks between health care workers • Basic management of chronic diseases can be shifted to Non-Physician Healthcare Worker (with physician oversight), with improved outcomes. – Callaghan et al., 2010 – Lekoubou et al., 2010 • Supported by WHO Task Shifting-Global Recommendations and Guidelines • Joint development of a WHO/PHRI curriculum for training NPHW in the assessment and management of CVD Heart Outcomes Prevention and Evaluation (HOPE-4) Program • Objective: Implement a programme for CVD risk assessment and management in select low and middle income countries • 190 rural and urban communities (10 000 participants) in Asia (India, Malaysia, Philippines), South America (Colombia, Argentina), and Sub-Saharan Africa (South Africa, Tanzania, Rwanda). • Package of Interventions: – Task shifting to teams of NPHWs using the HOPE-4 Training Curriculum – The Polycap (low cost, fixed dose, combination CV medications (4-5 pills in one) ($5/month) – Mobile phone technology-text messages* – Non-Professional Treatment Supporters* *To improve adherence to medication and lifestyle modifications HOPE-4 Training Curriculum • Developed in response to limitations in other CVD training curriculum – WHO’s CVD Risk Management Package – WHO’s Package of Essential NCD interventions • Interdisciplinary team • Participation of Stakeholders - Ministry of Health (Malaysia) - Ministry of Public Health (Columbia) Curriculum Development • Phase 1: Defining the Need – Standardization – Defining the ‘fixed’ and ‘adaptable’ elements • Phase 2: Improving Guidelines – Multiple Blood Pressure Readings – Empowering NPHWs – Cultural Adaptability • Phase 3: Understanding Task Shifting in a Global Context – Legal and Ethical Implications – Experience from HIV/AIDS programs Phase 4: Defining NPHW Roles and Responsibilities NPHW Roles and Responsibilities 1. Understanding risk factors to CVD such as hypertension, diabetes and high blood pressure 2. Expressing competency in assessing risk and potential consequences of high risk of CVD 3. Showing proficiency with skills relevant to managing and preventing CVD such as measuring blood pressure and the waist/hip ratio 4. Providing culturally relevant and appropriate counseling 5. Serving as a link between academic researchers and the communities 6. Developing the ability to appropriately conduct patient interviews and counsel them on lifestyle modifications such as smoking cessation, diet and physical activity. 7. Prescribing treatment regimens with physician oversight 8. Developing the ability to accurately record and organize patient data Phase 5: Curriculum Design • Curriculum Content • Trainer Manual • Workbooks for NPHW • 9 Modules delivered over 1 week • Pre-post module tests Module Descriptions Module 1. Health and Disease Objective(s) Define the concepts of health & disease 2. Organization and Communication Skills Understand importance of these skills 3. The Cardiovascular System Understand the basics of the CV system 4. Risk Factors for Cardiovascular Disease Understand the common CVD risk factors 5. Cardiovascular Risk Assessment Assess overall CVD risk 6. Cardiovascular Risk Prevention and Treatment Learn counseling techniques for behavioural modification 7. Pharmacological Management of Cardiovascular Disease 8. HOPE-4 Program Specific Training Understand the basics of how different drugs are used to manage CVD Understand the role of an NPHW 9. Observed Standardized Clinical Exam of NPHWs Successfully complete all scenarios Phase 6: Developing the OSCE • Preferred method of evaluation in clinical exams* • Advantages of this approach • Challenges we faced in developing the OSCE • Evaluation *(Zayyan,2011) Sample OSCE Scenario Information for NPHW: For this practice scenario, you will need to counsel a participant on alcohol consumption. The participant is a 56 year old and admits to drinking 10 beers per day. Standardized Participant Instructions: You are a 56 year old participant who consumes over 10 beers per day. You want to cut back and you realize that your drinking is negatively impacting your health. Marking Scheme NPHW evaluated using a checklist and marked out of seven Pilot Sessions • Recruitment of local ‘NPHWs’ and instructor • Curriculum was delivered in its entirety over 5 sessions, 3.5 hours each • Objective of the sessions – Determine areas of confusion, inconsistency and misinterpretation • Evaluation – NPHWs required to pass all pre/post module tests and OSCE scenarios – Successful completion means NPHWs are trained to go out in the field Contextual Adaptability • Adaptable elements of the curriculum – Legal roles of NPHW – Cultural differences (Columbia and Malaysia experience) – Teaching styles • Patient centered approach – Role playing and discussion activities – Use of standardized patients Our Experience • Lessons Learned: – – – – Interdisciplinary team was an advantage Difficulties in gauging cultural sensitivities Re-testing of NPHWs NPHW and instructor recruitment bias • What we would do differently: – – – – More active involvement of local stakeholders Summarize and re-iterate NPHW roles Better documentation of development process More objective evaluations Next Steps – Policy Implications • Feedback from pilot sessions used to further refine the curriculum • Curriculum has been translated to Spanish and Malay (April 2014) • HOPE-4 in Canada – Aboriginal populations – Low SES groups • Success of HOPE-4 could be used to tackle regulatory barriers preventing re-distribution of tasks in existing health systems