Empiric Therapy Directed Against MRSA in Patients Admitted to the Intensive Care Unit Does Not Improve
Outcomes in Community-Acquired Pneumonia
Allen T. Griffin MD, Paula Peyrani MD, Timothy L. Wiemken PhD, Julio A. Ramirez MD, and Forest W. Arnold MD
Division of Infectious Diseases, University of Louisville
ABSTRACT
Background:
The Infectious Diseases Society of America has
recommended empiric therapy active against methicillin-resistant
Staphylococcus aureus (MRSA) for all community-acquired pneumonia
patients admitted to the intensive care unit. However, since there is
sparse data to support this recommendation, the objective of the
current study was to ascertain if such a practice improves outcomes.
Methods: This study was a secondary, retrospective analysis of the
Community-Acquired Pneumonia Organization international database.
Outcomes in patients admitted to the intensive care unit with
community-acquired pneumonia were compared based on empiric
initiation of anti-MRSA therapy (vancomycin or linezolid) with standard
therapy or standard therapy alone.
Results: A total of 621 patients were identified with intensive care
pneumonia, with 57 patients having been initiated empirically on
vancomycin or linezolid. In-hospital and 28-day mortality, as well as
hospital length of stay and time to clinical stability, were not statistically
different in the vancomycin and linezolid group compared to the
standard group.
Conclusions: These findings suggest empiric MRSA therapy in all
intensive care community-acquired pneumonia patients is unnecessary
and argue for local epidemiologic data on the prevalence of MRSA to
guide use of anti-MRSA therapy.
INTRODUCTION
Community-associated methicillin-resistant Staphylococcus aureus
(CA-MRSA) has become an increasingly recognized etiology of
community-acquired pneumonia.1 MRSA has historically been limited to
those who were chronically ill, had exposure to a healthcare
environment, or were previously infected with influenza viruses, but
these associations have become less apparent as MRSA is being
found in otherwise healthy young adults.2-4 Characteristic features that
may alert clinicians to the presence of MRSA pneumonia are cavitation
in the setting of acute pneumonia or the presence of empyema,
multilobar involvement, hemoptysis, or leukopenia.5,6 However, given
the lack of specificity of these findings and the potentially severe nature
of this illness, the Infectious Diseases Society of America has recently
recommended empiric therapy against CA-MRSA (vancomycin or
linezolid) in all patients with severe community-acquired pneumonia as
defined by intensive care admission, empyema, or necrotizing
pneumonia.7 Some evidence suggests that a delay in initiation of
therapy against confirmed CA-MRSA in pneumonia patients increases
the chances of suboptimal outcomes.5 However, it remains unclear
from such evidence if empiric therapy directed against CA-MRSA in all
patients with severe pneumonia will improve outcomes. As a result, the
objective of the present study was to compare outcomes in patients
with severe community-acquired pneumonia defined by intensive care
admission who were initiated on empiric MRSA therapy (vancomycin or
linezolid) to those who were not initiated on empiric MRSA therapy.
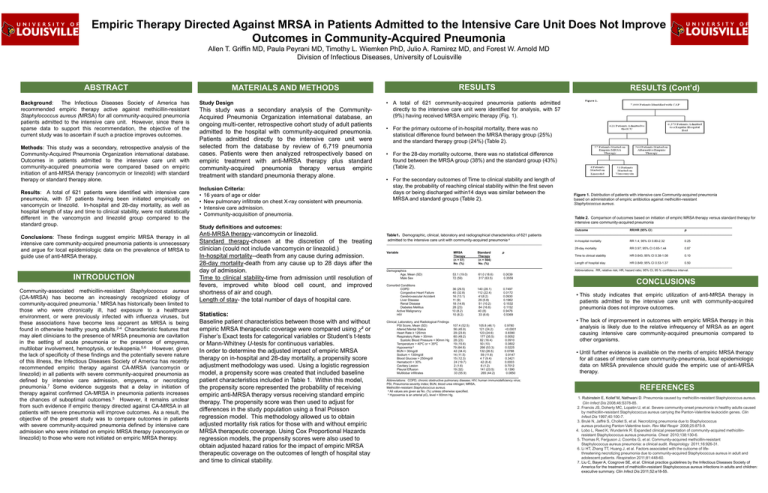
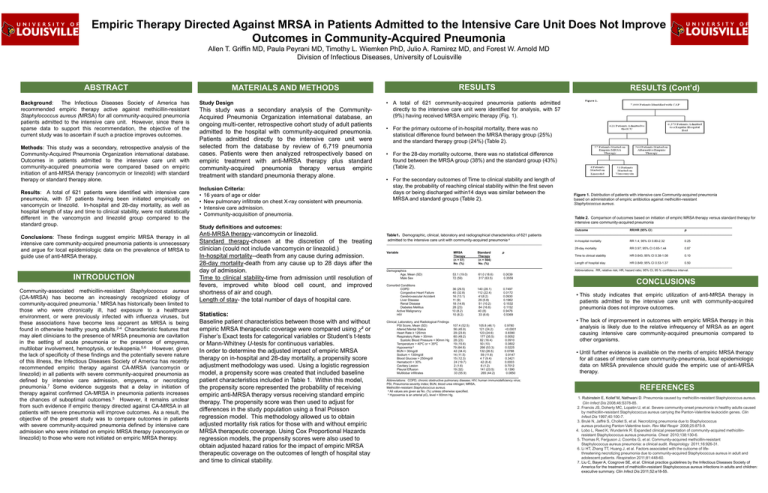
RESULTS
MATERIALS AND METHODS
Study Design
This study was a secondary analysis of the CommunityAcquired Pneumonia Organization international database, an
ongoing multi-center, retrospective cohort study of adult patients
admitted to the hospital with community-acquired pneumonia.
Patients admitted directly to the intensive care unit were
selected from the database by review of 6,719 pneumonia
cases. Patients were then analyzed retrospectively based on
empiric treatment with anti-MRSA therapy plus standard
community-acquired pneumonia therapy versus empiric
treatment with standard pneumonia therapy alone.
Inclusion Criteria:
• 16 years of age or older
• New pulmonary infiltrate on chest X-ray consistent with pneumonia.
• Intensive care admission.
• Community-acquisition of pneumonia.
RESULTS (Cont’d)
• A total of 621 community-acquired pneumonia patients admitted
directly to the intensive care unit were identified for analysis, with 57
(9%) having received MRSA empiric therapy (Fig. 1).
• For the primary outcome of in-hospital mortality, there was no
statistical difference found between the MRSA therapy group (25%)
and the standard therapy group (24%) (Table 2).
• For the 28-day mortality outcome, there was no statistical difference
found between the MRSA group (38%) and the standard group (43%)
(Table 2).
• For the secondary outcomes of Time to clinical stability and length of
stay, the probability of reaching clinical stability within the first seven
days or being discharged within14 days was similar between the
MRSA and standard groups (Table 2).
Table 2. Comparison of outcomes based on initiation of empiric MRSA therapy versus standard therapy for
intensive care community-acquired pneumonia
Study definitions and outcomes:
Anti-MRSA therapy-vancomycin or linezolid.
Standard therapy-chosen at the discretion of the treating
clinician (could not include vancomycin or linezolid.)
In-hospital mortality--death from any cause during admission.
28-day mortality-death from any cause up to 28 days after the
day of admission.
Time to clinical stability-time from admission until resolution of
fevers, improved white blood cell count, and improved
shortness of air and cough.
Length of stay- the total number of days of hospital care.
Statistics:
Baseline patient characteristics between those with and without
empiric MRSA therapeutic coverage were compared using ² or
Fisher’s Exact tests for categorical variables or Student’s t-tests
or Mann-Whitney U-tests for continuous variables.
In order to determine the adjusted impact of empiric MRSA
therapy on in-hospital and 28-day mortality, a propensity score
adjustment methodology was used. Using a logistic regression
model, a propensity score was created that included baseline
patient characteristics included in Table 1. Within this model,
the propensity score represented the probability of receiving
empiric anti-MRSA therapy versus receiving standard empiric
therapy. The propensity score was then used to adjust for
differences in the study population using a final Poisson
regression model. This methodology allowed us to obtain
adjusted mortality risk ratios for those with and without empiric
MRSA therapeutic coverage. Using Cox Proportional Hazards
regression models, the propensity scores were also used to
obtain adjusted hazard ratios for the impact of empiric MRSA
therapeutic coverage on the outcomes of length of hospital stay
and time to clinical stability.
Figure 1. Distribution of patients with intensive care Community-acquired pneumonia
based on administration of empiric antibiotics against methicillin-resistant
Staphylococcus aureus.
Table1. Demographic, clinical, laboratory and radiographical characteristics of 621 patients
admitted to the intensive care unit with community-acquired pneumonia a
___________________________________________________________________________________________________________________________
MRSA
Standard
p
Therapy
Therapy
(n = 57)
(n = 564)
No. (%)
No. (%)
____________________________________________________________________________________________
Demographics
Age, Mean (SD)
53.1 (19.0)
61.0 (18.6)
0.0039
Male Sex
72 (59)
317 (63.5)
0.3559
_____________________________________________________________________________________________
Outcome
RR/HR (95% CI)
p
_____________________________________________________________________________________________
In-hospital mortality
RR 1.4; 95% CI 0.80-2.32
0.25
28-day mortality
RR 0.97; 95% CI 0.65-1.44
0.87
Time to clinical stability
HR 0.643; 95% CI 0.38-1.08
0.10
Variable
Comorbid Conditions
COPD
Congestive Heart Failure
Cerebrovascular Accident
Liver Disease
Renal Disease
Diabetes Mellitus
Active Malignancy
HIV
36 (29.5)
40 (32.8)
16 (13.1)
11 (9)
18 (14.8)
28 (23)
10 (8.2)
10 (8.2)
140 (28.1)
112 (22.4)
41(8.2)
29 (5.8)
51 (10.2)
84 (16.8)
40 (8)
33 (6.6)
0.7497
0.0172
0.0930
0.1962
0.1532
0.1152
0.9476
0.5369
Clinical, Laboratory, and Radiological Findings
PSI Score, Mean (SD)
107.4 (52.5)
105.8 (46.1)
0.9780
Altered Mental Status
56 (45.9)
121 (24.2)
<0.0001
Heart Rate ≥ 125/min
29 (23.8)
123 (24.6)
0.8390
Respiratory Rate > 30/min
60 (49.2)
177 (35.5)
0.0052
Systolic Blood Pressure < 90mm Hg 28 (23)
82 (16.4)
0.0910
Temperature > 40ºC or < 35ºC
19 (15.6)
50 (10)
0.0802
b
Hypoxemia
79 (64.8)
266 (53.3)
0.0225
BUN > 30mg/dl
42 (34.4)
132 (26.5)
0.0788
Sodium < 130mg/dl
14 (11.5)
59 (11.8)
0.9147
Blood Glucose > 250mg/dl
15 (12.3)
4 7 (9.4)
0.3421
Hematocrit < 30%
24 (19.7)
42 (8.4)
0.0003
Cavitary Lesion
2 (1.6)
6 (1.2)
0.7012
Pleural Effusion
19 (32)
141 (23.5)
0.1390
Multilobar infiltrates
33 (55.9)
265 (44.2)
0.0850
______________________________________________________________________________
Abbreviations: COPD, chronic obstructive pulmonary disease; HIV, human immunodeficiency virus;
PSI, Pneumonia severity index; BUN, blood urea nitrogen; MRSA,
Methicillin-resistant Staphylococcus aureus.
a All values are given as No. (%) unless otherwise specified.
b Hypoxemia is an arterial pO₂ level < 60mm Hg.
Length of hospital stay
HR 0.849; 95% CI 0.53-1.37
0.50
_____________________________________________________________________________________________
Abbreviations: RR, relative risk; HR, hazard ratio; 95% CI, 95 % confidence interval.
CONCLUSIONS
• This study indicates that empiric utilization of anti-MRSA therapy in
patients admitted to the intensive care unit with community-acquired
pneumonia does not improve outcomes.
• The lack of improvement in outcomes with empiric MRSA therapy in this
analysis is likely due to the relative infrequency of MRSA as an agent
causing intensive care community-acquired pneumonia compared to
other organisms.
• Until further evidence is available on the merits of empiric MRSA therapy
for all cases of intensive care community-pneumonia, local epidemiologic
data on MRSA prevalence should guide the empiric use of anti-MRSA
therapy.
REFERENCES
1. Rubinstein E, Kollef M, Nathwani D. Pneumonia caused by methicillin-resistant Staphylococcus aureus.
Clin Infect Dis 2008;46:S378-85.
2. Francis JS, Doherty MC, Lopatin U, et al. Severe community-onset pneumonia in healthy adults caused
by methicillin-resistant Staphylococcus aureus carrying the Panton-Valentine leukocidin genes. Clin
Infect Dis 1997;40:100-7.
3. Brulé N, Jaffré S, Chollet S, et al. Necrotizing pneumonia due to Staphylococcus
aureus producing Panton-Valentine toxin. Rev Mal Respir 2008;25:875-9.
4. Lobo L, Reed K, Wunderink R. Expanded clinical presentation of community-acquired methicillinresistant Staphylococcus aureus pneumonia. Chest 2010;138:130-6.
5. Thomas R, Ferguson J, Coombs G, et al. Community-acquired methicillin-resistant
Staphylococcus aureus pneumonia: a clinical audit. Respirology 2011;16:926-31.
6. Li HT, Zhang TT, Huang J, et al. Factors associated with the outcome of lifethreatening necrotizing pneumonia due to community-acquired Staphylococcus aureus in adult and
adolescent patients. Respiration 2011;81:448-60.
7. Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the Infectious Diseases Society of
America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children:
executive summary. Clin Infect Dis 2011;52:e18-55.